Chlamydia trachomatis infections remain a burden worldwide. The goals of this study were to determine the number of C. trachomatis infections per year, characterize the demographic traits of the infected population and identify the associated sexually transmitted infections (STI), over the last 11 years, in Lisbon main Hospital Centre.
Materials and methodsLaboratorial confirmed C. trachomatis infections diagnosed between January 1st, 2009 and December 31st, 2019 were evaluated.
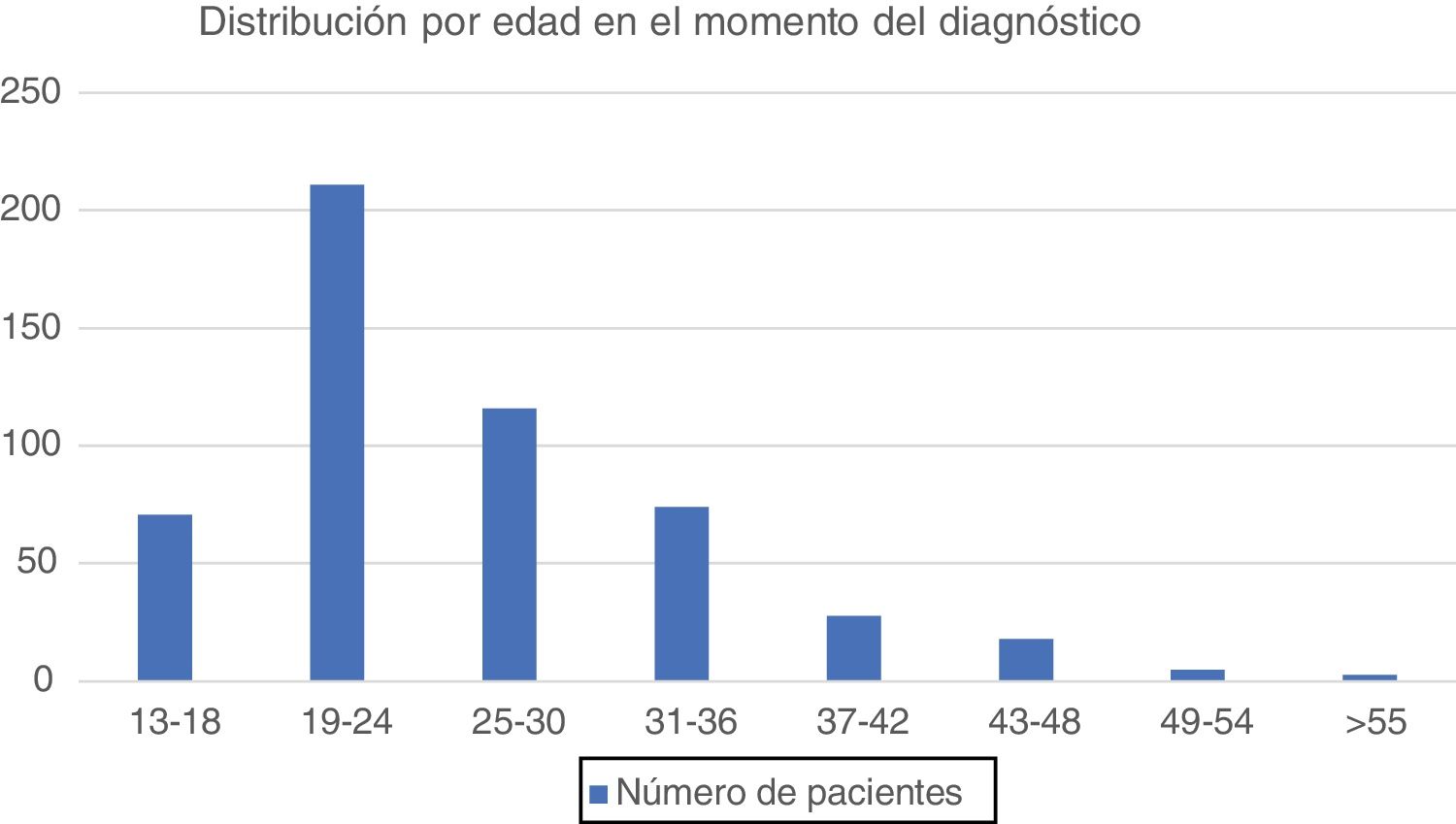
ResultsA total of 6404 samples were collected, with 602 being positive for C. trachomatis, corresponding to 550 patients. 60% of diagnoses were made by dermatovenereologists and most cases occurred in males (n = 371; 67.5%), with a median age of 26.1 years (standard deviation 7.98), ranging from 13 to 68 years. More than half the cases (51.3%) occurred below the age of 25 years.
