Hidradenitis suppurativa has been described as a chronic, recurrent, and disabling inflammatory disease involving the entire hair follicle.
Several treatments, including photodynamic therapy, have been used, but the results have been inconsistent and recurrence is high.
In this prospective study, we evaluated disease severity, quality of life, and treatment tolerance in 5 patients with moderate to severe hidradenitis suppurativa treated with photodynamic therapy using 5-aminolevulinic acid and a 635-nm light source. Treatment effectiveness was evaluated using the Sartorius severity score, the Dermatology Life Quality Index, and a visual analog scale for pain and disease activity.
Significant improvements were observed with all 3 instruments and the effects remained visible at 8 weeks. Our results suggest that photodynamic therapy with 5-aminolevulinic acid and a light wavelength of 635 nm could reduce disease severity and improve quality of life in patients with difficult-to-treat hidradenitis suppurativa.
La hidrosadenitis supurativa (HAS) se ha definido como una enfermedad inflamatoria crónica, recurrente y debilitante, que compromete todo el folículo piloso.
Varias alternativas terapéuticas, incluida la terapia fotodinámica, han sido utilizadas, con resultados variables y altas tasas de recurrencia.
El presente trabajo muestra la evaluación de severidad, calidad de vida y seguridad de una serie prospectiva de 5 pacientes con HAS moderada o severa, sometidos a terapia fotodinámica, utilizando ácido 5-aminolevulínico (ALA) y luz 635nm. Se evaluó la efectividad del tratamiento con el score de severidad de Sartorious, índice de calidad de vida (DLQI) y una escala visual analógica (EVA) para dolor y actividad de la enfermedad.
Los pacientes mostraron una mejoría significativa en las 3 variables estudiadas, con efectos visibles que se mantenían a las 8 semanas, sugiriendo que esta terapia podría ser efectiva en HAS refractaria a terapias convencionales, disminuyendo la gravedad y mejorando la calidad de vida de los pacientes.
Hidradenitis suppurativa is traditionally defined as a recurrent and debilitating chronic inflammatory disease that typically presents after puberty with deep and painful inflammatory lesions in apocrine gland–bearing areas, particularly the axillary, inguinal, and anogenital regions.1 However, recent findings emphasize the involvement of the whole hair follicle and pinpoint follicular occlusion and hyperkeratinization as the earliest pathophysiological event in hidradenitis suppurativa.2
While the pathogenesis of hidradenitis suppurativa remains uncertain, genetic factors, hormonal disorders, smoking, and obesity have all been shown to play some role.3 The fact that this condition is associated with Crohn disease and has been successfully treated with anti–tumor necrosis factor biologic agents has led to the suggestion that that patients might have an innate immune disorder, and current research focuses on this possibility.4,5
Hidradenitis suppurativa affects 1% of the European population; incidence is highest in the second and third decade of life and is 3 times higher among women than among men.4 Because of its severe physical and psychological effects, patients with this condition experience even greater morbidity and quality-of-life impairment than those with other chronic skin conditions, such as psoriasis.6
Treatment options are limited despite the high prevalence rate, and few clinical trials have assessed treatment safety or efficacy. Topical and systemic antibiotics, hormone therapy, oral retinoids, immunosuppressants, and surgery have all been tried, with variable outcomes and high recurrence rates.7,8
Evidence that photodynamic therapy is effective against acne9 has led to its use against hidradenitis suppurativa in small case series, with varying results.7,8,10–17 Treatment protocols in these series are not comparable due to variation in photosensitizers, light sources, and treatment regimens. The true role of photodynamic therapy against hidradenitis suppurativa is hard to determine based on the limited and mixed evidence currently available.7,8,10
Considering the above, and given the few options available for recalcitrant cases, we report our experience using aminolevulinic acid (ALA) and a 635-nm light source to treat 5 patients with moderate to severe hidradenitis suppurativa.Our aim was to evaluate the effectiveness of this treatment by assessing severity, quality of life, and safety.
