Capillary malformations are the most common vascular malformations in childhood. The current treatment of choice is pulsed dye laser (PDL) therapy, but this frequently does not result in complete resolution. The search for alternative treatment strategies thus continues. In this study we describe our experience with the use of sequential dual-wavelength PDL and Nd:YAG laser therapy in patients with capillary malformations.
Material and methodsWe conducted a retrospective, descriptive study of patients with capillary malformations treated with dual-wavelength PDL and Nd:YAG laser therapy between 2006 and 2011. Four dermatologists rated the effectiveness of treatment on a scale of 10 to 0. We also investigated the potential value of the following factors as predictors of better treatment response: sex, malformation size and color, and presence of associated hypertrophy. Adverse effects were also analyzed.
ResultsWe studied 71 patients and most of them experienced a statistically significant improvement after treatment. More favorable responses were observed for violaceous malformations, lesions with associated hypertrophy, and smaller lesions. Adverse effects were reported for 26.76% of patients, and the most common effect was the appearance of isolated areas of skin atrophy.
ConclusionsWe consider that sequential dual-wavelength PDL and ND:YAG laser therapy is an effective alternative for treating capillary malformations in selected patients.
Las malformaciones capilares son las malformaciones vasculares más frecuentes en la infancia. El tratamiento de elección sigue siendo el láser de colorante pulsado (LCP), sin embargo, la resolución completa con este habitualmente no se consigue, motivo por el que se siguen buscando otras alternativas terapéuticas. En este estudio comunicamos nuestra experiencia con el láser dual secuencial de LCP y Nd:YAG.
Material y métodosSe efectuó un estudio retrospectivo y descriptivo de los pacientes con malformaciones capilares tratados con el láser dual de LCP y Nd:YAG desde 2006 hasta 2011. Cuatro dermatólogos valoraron el grado de eficacia en una escala del 10 al 0. Se analizó la posibilidad de factores predictores de mejor respuesta al tratamiento: sexo, color de la lesión, existencia de hipertrofia asociada y tamaño de la malformación. Se recogieron igualmente los efectos secundarios.
ResultadosSe incluyeron 71 pacientes, presentando el conjunto de ellos una mejoría estadísticamente significativa tras el tratamiento. Las malformaciones de coloración violácea que tenían hipertrofia asociada y las de menor tamaño se asociaron con una mejor respuesta. Se produjeron efectos adversos en un 26,76% de los pacientes, siendo la presencia de zonas atróficas puntuales el más frecuente.
ConclusionesConsideramos que el láser dual de LCP y Nd:YAG es una alternativa eficaz para el tratamiento de malformaciones capilares en paciente seleccionados.
Capillary or venular malformations occur in approximately 0.1% to 2% of newborn infants and are the most common type of vascular malformations.1 They can be found on any body part but occur most frequently on the head and neck.
Capillary malformations present as pink patches that tend to darken with age, acquiring a violaceous color and a pebbly appearance. They can also be associated with hypertrophy of the soft tissues and underlying bone.
The current treatment of choice for capillary malformations is pulsed dye laser (PDL) therapy, but in many patients this is ineffective or achieves only partial improvement. The search for alternative treatment strategies thus continues.
Good results have been achieved with other types of laser therapy, including Nd:YAG2–4 and alexandrite.5–8 Nd:YAG and alexandrite lasers both achieve greater penetration than PDL, which is one reason why hypertrophic lesions tend to respond better to these treatment options. Other light sources, such as intense pulsed light therapy,9–15 have also been used, as well as laser therapy combined with antiangiogenic drugs.16 Photodynamic therapy also appears to be effective.17
In this study, we describe our experience with the treatment of capillary malformations using dual-wavelength sequential pulses from a PDL and a Nd:YAG laser (Cynergy Multiplex, Cynosure, Inc., Westford, MA, United States).
Materials and MethodsStudy PopulationWe conducted a retrospective, descriptive study of patients with capillary malformations treated with dual-wavelength PDL and Nd:YAG laser therapy in the laser therapy unit of Hospital Ramón y Cajal between 2006 and 2011. Patients with an incomplete clinical history or insufficient photographic documentation were excluded.
