Physicians are exposed to a series of occupational risk factors, of which musculoskeletal problems are among the most noteworthy. Musculoskeletal problems can lead to both acute and chronic neck and low back pain. They can also become disabling, are one of the main reasons for sick leave, and account for considerable consumption of health care resources.1 A high percentage of physicians and surgeons may be affected by symptoms,1–3 mainly chronic neck and low back pain. While data on prevalence of these conditions among dermatologists are scarce, the prevalence of musculoskeletal symptoms has been reported to be between 30% and 50%, especially those associated with poor posture.4,5 We were unable to find recommendations on appropriate posture for dermatologists performing clinical examinations and dermatoscopy.
Various studies have shown how repetition and maintenance of some postures and body movements lead to degeneration of the joints responsible for stabilizing the spinal column, and often additional complications such as chronic bone and muscle pain.6 Some of these movements can damage the intervertebral discs, cause ligament strain, and reduce the diameter of the intervertebral foramina.7
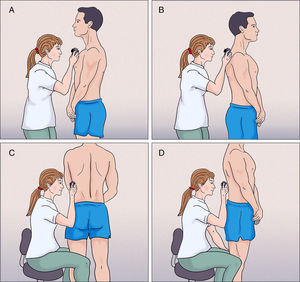
Joint movements that are advised against include any posture or gesture that requires unvarying, forced movements that overload joint structures and are systematically repeated.8 Some of these movements are observed daily in dermatologists who perform physical examinations. They take the form of trunk hyperflexion that may involve rotation, as well as cervical hyperextension or hyperflexion (Fig. 1). Therefore, the risk of lesions is not only associated with weight or sudden effort, but also with the adoption of specific postures. Given the high caseloads in our health centers, it is not uncommon for a dermatologist to perform 10-15 physical examinations per day in patients with a high number of pigmented lesions or a history of multiple skin tumors.
Education about posture should play a key role in preventing the development of lesions in daily clinical practice. Therefore, we should try to ensure a neutral, well-balanced posture with the muscles relaxed. Postures that do not respect the natural curves of the spinal column overload its joint structures. We should also adapt our workplace furniture and fittings to prevent forced postures.9 In this article, we propose a routine for performing clinical examinations and dermatoscopy based on good posture.
Furthermore, carrying out a physical examination systematically and meticulously can help to prevent omissions and delays in the diagnosis of lesions in areas that are difficult to examine, such as the scalp or the soles.10,11
Our proposal for clinical examination and dermatoscopy in adult patients requires few specific items of furniture, since we have a stool (preferably a swivel chair with wheels and a backrest) and a stretcher. We can summarize our algorithm in the following successive steps:
- -
Patient standing: The upper third of the trunk is examined (Fig. 2A and B). If the patient is of a similar height to the dermatologist, then we can also examine facial and cervical lesions.
- -
Patient standing: The doctor sits on a stool and can therefore examine the abdominal and suprapubic areas more comfortably. The patient is then asked to turn his/her trunk towards the doctor so that the flanks, lower back, and buttocks can be examined (Fig. 2C and D). We believe that examination in this position is more comfortable than the alternative, ie, the patient in supine decubitus, since we can comfortably examine the lower back and buttocks through 360°, thus obviating the need for the doctor to bend over too far.
- -
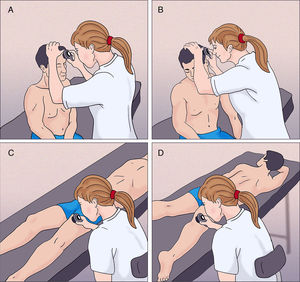
Patient sitting on the stretcher: If the patient is tall, we can explore facial lesions, since the patient is in our line of vision, and we can perform the examination comfortably (Fig. 3A). We can take advantage of this position to perform a full examination of the scalp and pinnae (fig. 3B).
- -
Patient in supine decubitus on the stretcher: While the doctor remains seated on the stool, the anterior surface of the thighs, legs, and dorsum of the feet are examined (Fig. 3C). It is better if the stretcher is situated in such a way that the doctor can move around it and thus examine both sides of the patient more comfortably.
- -
Patient in prone decubitus on the stretcher: With the patient in this condition, the doctor can examine the posterior surface of the thighs, legs, and the soles of the feet (Fig. 3D).
While these simple steps for a full examination may seem no more than common sense, incorrect gestures and movements are not infrequent among dermatologists in daily practice. Therefore, we believe that our suggestions could pave the way toward greater awareness of the importance of posture and thus help prevent the acquisition of inappropriate gestures and movements. Similarly, following these steps in an orderly fashion allows us to perform a systematic examination that covers the whole body surface, without missing areas that are difficult to examine.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Aragüés IH, Castañeda AN, Vilariño EF, Simal G. Posturas ergonómicas para la exploración en dermatología. Actas Dermosifiliogr. 2018;109:661–663.