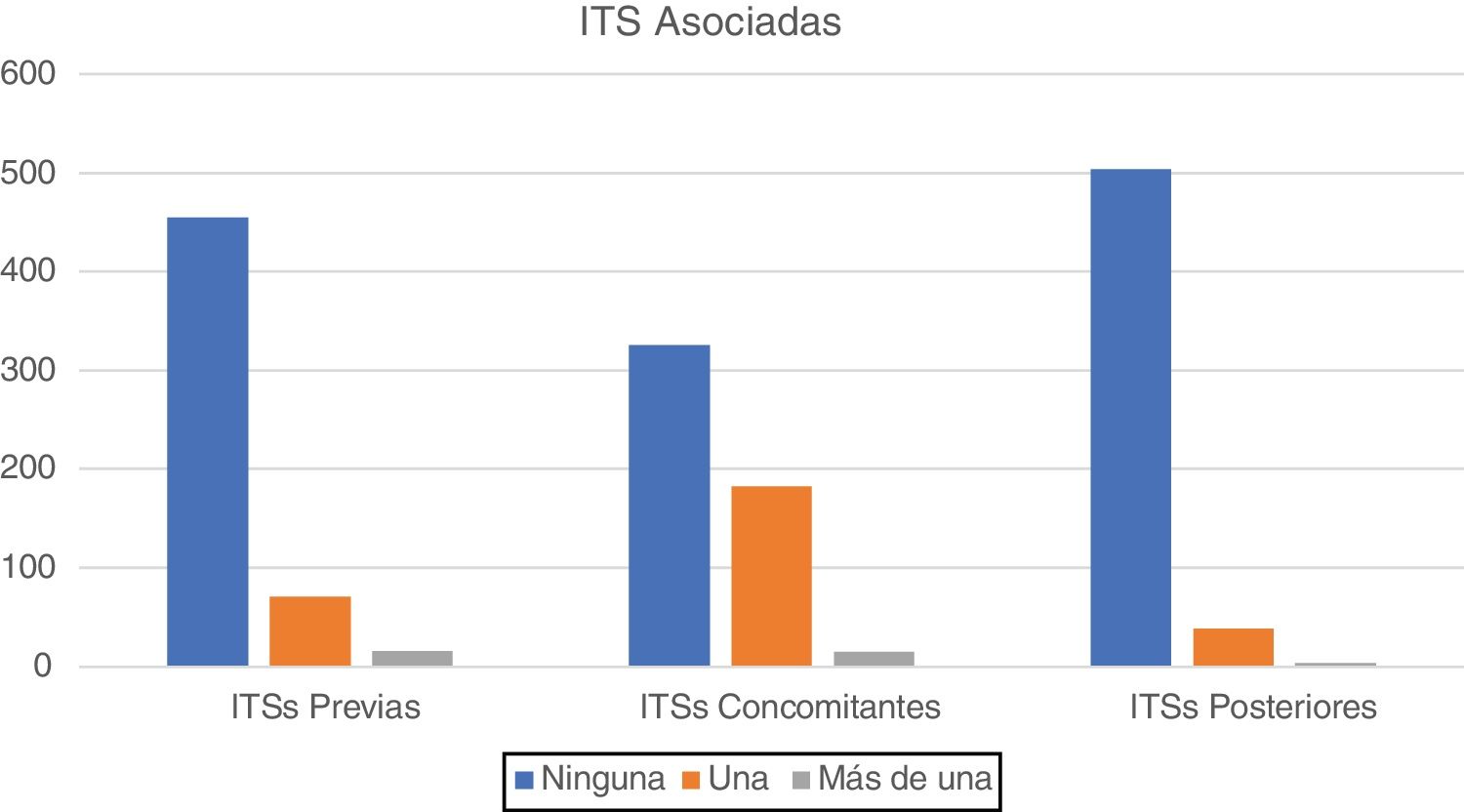
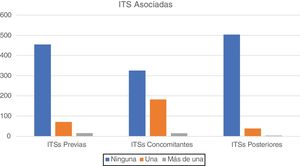
In 87 patients (15.8%) there was previous history of STI, in 198 patients (36%) a concomitant STI was present and 43 patients (7.8%) developed a posterior STI.
