The patient was a 76-year-old woman with a history of systemic hypertension and IgA κ multiple myeloma (stage IIIB) diagnosed 1 year previously after an episode of acute renal failure. The patient also had Bence-Jones proteinuria, normocytic normochromic anemia, and lytic lesions in the axial skeleton, sternum, and pelvis. She had received several cycles of bortezomib and melphalan, although her disease continued to progress.
Physical ExaminationThe clinical manifestations comprised multiple erythematous nodules measuring between 0.5cm and 3cm in diameter that had first appeared on the left heel 2 months previously (Fig. 1). The patient reported associated pain. She also had severe macroglossia, although no significant lesions were visible on the rest of the skin or mucosas.
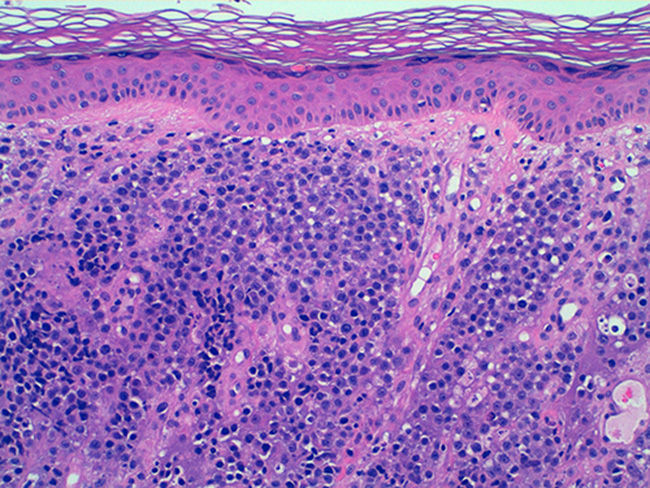
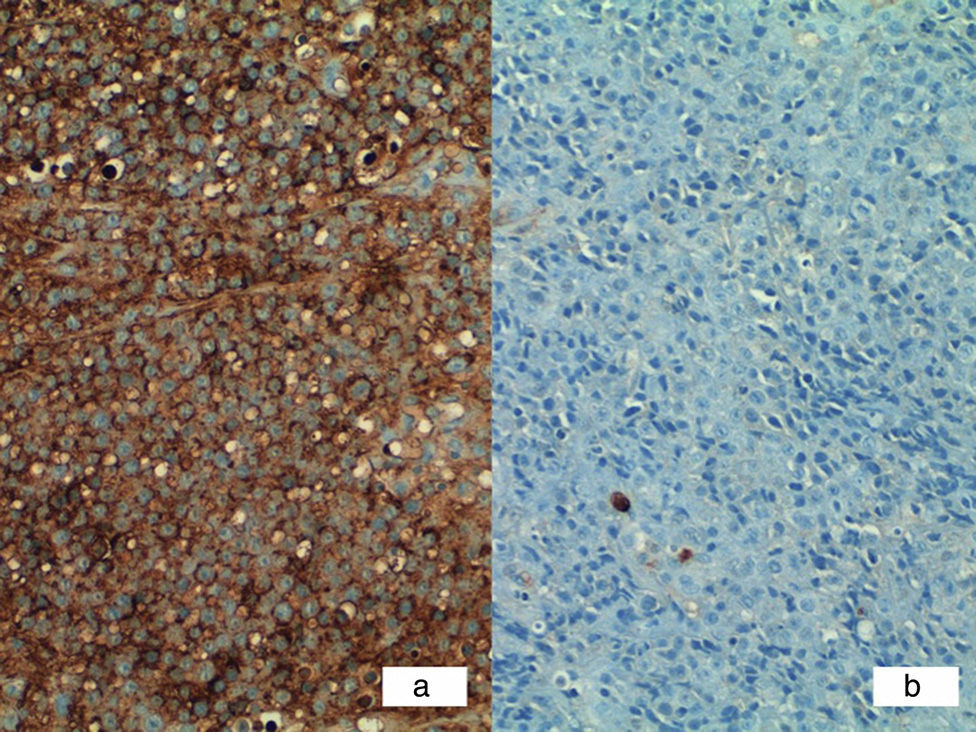
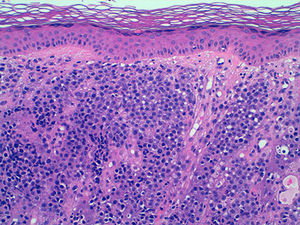
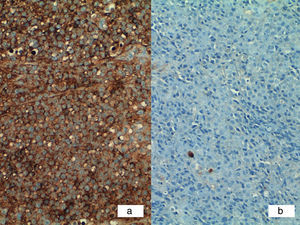
HistopathologyHistopathology of the largest nodular lesion revealed a diffuse infiltrate of atypical cells throughout the dermis that were plasmablastic in appearance (Fig. 2). These cells were positive for Ki-67, CD56, CD79a, CD138, cyclin DI, and IgG κ (Fig. 3A) and negative for IgG λ (Fig. 3B).
Additional TestsAlthough a radiograph of the affected limb was requested, the patient did not return to the clinic.
What is your diagnosis?
DiagnosisCutaneous plasmacytoma associated with multiple myeloma.
Clinical Course and TreatmentGiven the poor response to initial chemotherapy and the progression of the disease, no further therapy was prescribed. The biopsy did not rule out bone involvement contiguous to the skin lesions.
DiscussionSkin involvement in multiple myeloma is very rare and generally occurs during the later stages of the disease.1 It was first described in 1910 by Bruno Bloch; to date, some 150 cases have been reported in the literature.2
The 4 known neoplasms of plasma cells are classic multiple myeloma, extramedullary plasmacytoma without multiple myeloma, solitary plasmacytoma of bone, and plasma cell leukemia.2 All 4 types can affect the skin, although the most common mechanism is by direct extension to the skin from an underlying bone lesion; metastatic lesions without contiguous bone involvement are less likely.3,4
Cutaneous plasmacytoma in the context of multiple myeloma is mainly associated with IgG and IgA.
Histopathology usually reveals a monomorphous dermal infiltrate of plasma cells with a diffuse interstitial or nodular pattern. Immunohistochemistry is usually positive for CD38, CD43, CD56, CD79a, CD138, epithelial membrane antigen, and κ and λ light chains.
The differential diagnosis includes diseases such as squamous cell carcinoma, skin metastases from internal neoplasms, cutaneous marginal zone lymphoma, cutaneous leishmaniasis, sarcoidosis, and amelanotic melanoma. However, the clinical setting of the patient should point us in the direction of plasmocytoma associated with multiple myeloma.
Treatment should be aimed at monoclonal gammopathy using autologous bone marrow transplant in persons aged less than 65 years and chemotherapy with bortezomib and melphalan, combined with local radiation therapy and surgical removal of the skin lesion where necessary.5
Please cite this article as: Gómez-Armayones S, Climent F, Servitje O. Nódulos cutáneos asociados a mieloma múltiple. Actas Dermosifiliogr. 2015;106:581–582.