Benign cutaneous adnexal tumors are a heterogeneous group of uncommon lesions that includes spiradenoma and cylindroma. We report a case of coexisting spiradenoma and cylindroma and describe the corresponding dermoscopic findings.
A 37-year-old woman with no known medical history of interest was seen for an asymptomatic scalp lesion that was located on the hairline and had appeared 6 months earlier. Physical examination revealed a soft, rounded, skin-colored nodule (1 cm in diameter), upon which was a bluish, hard-elastic papule (Fig. 1).
Dermoscopy revealed a salmon-pink area containing linear vessels on the lesion surface and the presence at the lesion periphery of associated structures with homogeneous blue coloration. Yellowish-brown desquamation corresponding to seborrhoeic eczema was also observed (Fig. 1).
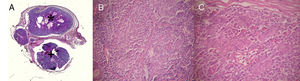
An excisional biopsy was performed. Subsequent histopathology revealed 2 distinct histological patterns. The first, more superficial pattern corresponded to a dermal tumor composed of multiple basophilic nodules formed by strands of dark basaloid cells and larger cells with pale nuclei. Ductal structures were also observed inside the lobes, as well as hyaline drops and squamous corpuscles (Fig. 2).
A, Spiradenoma (*) and cylindroma (+) within a single lesion (hematoxylin-eosin, original magnification ×40). B, Spiradenoma: upper portion of the lesion consisting of cells with small hyperchromatic nuclei and others with large, pale nuclei (hematoxylin-eosin, original magnification ×400). C, Cylindroma: lower portion of the lesion consisting of tumoral nests arranged in a checkerboard pattern and surrounded by hyaline bands (hematoxylin-eosin, original magnification ×400).
The second pattern, observed in the deepest part of the lesion, consisted of irregular strands of basophilic cells arranged in a checkerboard pattern and surrounded by eosinophilic hyaline bands (Fig. 2). Based on these findings a diagnosis of spiradenocylindroma was established.
Spiradenoma, first described by Kersting and Helwing in 1956,1 is more frequent in females aged 15 to 35 years. The clinical presentation consists of a single, soft, bluish nodule of 1 cm to 2 cm in diameter that is painful on palpation and is typically located on the trunk or neck.1,2 In 2015 Sahin3 reported the following dermoscopic features of this lesion: bluish pigmentation, varied vascular structures, and reticulated pigmentation at the lesion periphery. In the same year Ankad and coworkers4 described the trichoscopic features of spiradenoma, including the presence of red serpentine linear structures surrounded by whitish areas.
The term cylindroma was first used by Billroth in 1856 to describe a benign adnexal tumor that mainly affects women aged 20 to 30 years.5,6 Cylindroma presents as a firm, pink nodule located on the face or scalp, usually grows slowly, and has a mean size of 2mm to 6 mm.7 Reported dermoscopic patterns include arboriform vessels on a whitish, salmon-pink background, blue dots and globules, and ulceration.8,9
Spiradenoma and cylindroma are neoplasms of controversial histogenesis. Historically, spiradenoma has been considered a tumor of eccrine differentiation. However, its association with trichoepitheliomas in Brooke-Spiegler syndrome and with milium cysts in Rasmussen syndrome suggests a probable apocrine origin. Cylindroma was originally considered an apocrine tumor. Recent studies have revealed apocrine and eccrine characteristics in both tumor types. Some authors even claim that these tumors are derived from the follicular epithelium, since they are positive for CD200, an immunohistochemical marker of hair-follicle stem cells.5,10
While co-occurrence of both neoplasms in the same patient has been previously reported, coexistence within the same clinical lesion is highly unusual. Meybehm and Fischer proposed the term spiradenocylindroma for this particular presentation.11
Spiradenocylindroma presents as a benign tumor, which can be solitary or, in the case of Brooke-Spiegler syndrome, multiple. Physical examination of our patient, who had no family history of interest, revealed a solitary lesion and no other pathological findings.10,11
The dermoscopic features of spiradenocylindroma have not been previously described. In our case, the main dermoscopic findings were areas with salmon-pink coloration, linear vessels, and the presence at the lesion periphery of structures with a homogeneous blue coloration (Table 1).
Differential Diagnosis of Spiradenoma, Cylindroma, and Spiradenocylindroma
| Spiradenoma | Cylindroma | Spiradenocylindroma | |
|---|---|---|---|
| Age at presentation, y | 15–351 | 20–306 | 20–7312 |
| Clinical appearance | Soft bluish nodule, painful on palpation, located on the trunk and neck.1,2 | Firm, pink nodule located on the face or scalp.7 | Solitary or multiple lesions. Frequently associated with Brooke-Spiegler syndrome.12 |
| Histology | Nodules composed of 2 cell types: small hyperchromatic cells and other larger cells with pale nuclei and ductal differentiation. Thin basal membrane.Frequent lymphocytic infiltration.10 | Small lobules of basaloid cells arranged in a checkerboard pattern and surrounded by a prominent hyaline basement membrane.Positive periodic acid-Schiff staining. Absence of inflammatory infiltrate.10 | Two distinct histological patterns within the same lesion.10 |
| Dermoscopic features | Light blue pigment with peripheral reticulate pigmentation, associated with reddish linear serpentine structures surrounded by whitish areas.3,4 | Blue dots and globules associated with arboriform vessels on a whitish, salmon-pink background.8,9 | Salmon-pink areas, linear vessels, and peripheral structures with homogeneous blue pigmentation. |
We have reported this case to share our finding of a very rare adnexal tumor and to describe the dermoscopic features of spiradenocylindroma.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We thank the patient, who provided written consent to publication of the images included in this report.
Please cite this article as: Senarega A. Espiroadenocilindroma: hallazgos dermatoscópicos. 2019;110:604–606.