In order to identify factors that might have influenced the response to therapy, we collected the following data on each patient: sex, color of lesion (red, pink, or violaceous), associated soft-tissue hypertrophy, and size of lesion (maximum diameter <3cm, 3-10cm, or >10cm).
ProcedureThe patients or their guardians were informed of the likely benefits, risks, and potential complications of the treatment and the available alternatives. Written informed consent was obtained before treatment was started.
Anesthesia was used in some cases, depending on the size and site of the lesion and the age and tolerance of each patient. In cases in which anesthesia was indicated, the options used were anesthetic cream containing lidocaine and prilocaine (Eutectic Mixture of Local Anesthetics [EMLA], AstraZeneca, Wedel, Germany) applied under occlusion 2hours before each session or general anesthesia administered under the supervision of the anesthesiology department.
The parameters for the sequential dual-wavelength pulses from a 595nm PDL and a 1064nm Nd:YAG laser were as follows: with a 10mm spot size, a 10ms pulse with a PDL at a fluence of 6J/cm2, a 1 second delay, followed by a 15ms pulse with a Nd:YAG laser at a fluence of 30-60J/cm2; or, with a 7mm spot size, a 10ms pulse with a PDL at a fluence of 6J/cm2, a 1 second delay, followed by a 15ms pulse with a Nd:YAG laser at a fluence of 30-80J/cm2. Patients attended treatment sessions approximately once every 6 months.
A forced-air cooling device (Cryo 5, Zimmer MedizinSysteme GmbH, Neu-Ulm, Germany) set to its highest fan speed (6) was used throughout the treatment. In patients with larger malformations and a marked hypertrophic component, ice was also applied immediately after the treatment.
For posttreatment care, patients were instructed to apply a topical antibiotic cream (fusidic acid, Fucidine, LEO Pharma, Barcelona, Spain) once daily for approximately 1 week and to avoid exposure to sunlight and use sunscreen with a sun protection factor of 50 or higher for at least 2 months after each treatment session.
AssessmentWe used a visual scale based on photographs taken before the first treatment session and at least 1 month after the last session. Taking into account skin color and texture and lesion height, 4 dermatologists evaluated the effectiveness of the treatment on a scale of 10 to 0, where 10 was the original pretreatment lesion and 0 was completely normal skin. Each patient's improvement was calculated as the mean of those 4 scores.
Patient photographs and medical histories were searched for evidence of adverse effects.
Statistical AnalysisFor each variable studied and in the analysis of each subgroup, data were checked for normal distribution with the Kolmogorov-Smirnov goodness-of-fit test and the normality of the sample was confirmed.
Mean and standard deviation were the descriptive measures used for the quantitative variables and percentages were used for the qualitative variables.
For the quantitative variables, the paired t test was used to analyze paired data.
The t test or the analysis of variance were used to analyze unpaired data, depending on the number of variables being studied. When significant differences were found between a group of 3 or more variables, the Scheffe test was subsequently used to determine whether differences existed between the means of any groups.
In all cases, statistical significance was set at P<.05.
Agreement between observers was assessed with the intraclass correlation coefficient.
ResultsSeventy-one patients—37 male (52.11%) and 34 female (47.89%)—were included in the study. The patients were between the ages of 8 and 76 years at the start of treatment, and the mean (SD) age was 39.25 (15.00) years.
Nineteen patients (26.76%) had pink lesions, 29 (40.85%) had red lesions, and 23 (32.39%) had violaceous lesions. Soft-tissue hypertrophy associated with the lesion was present in 38 patients (53.52%).
The maximum lesion diameter was <3cm in 6 patients (8.45%), 3-10cm in 21 patients (29.58%), and >10cm in 44 patients (61.97%).
No previous treatment had been administered in 18.31% of the patients, whereas 81.69% of the patients had been treated at least once. Of the patients who had received treatment, 98.28% had been treated with PDL, 18.97% with carbon dioxide laser, 10.34% with diode laser, 3.45% with Nd:YAG laser and electrocoagulation, and 1.72% with alexandrite laser, argon laser, intense pulsed light, surgery, and radiation therapy.
The number of laser treatment sessions per patient ranged from 1 to 15, and the mean (SD) number of sessions was 5.18 (3.17).
