A 63-year-old woman with no personal or family background of interest presented a 13-month history of a skin rash formed of papules that coalesced into pruritic plaques affecting the upper third of the back, with no involvement of the limbs or face or of the mucosas. She had previously been treated for 2 months with topical corticosteroids by her family physician, with no response.
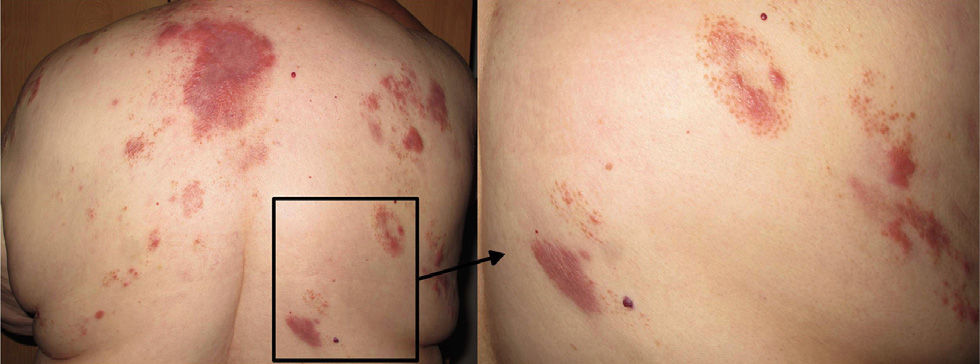
Physical ExaminationPhysical examination revealed a predominantly follicular erythematous papules and more extensive plaques with a moderate degree of infiltration on the upper half of the back (Fig. 1). There were no palpable locoregional lymph nodes and no hepatosplenomegaly.
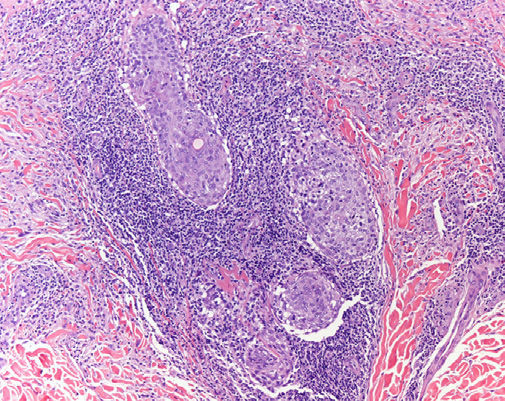
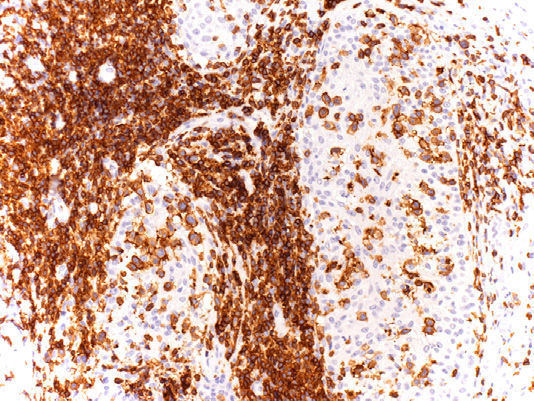
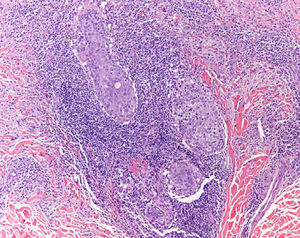
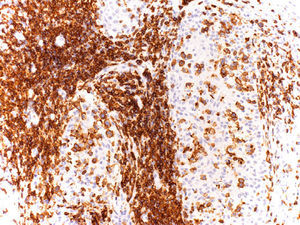
HistologyOn histopathology, the dermis was infiltrated by a lymphoproliferative process with a perivascular and periadnexal distribution and with minimal epidermal involvement (Fig. 2). The hair follicles presented a lymphoproliferative infiltrate, with the presence of mucin that stained intensely positive with Alcian blue at pH 2.5. Immunohistochemistry was positive for CD3 (Fig. 3), CD5, and CD7, with deletion of CD2 and partial deletion of CD4. The proliferating cells were negative for CD30, CD56, TIA-1, perforin, and granzyme B. Molecular study showed clonal rearrangement of the gamma chain of the T-cell receptor.
Additional TestsThe results of the metastatic work-up (complete blood count, general biochemistry, lactate dehydrogenase, β2-microglobulin, bone marrow aspiration biopsy, protein electrophoresis, and positron emission tomography-computed tomography) were within normal limits.
What Is Your Diagnosis?
DiagnosisFollicular mycosis fungoides.
Clinical Course and TreatmentBased on the findings of the histology study and additional tests, we made a diagnosis of stage IB (T2b, N0, M0, B0) mycosis fungoides. The case was presented to the Skin Oncology Committee and it was decided to start treatment with psoralen-UV-A (PUVA) therapy following the standard protocol. Little improvement was achieved at the 3-month follow-up and the patient remains pending further evaluation of other treatment options.
CommentFollicular mycosis fungoides is a variant of mycosis fungoides characterized by the presence of follicular infiltrates that tend mainly to affect the head and neck. It was first described by Kim in 1985, who reported cases of mycosis fungoides limited to the hair follicles and perifollicular dermis. This variant accounts for 10% of cases of MF.1
From an epidemiologic point of view, there appear to be no differences between the sexes, although there is a slight predominance in adult men. The age at presentation does not differ from that of classic mycosis fungoides.
The etiology and pathogenesis are not fully understood. It has been postulated that the epithelium of the hair follicles may express higher levels of skin-selective lymphocyte receptors (skin-selective homing) and epidermal adhesion molecules.2 Hodak et al.3 described the selective expression of intercellular adhesion molecule 1 on the cell membranes of the follicular epithelium in follicular mycosis fungoides lesions.
The disease presents clinically as follicular papules, plaques with follicular accentuation, or cysts and comedones. Although single lesions have been reported in some patients, it is more common to observe multiple plaques. Presentation in the form of tumors, pseudotumors, or erythroderma is rare. Alopecia is common when the scalp is affected. Pruritus occurs frequently, and in 68% of patients requires specific treatment.
Histopathology usually shows a dermal infiltrate with a perivascular and adnexal distribution, with infiltration of the follicular epithelium by atypical lymphocytes of follicular size and with cerebriform nuclei. There may be associated follicular mucinosis, although this is not a constant finding, and syringotropism and even squamous syringometaplasia. Five different basic patterns are recognized: the classic pattern, with or without associated follicular mucinosis; the eosinophilic folliculitis-like pattern; the cystic pattern; the basaloid pattern; and the granulomatous pattern.4
On immunohistochemistry, the neoplastic T lymphocytes are CD3+, CD4+, and CD8−, and scattered CD30+ cells may be observed. The presence of more than 15% of CD30+ or CD30− blast cells is considered a poor prognostic factor. Follicular mycosis fungoides is actually thought to have a poorer prognosis, behaving in a similar or equivalent manner to classic tumor-stage mycosis fungoides (stage IIB).5
Electron beam radiation is considered to be a more effective treatment than skin-targeting therapies such as PUVA and the topical nitrogen mustards. Some authors propose a more conservative approach using UV-A and bexarotene as the initial option.6,7 Isolated cases have shown a good response to isotretinoin, chlorambucil, radiotherapy, and interferon alfa, although the responses have usually been transitory.4
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ruiz-Villaverde R, Pérez-López I, Aneiros-Fernández J. Pápulas foliculares y placas eritematosas en espalda. Actas Dermosifiliogr. 2016;107:519–520.