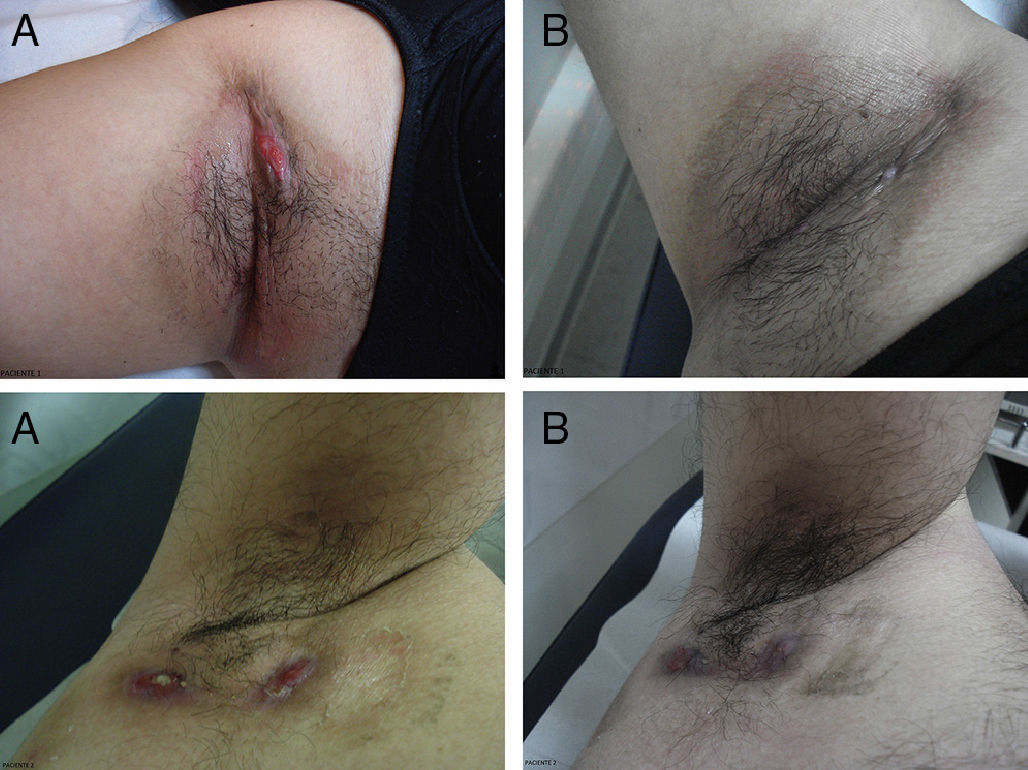
Patients and MethodsWe selected 5 patients, 1 man and 4 women, with a mean (SD) age of 26 (5) years and mean duration of disease of 4 (1) years. Four of the 5 cases involved both armpits (Fig. 1) and 1 involved the pubic region. Our inclusion criteria were Hurley stage II or III and hidradenitis suppurativa refractory to at least 2 medical treatments. Written informed consent was obtained from all patients.
Hidradenitis suppurativa: Bilateral axillary involvement. Results for patients 1 (above) and 2 (below) mentioned in Table 1. A, Before treatment. B, At 8 weeks’ follow-up.Treatment response was satisfactory in patient 1. Considerable reduction of inflammatory lesions and decreased signs of disease activity were observed in patient 2.
A 20% solution of ALA (Oldex, Recalcine) was applied for 1.5 hours followed by exposure to a 635-nm red light source (PDT 1200 L, Herbert Waldmann GmbH & Co.) at a 70 mW/cm2 fluence rate, with a total dose per session of 37 J/cm.2 Each patient had a minimum of 4 sessions at 1- to 2-week intervals, with clinical assessment at 4 and 8 weeks. At baseline and during follow-up visits we determined each patient's modified Hidradenitis Suppurativa Score as described by Sartorius et al., 18 quality of life in terms of the Dermatology Life Quality Index (DLQI) score,19 and pain and disease activity rated by the patient according to the following scale: 0, no symptoms or disease activity; 1, mild pain and/or activity; 2, moderate pain and/or activity; 3, severe pain and/or activity.
Directed questioning about treatment adverse effects was included in all sessions.
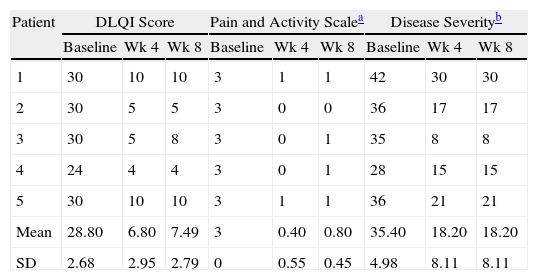
ResultsResults are summarized in Table 1. Patients showed significant improvement in all 3 scores, with effects persisting at 8 weeks’ follow-up. Mean (SD) severity scores dropped from 35 (5) at baseline to 18 (8) after treatment and DLQI decreased by an average 21 points after 4 treatment sessions, with both effects persisting after 8 weeks (Fig. 1). All patients scored 3 for pain and disease activity at baseline, and all scores were considerably lower (0-1) at 4 and 8 weeks.