The intraclass correlation coefficient among the 4 evaluators was 0.947 (95% CI, 0.923-0.964), indicating very good, statistically significant agreement.
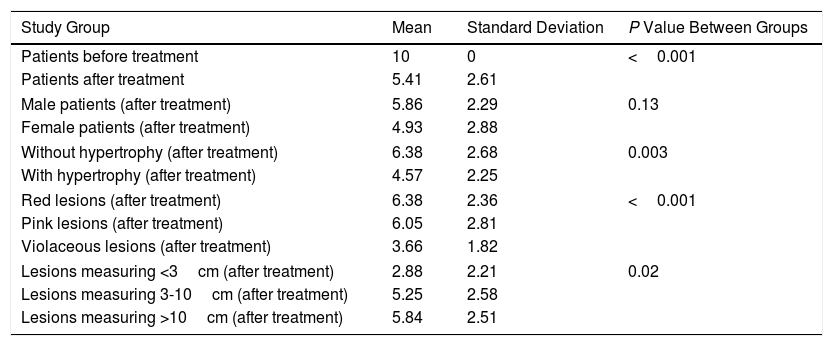
The difference between the pretreatment and posttreatment values for the entire group of patients was statistically significant (P<.001) and the mean improvement was 4.59 points (95% CI, 3.97-5.20).
The mean (SD) improvement was 4.93 (2.88) in female patients and 5.86 (2.29) in male patients, without statistically significant differences between the groups (P=0.13).
As for lesion color, the mean (SD) improvement was 6.05 (2.81) for pink lesions, 6.38 (2.36) for red lesions, and 3.66 (1.82) for violaceous lesions. Statistically significant differences were found, respectively, between the groups with violaceous and pink malformations (P=0.006) and between the groups with violaceous and red malformations (P<0.001), but not between the groups with pink and red malformations (P=0.89).
Greater mean (SD) improvement was observed in patients with hypertrophy (4.57 [2.25]) than in patients without hypertrophy (6.38 [2.68]), and the difference between the groups was statistically significant (P=0.003).
As for lesion size, the mean (SD) improvement was 2.88 (2.21) in patients with lesions measuring <3cm, 5.25 (2.58) in patients with lesions measuring 3-10cm, and 5.84 (2.51) in patients with lesions measuring >10cm. There were statistically significant differences between patients with malformations measuring <3cm and those with lesions measuring >10cm (P=0.03); no statistically significant differences were found between patients with lesions measuring <3cm and those with lesions measuring 3-10cm (P=0.13) nor between the latter group and patients with malformations measuring >10cm (P=0.68).
Table 1 summarizes the statistical results.
Mean, Standard Deviation, and P Value Between Study Groups.
| Study Group | Mean | Standard Deviation | P Value Between Groups |
|---|---|---|---|
| Patients before treatment | 10 | 0 | <0.001 |
| Patients after treatment | 5.41 | 2.61 | |
| Male patients (after treatment) | 5.86 | 2.29 | 0.13 |
| Female patients (after treatment) | 4.93 | 2.88 | |
| Without hypertrophy (after treatment) | 6.38 | 2.68 | 0.003 |
| With hypertrophy (after treatment) | 4.57 | 2.25 | |
| Red lesions (after treatment) | 6.38 | 2.36 | <0.001 |
| Pink lesions (after treatment) | 6.05 | 2.81 | |
| Violaceous lesions (after treatment) | 3.66 | 1.82 | |
| Lesions measuring <3cm (after treatment) | 2.88 | 2.21 | 0.02 |
| Lesions measuring 3-10cm (after treatment) | 5.25 | 2.58 | |
| Lesions measuring >10cm (after treatment) | 5.84 | 2.51 | |
Adverse effects were seen in 19 patients (26.76%), the most frequent (n=13, 18.31%) being skin atrophy—usually mild—in certain areas. Skin atrophy throughout the treated area occurred in 2 patients (2.82%), transient crusting after some treatment sessions in 2 patients (2.82%), pigmentary changes, generally transient, in 3 patients (4.22%), and focal ulceration after some treatment sessions in 1 patient (1.41%).