Concerning follow-up, 196 patients (corresponding to 35.6% of total patients) did not show for a re-evaluation after the diagnosis was made.
ConclusionConfirmed cases of C. trachomatis infection have risen along the years, affecting mainly people younger than 25 years. C. trachomatis infection is especially associated with Neisseria gonorrhoeae infection, but other STI are also very prevalent. Considering the potential complications of C. trachomatis infection, screening and treatment are necessary. The high percentage of diagnoses made by dermatovenereologists support the pivotal role of dermatovenereology in diagnosing C. trachomatis infections.
Las infecciones por Chlamydia trachomatis siguen siendo un problema de salud mundial. Los objetivos de este estudio fueron determinar el número de infecciones por C. trachomatis por año, caracterizar los rasgos demográficos de la población infectada e identificar las infecciones de transmisión sexual (ITS) asociadas. Con dicha finalidad se recogieron los casos diagnosticados en los últimos 11 años en el principal centro hospitalario de Lisboa.
Materiales y métodosSe incluyeron todas las infecciones causadas por C. trachomatis y confirmadas laboratorialmente entre el 1 de enero de 2009 y el 31 de diciembre de 2019.
ResultadosSe recogieron un total de 6.404 muestras, de las cuales 602 fueron positivas para C. trachomatis, y correspondían a un total de 550 pacientes. El 60% de los casos fueron diagnosticados por dermatólogos – venereólogos. La mayoría de los casos se observaron en pacientes de sexo masculino (n = 371; 67.5%), con una mediana de edad de 26.1 años (desviación estándar de 7.98) y con un rango de edad que oscilaba entre los 13 y los 68 años. Más de la mitad de los casos (51.3%) se diagnosticaron en pacientes menores de 25 años.
En 87 pacientes (15.8%) se hallaron antecedentes de otra ITS. En 198 pacientes (36%) se diagnosticaron además otras ITS concomitantes y 43 pacientes (7.8%) presentaron una ITS posteriormente.
En cuanto al seguimiento, 196 pacientes (correspondientes al 35.6% del total de pacientes) no acudieron a una reevaluación tras el diagnóstico.
ConclusiónEl número de casos confirmados de C. trachomatis han demostrado un incremento con el transcurso de los años, afectando principalmente a pacientes menores de los 25 años. La infección por C. trachomatis se asociará especialmente a la infección por Neisseria gonorrhoeae, sin embargo, las infecciones concomitantes por otras ITS serán también muy prevalentes. Teniendo en cuenta las posibles complicaciones de la infección por C. trachomatis, tanto las pruebas de cribado, como el tratamiento oportuno de esta entidad serán necesarios. El hecho de que un elevado porcentaje de diagnósticos se hayan realizado por dermatólogos - venereólogos confirma el rol fundamental que tendrán estos especialistas en el diagnóstico de esta infección.