Individual Patient Scores at Baseline and at 4 and 8 Weeks.
| Patient | DLQI Score | Pain and Activity Scalea | Disease Severityb | ||||||
| Baseline | Wk 4 | Wk 8 | Baseline | Wk 4 | Wk 8 | Baseline | Wk 4 | Wk 8 | |
| 1 | 30 | 10 | 10 | 3 | 1 | 1 | 42 | 30 | 30 |
| 2 | 30 | 5 | 5 | 3 | 0 | 0 | 36 | 17 | 17 |
| 3 | 30 | 5 | 8 | 3 | 0 | 1 | 35 | 8 | 8 |
| 4 | 24 | 4 | 4 | 3 | 0 | 1 | 28 | 15 | 15 |
| 5 | 30 | 10 | 10 | 3 | 1 | 1 | 36 | 21 | 21 |
| Mean | 28.80 | 6.80 | 7.49 | 3 | 0.40 | 0.80 | 35.40 | 18.20 | 18.20 |
| SD | 2.68 | 2.95 | 2.79 | 0 | 0.55 | 0.45 | 4.98 | 8.11 | 8.11 |
Abbreviation: DLQI, Dermatology Life Quality Index.
Treatment was well tolerated and the only adverse effect was a mild burning sensation during light exposure in 2 of the 5 patients.
DiscussionPhotodynamic therapy using 20% ALA was shown to be effective against hidradenitis suppurativa in this study, with significant reduction in severity scores and improved quality of life. This improvement was sustained at 4 and 8 weeks’ follow-up.
Gold et al.12 observed clinical improvement rates of 75% to 100% in 4 patients after 3 or 4 short-contact (15- to 30-minute) treatment sessions using blue light and 20% ALA, and suggested anti-inflammatory activity as the mechanism of action.
Schweiger et al.13 treated 12 patients for 4 weeks with a weekly application of 20% ALA for 45 minutes followed by exposure to either blue light or intense pulsed light. They observed a 50% reduction in mean lesion count after 4 weeks and a 29% reduction after 8 weeks, with DLQI scores lower than at baseline. Blue light was better tolerated than intense pulsed light.
Less encouraging results were obtained by Strauss et al.,14 who treated 4 patients with 20% ALA for 3 hours followed by red light exposure. One patient received 3 sessions at weekly intervals and experienced no clinical improvement, another received only 2 sessions and improved significantly at first but without lasting effect, and the remaining 2 patients did not complete the course due to pain during sessions. Sotiriou et al.15 treated 5 patients for 5 sessions at 2-week intervals using 20% ALA with red light and also found no significant improvement.
Using methyl aminolevulinate, Guglielmetti et al16 reported 1 case of recalcitrant HS treated with 16% methyl aminolevulinate and red light; inflammation and exudate in the treated areas decreased by 90% to 100% after the second session, with sustained effects at 4 months’ follow-up. In a similar case the patient received 9 treatment sessions at 2-week intervals, itching and discomfort were completely resolved at 6 months’ follow-up, with an 80% remission rate for skin lesions.17
Greater absorption of ALA together with higher production of protoporphyrin IX in hair follicles compared to other tissues has been suggested as the mechanism of action of photodynamic therapy for hidradenitis suppurativa.20 The main mechanisms proposed for photodynamic therapy against acne vulgaris, including decreased sebum production, destruction of Propionibacterium acnes, and reduced follicular occlusion,9,11 may also play a role against hidradenitis suppurativa.
Althought evidence supporting the use of photodynamic therapy for hidradenitis suppurativa is extremely limited, our findings suggest that topical ALA at 20% concentration with a 635-nm light source may be effective in cases refractory to conventional treatment, reducing disease severity and improving quality of life. Controlled clinical studies with larger sample sizes and longer follow-up are needed to assess the effectiveness of photodynamic therapy more conclusively and determine optimal treatment regimens.
Ethical DisclosuresProtection of human and animal subjects.The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed their hospital's protocol on the publication of data concerning patients and that all patients included in the study have received sufficient information and have given their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article.
FundingThis study was entirely funded by the Department of Dermatology of Pontificia Universidad Católica de Chile.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Andino Navarrete R, Hasson Nisis A, Parra Cares J. Efectividad de la terapia fotodinámica con ácido 5-aminolevulínico en el tratamiento de la hidrosadenitis supurativa. Serie de 5 casos. Actas Dermosifiliogr. 2014;105:614–617.