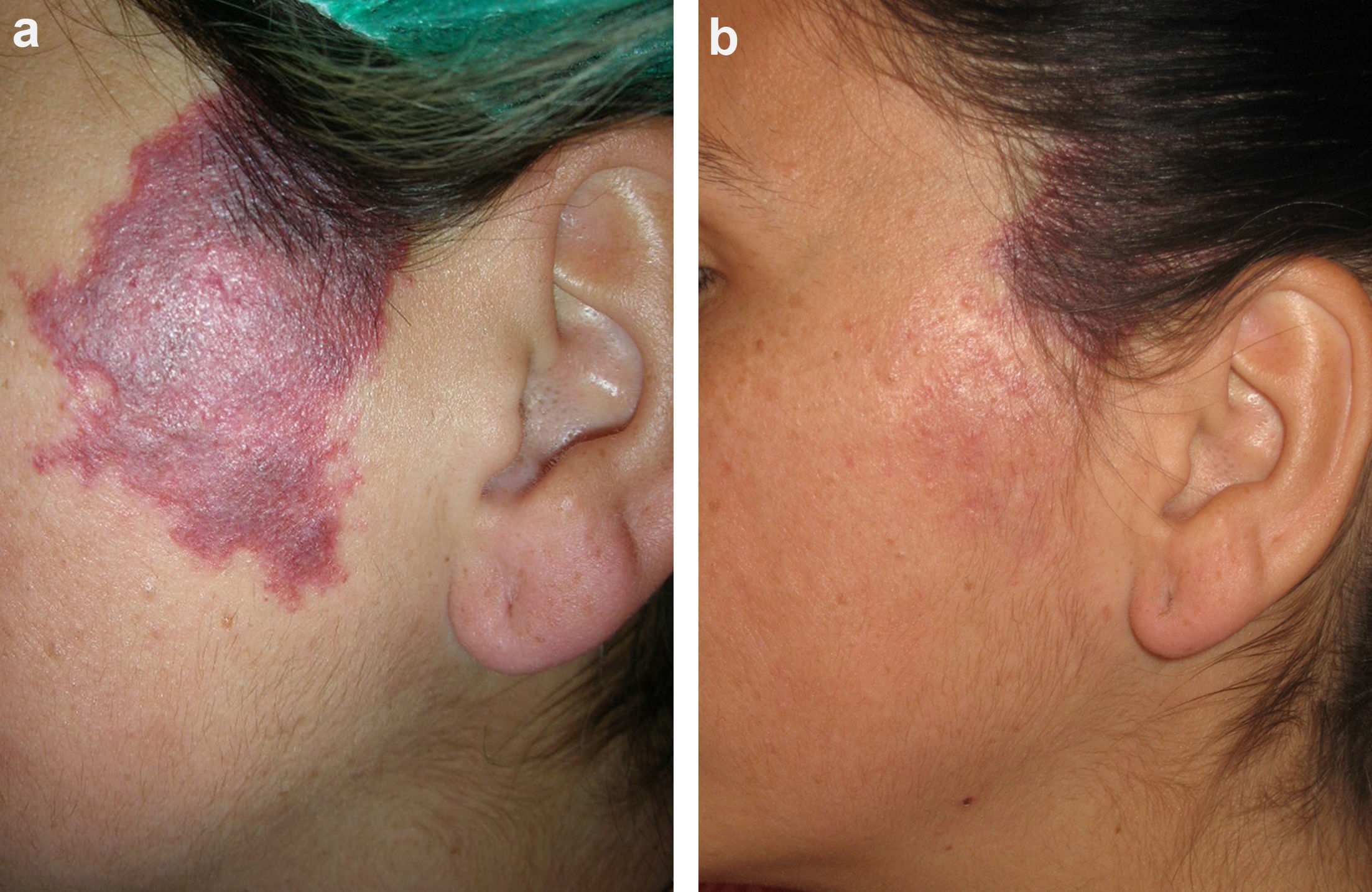
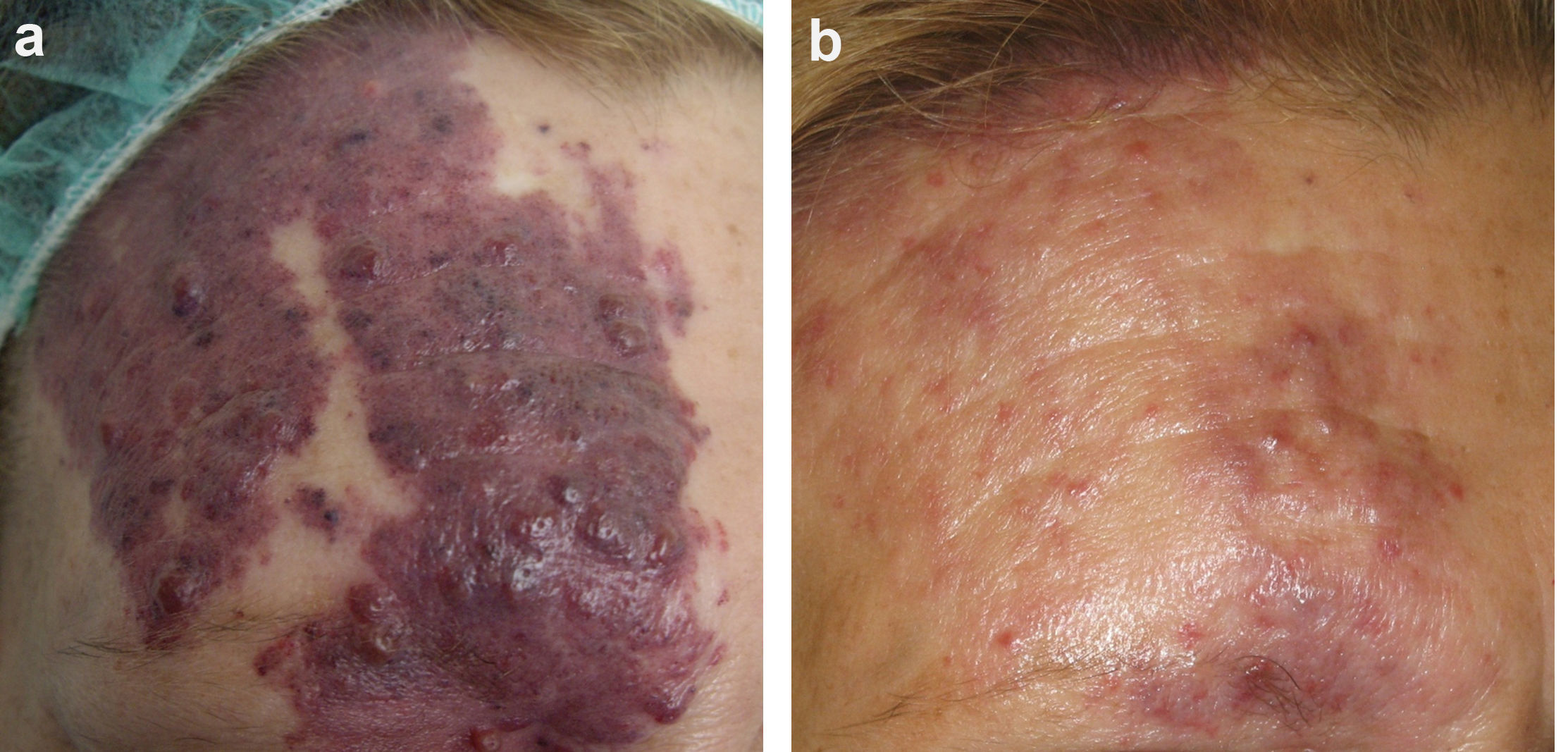
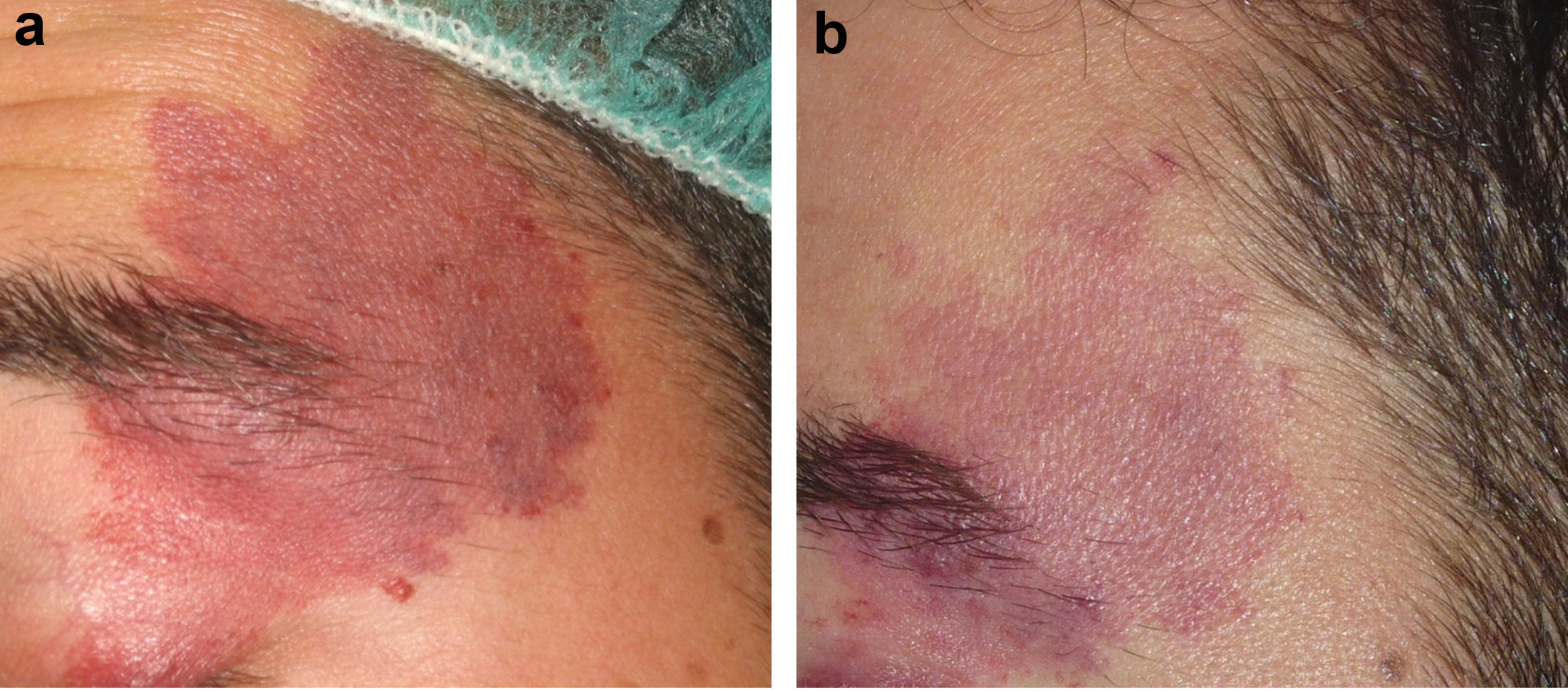
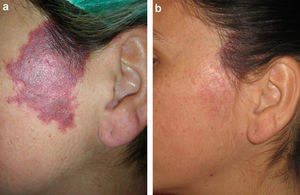
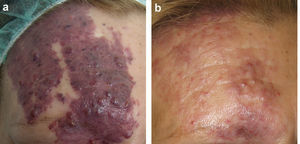
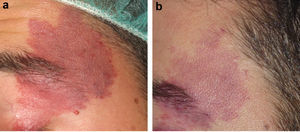
Figs. 1-3 show the responses achieved in some of the patients.
In the years since Anderson and Parrish proposed the theory of selective photothermolysis, PDL has become the first-line option for treating capillary malformations.18 However, complete lesion clearance is only achieved in approximately 20% of patients treated with PDL, while 20-30% of patients see little or no improvement.19
There are various reasons why PDL is unable to completely destroy the ectatic capillaries of these lesions, including insufficient penetration, chromophore scarcity in the capillaries of small-caliber vessels, limited pulse duration, the use of inadequate fluence, and posttreatment revascularization and neoangiogenesis.
Because of these disadvantages, various alternatives have been used, including other light sources such as the Nd:YAG laser, which has been used successfully to treat capillary malformations with a marked hypertrophic component,2–4 although adverse effects are more common with Nd:YAG laser than with PDL.