Chlamydia trachomatis (C. trachomatis) infection represents the most frequently detected bacterial sexually transmitted infection (STI) worldwide.1 In women most infections are asymptomatic, with less than one-third of women having complaints, such as, dysuria or vaginal discharge, while men are symptomatic in more than half the cases.2,3
Clinical manifestations depend on the Chlamydia serovariants, with serovariants D-K being associated with infection in the genital tract, pharynx, and rectum, while, serovariant L is associated with lymphogranuloma venereum (LGV).3 Absence of treatment can lead to pelvic inflammatory diseases, ectopic pregnancy and infertility in women and epididymitis in men.1,2 Also, infections by C. trachomatis increases the risk of HIV acquisition.1,2 Infection in pregnant women can be transmitted to their children during delivery, with subsequent risk of ophthalmia neonatorum and pneumonia.4,5
The gold standard for C. trachomatis diagnosis is nucleic acid amplification test that can be performed on urine, urethral, vaginal, and rectal samples.3
Reducing the incidence of anal and genital chlamydial infections is difficult since infections are frequently asymptomatic.2 Additionally, there is no C. trachomatis vaccine, so screening of patients, particularly in the presence of other STIs, and partner treatment must be done to prevent C. trachomatis propagation.2,6
Antimicrobial resistance of Chlamydia trachomatis is infrequent, with even lower rates for doxycycline, when compared to azithromycin.7 As such, azithromycin or doxycycline are recommended as first-line therapy.7,8
ObjectivesThe goals of this study were:
- 1
To determine the number of C. trachomatis infections per year.
- 2
To characterize the demographic traits of the infected population.
- 3
To identify the proportion of asymptomatic vs symptomatic patients.
- 4
Evaluate the presence of other previous, concomitant, and posterior sexual transmitted infections.
We conducted a retrospective study of all patients with laboratorial confirmed C. trachomatis infections, diagnosed between January 1st, 2009 and December 31st, 2019, in the Microbiology Laboratory of Hospital de Santa Maria, Lisbon, Portugal. We analysed the following parameters: year of diagnosis, which department ordered the test, patient’s age, gender, nationality, sexual orientation, number of sexual partners in the previous 6 months, if the patient had symptoms related to C. trachomatis infection, previous, concomitant, and subsequent sexually transmitted infections, treatment prescribed for C. trachomatis infection, if the patient presented to a follow-up consultation, and if patients were pregnant at time of diagnosis.
Being symptomatic was defined as presenting with manifestations characteristically associated with C. trachomatis infection, which include, cervicitis, pelvic inflammatory disease, urethritis, epididymitis, prostatitis or proctitis. If patients presented with other concomitant diagnosis (with exception of Neisseria gonorrhoeae) that could justify the presence of the clinical manifestations, they were considered asymptomatic to C. trachomatis infection.
Statistical analysis was performed with SPSS (IBM Statistics, version 23.0). Categorical variables are presented as frequencies and percentages, and continuous variables as means and standard deviations. Comparisons between groups were based on chi square tests. All reported p values are two-tailed, with a p value <0.05 indicating statistical significance.
ResultsFrom 2009 to 2019, a total of 6404 samples for C. trachomatis were collected (562 urethral swabs, 857 vaginal swabs and 4985 urine samples) with 34 tests being inconclusive, which were excluded. We found 602 confirmed cases of C. trachomatis (9.4% of total samples), corresponding to 550 patients. The principal method for diagnosis was urine samples (8,7% of total urine samples collected were positive) with 434 patients being diagnosed by this method, corresponding to 78,9% of total patients.
Over these 11 years, the number of cases of anal and urogenital infection by C. trachomatis increased from a minimum of 16 cases, in 2011, to a maximum of 111 cases per year, in 2018 (Fig. 1). 42 patients had more than one positive test and, of these, 35 had two positive tests in different occasions, six patients had three positive tests on different occasions and one patient had five positive tests on different occasions.
Most patients were males (n = 371; 67,5%). Median age was 26.1 years (standard deviation 7.98), ranging between 13 and 68 years (Fig. 2). More than half cases (51.3%) occurred below the age of 25 years.
The majority of diagnoses were made by the dermatovenereology department (330 patients – 60%), either in consultation (93 patients – 16.9%) or in the dermatovenereology emergency (237 patients – 43.1%). The remaining cases were diagnosed by the gynaecology department (109 patients- 19.8%), general emergency department (37 patients – 6.7%), paediatrics department (24 patients – 4.4%), infectious diseases department (20 patients – 3.6%) and by other departments, such as urology and rheumatology (30 patients – 5.5%).
Concerning nationality, 396 patients (72%) were Portuguese, with the rest being foreign patients (154 patients -28%), mostly from Brazil and Portuguese speaking African countries, like Angola, Mozambique, and Cape Verde.