Sequential application of a 595nm PDL followed by a 1064nm Nd:YAG laser has been shown to be effective at treating venous malformations,20 angiolymphoid hyperplasia with eosinophilia,21 and infantile hemangiomas.22 The response obtained with sequential application is due to the fact that PDL and Nd:YAG lasers have a depth of penetration of approximately 1mm and 5-6mm, respectively, and therefore reach structures at different dermal layers. Furthermore, PDL is used first. This reduces the oxygenated hemoglobin in the red blood cells to methemoglobin, causing a 3-fold to 5-fold increase in hemoglobin absorption by the Nd:YAG laser and making it possible to set the Nd:YAG laser at a lower fluence, thereby reducing the associated pain and edema.23–25 This approach can theoretically reduce the adverse effects associated with the use of Nd:YAG lasers as monotherapy because higher fluences could increase the risk of atrophy and unattractive scarring associated with the loss of vascular selectivity.
In our study, we treated 71 patients with dual-wavelength pulses from a PDL and a Nd:YAG laser; most had previously been treated with other therapies until no further clearance could be obtained.
In our series, statistically significant improvement after treatment was achieved in the entire group of patients. Furthermore, we identified several predictors of better treatment response. Violaceous lesions had a significantly better response, and the presence of hypertrophy was also associated with greater improvement. Finally, lesions with a maximum diameter of <3cm responded better to treatment than lesions measuring >10cm.
Adverse effects occurred with moderate frequency (25.76%). In most cases, these effects were mild, the most common being mild skin atrophy in certain areas. However, we believe that this is an acceptable risk because most of these patients had not responded to other therapies and the overall result—taking into account improvement as well as adverse effects—was favorable.
In the literature reviewed, we found only 1 study similar to ours.26 In that study, dual-wavelength PDL and Nd:YAG laser therapy was used to treat 25 patients with hypertrophic capillary malformations that were refractory to treatment with PDL. Moderate improvement was seen in 12 patients and slight improvement in 13 patients. Adverse effects included mild purpura (which is nearly inevitable after effective treatment) and, in 1 patient, the formation of vesicles, which resolved in 6 days without sequelae.
Although that study used a different assessment system and is therefore difficult to compare with our study, we believe that our results are slightly more promising. It is important to note that the other study included patients with capillary malformations that were either hypertrophic or refractory to PDL, whereas our study was limited to patients with hypertrophic capillary malformations and included some patients who had not been treated previously. However, we do not believe that the possibly greater degree of clearance achieved in our study can be attributed exclusively to this difference, since patients with hypertrophic malformations had the best response in our study. It is possible that there were slight differences in the parameters used for each patient and that each physician's experience may have played a role in this.
Our study had various limitations, including those typical of a retrospective, uncontrolled study. It is also possible that the efficacy of the treatment may have been influenced by certain variables not analyzed in this study: age, number of sessions, history of previous treatment, and use of topical anesthesia (although, on the basis of our experience and previous findings, we do not believe that this last factor alters efficacy).27,28
We therefore consider that dual-wavelength sequential pulses from a PDL and a Nd:YAG laser is effective at treating capillary malformations. Despite not being considered the treatment of choice, this option could be considered in certain patients with lesions that are refractory to the usual treatment. It would be interesting to carry out a comparative study with Nd:YAG laser monotherapy in order to determine which treatment has a better efficacy and safety profile.
Ethical DisclosuresProtection of persons and animalsThe authors declare that the procedures followed complied with the ethical standards of the corresponding human experimentation committee and the World Medical Association and with the principles of the Declaration of Helsinki.
Data confidentialityThe authors declare that they followed their hospital's regulations regarding the publication of patient information.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects referred to in this article. This document is in the possession of the corresponding author.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Alcántara-González J, Boixeda P, Truchuelo-Díez MT, Jiménez-Gómez N, Pérez-García B, Pérez-Carmona L, et al. Malformaciones capilares tratadas con aplicación secuencial de láser de colorante pulsado y Nd:YAG: estudio retrospectivo. Actas Dermosifiliogr. 2018;109:155–161.