As for the number of sexual partners, in the 6 months previous to the diagnoses: five patients (0.9%) had no sexual partners, 242 patients (44%) had one sexual partner, 85 patients (15.5%) had two sexual partners, 53 patients (9.6%) had three sexual partners, 18 patients (3.3%) had four sexual partners and 23 patients (4.2%) had 5 or more sexual partners. Data regarding number of sexual partners was not available in 124 patients (22.5%).
Regarding sexual orientation, 372 patients were heterosexual (67.6%) and 50 patients were homosexual or bisexual (9.1%). Data regarding sexual orientation was not available in 128 cases (23.3%).
Of the 371 male patients, 276 (74.3%) were considered symptomatic to C. trachomatis infection, most presenting with symptoms of urethritis, while 7 patients presented with proctitis. Of the 179 female patients, only 39 patients (21.7%) were considered symptomatic to C. trachomatis infection, with 140 patients (78.3%) being asymptomatic.
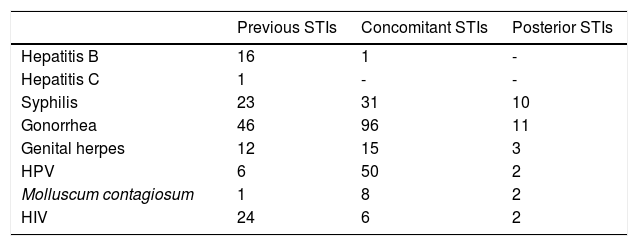
In 87 patients (15.8%) there was previous history of STI, with 71 patients reporting having had another STI and 16 patients admitting having had more than one previous STI (Fig. 3 and Table 1).
Concomitant STI (diagnosed in simultaneous with Chlamydia Trachomatis) were frequent. 198 patients (36%) had a concomitant STI, of which 15 patients had two or more STIs (Fig. 3 and Table 1).
As for posterior STIs (diagnosed after Chlamydia Trachomatis was identified) this occurred in 43 patients (7.8%), with 39 patients developing one more STI and 4 patients acquiring more than one STI (Fig. 3 and Table 1).
Considering therapeutic options, azithromycin was used in monotherapy in 471 patients (85.6%). 32 patients had doxycycline as first option (5.9%) and 10 patients (1.8%) were treated with penicillin. 37 patients (6.7%) had no therapy to Chlamydia Trachomatis infection administered, because they did not attend the follow-up visit. 12 patients (2.2%) had both azithromycin and doxycycline, because of persistence of symptoms. One patient had levofloxacin, after having persistent symptoms despite azithromycin and doxycycline treatment.
Regarding detection of C. trachomatis, during pregnancy, there were nine women (1.6%) found positive and they were treated with azithromycin. Of these, three of them terminated pregnancy, for different reasons. None of the six children had complications associated with C. trachomatis infection.
A significant proportion of patients, corresponding to 196 patients (35.6%) did not show for a re-evaluation consultation after the diagnoses was made.
DiscussionIn this study we evaluated all confirmed cases of anal and urogenital C. trachomatis, over 11 years at a Tertiary Care Portuguese Hospital.
Overall, we found a rise in the number of confirmed cases of infection, along the years, that related to an also higher number of screening tests (Fig. 1). This increased number of screening tests may reflect a rising incidence of anal and urogenital chlamydial infection, similar to trends reported in other countries.9–12 However, this increment is not proportional, and this may be due to the fact that in earlier years, mainly symptomatic patients were tested and so the likelihood of a positive test was higher, when compared to most recent years where screening of asymptomatic leads to a higher detection of cases, but with also many negative tests.
There were 42 patients with more than one positive C. trachomatis test at different times. Since in many instances, no tests of cure were collected we cannot ascertain if these cases represent a failure of initial treatment or a chlamydial reinfection.
The age at diagnosis ranged from 13 years to 68 years (mean age, 26.1). The highest prevalence of chlamydia occurred predominantly in younger age groups (< 25 years). Our findings agree with European reports stating that, C. trachomatis infection cases peak among 20-24-year-old.13,14
Infection with N. gonorrhoeae was the most prevalent previous (46 patients – 8.3%), concomitant (96 patients -17.4%), and posterior STI (11 patients – 2%). This reflects an important association, specifically as concomitant infections, and the need for simultaneous treatment of both infections.15
Taking into account only female patients, most infections were asymptomatic (78.3%) (p < 0.05). This is in accordance with other reports, affirming that, in the female population, most of C. trachomatis infections are asymptomatic.16–18 As for male patients, 74.3% were considered symptomatic (p < 0.05), confirming that men are predominantly symptomatic to C. trachomatis infections.18 One factor possibly affecting the number of symptomatic patients is that many patients were evaluated in an emergency setting, what may overestimate the rate of symptomatic patients. Additionally, in 96 cases, concomitant infection with N. gonorrhoeae was present, and so this may be a confounding factor, because these symptoms cannot be attributed exclusively to chlamydial infection. These data support that screening is essential, especially in the female population, given that most infections are asymptomatic.
The most prescribed treatment was azithromycin. Both the CDC and IUSTI recommend azithromycin 1 g orally in a single dose or doxycycline 100 mg bd for 7 days, as a first-line treatment for urogenital C. trachomatis infection, while the British Association for Sexual Health and HIV, no longer recommends azithromycin as a first option, because of the emergence of sexually transmitted pathogens, such as, Mycoplasma genitalium than can present as a coinfection.19–22 We did not perform tests of cure for the majority of patients, however, tests of cure are recommended for rectal infections and in pregnant patients.19–21
Penicillin was initially administered to 10 patients (1.8%), mainly because of suspicion of syphilis, with 7 patients having confirmed concomitant syphilis. 37 patients (6.7%) had no therapy to C. trachomatis infection administered, because they did not show for a revaluation consultation.
Concerning the nine cases of detection of C. trachomatis during pregnancy, there were no consequences to the children, and six of them were born full-term and with a normal weight, while the other three pregnancies were terminated, by mother’s choice. However, infections during pregnancy have been associated with premature rupture of membranes, preterm birth and low birthweight.23,24 Therefore, screening for C. trachomatis, during pregnancy should be recommended.23,24
Our elevated rate of loss of follow-up is important (35.6% of total patients), because it does not allow for partners treatment and in the cases where the diagnoses was not considered (either because the patient was asymptomatic or presented with clinical manifestations suggestive of other STI) no treatment for C. trachomatis infection was prescribed. Aside from this fact, a follow-up visit is another chance to remind patients of protective measures against STIs, possibly reducing future STIs. Although we have not found any statistical significance between presenting to a follow-up consultation and developing posterior STIs (30/354 patients vs 15/196 patients) we cannot exclude that patients who abandoned follow-up at our hospital, were not diagnosed with other STIs at a different hospital.
Our study has several limitations: it is a retrospective study and there is missing data regarding the sexual orientation and number of sexual partners in the last 6 months in many patients. Also, some patients may not disclaim all the STIs had previously.
Another limitation is that the amount of STIs acquired after C. trachomatis diagnoses may be underestimated, because of loss of follow-up.
ConclusionConfirmed cases of C. trachomatis infection have risen along the years in our hospital, with people younger than 25 years representing more than half the number of infected patients. This data emphasizes the need for screening, especially among adolescents and young adults.
Data from this study supports that, in women, most C. trachomatis infections are asymptomatic, while men usually present with genitourinary complaints.
Our findings support a strong association with other STIs and the necessity for screening in order to stop dissemination of this infection in the community.
The high percentage of diagnoses made by dermatovenereologists support the pivotal role of dermatovenereology in diagnosing C. trachomatis infections.
FinancingThe authors did not receive any financial support for the research, authorship and/or publication of this article.
Declaration of conflicts of interestThe authors declared that they had no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Please cite this article as: Silva L, Queirós C, Borges-Costa J, Barreto R, Filipe P, Melo-Cristino J, Infecciones por Chlamydia trachomatis en un hospital portugués de atención terciaria: estudio retrospectivo de 11 años. Actas Dermosifiliogr. 2021;112:528–533.