A 51-year-old man with no relevant personal or family history presented to our dermatology department with a lesion on the scalp that had appeared 8 years earlier and had been biopsied at another center 4 years previously. The histologic diagnosis was compatible with granulomatous dermatitis with eosinophilia, resulting from arthropod bites. However, at the original consultation and again when he consulted our department, the patient denied any prior history of trauma or insect bite. In recent months the lesion had increased in size and occasionally gave rise to itching, despite no change in the original morphologic features. There were no associated systemic symptoms.
Physical ExaminationThe patient presented a well-defined, slightly raised annular lesion, measuring 3x3.5cm, with an atrophic appearance and superficial telangiectases (Fig. 1). There were no palpable locoregional lymph nodes.
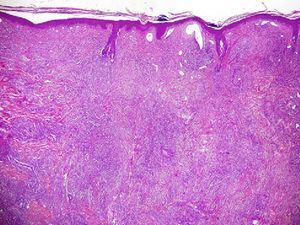
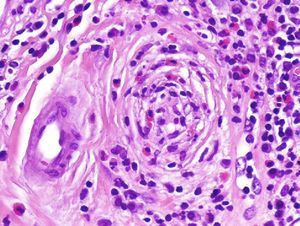
HistologyHistopathology showed a moderately atrophic epidermis, with an abundant inflammatory infiltrate characterized by polymorphism in the mid to deep dermis (Fig. 2). It contained neutrophils, eosinophils, and lymphocytes and was particularly intense in periadnexal regions (Fig. 3).
Additional TestsThe results of additional tests (complete blood count, routine biochemistry, thyroid function tests, autoimmune studies, serology for syphilis, chest x-ray, Mantoux test) were within the normal range.
What Is Your Diagnosis?
DiagnosisExtrafacial granuloma faciale.
Clinical Course and TreatmentTreatment with twice daily applications of tacrolimus ointment 0.1% achieved a moderate response at 3 months after diagnosis.
CommentExtrafacial granuloma faciale is a dermatosis of unknown origin that can present as a single or multiple lesion; the clinical course is slow and progressive. An extrafacial site is extremely rare and fewer than 30 cases have been reported in the literature.1
When the lesion is extrafacial, the most common sites are the trunk, upper and lower limbs, and the scalp. In fact, it is not uncommon for facial lesions to precede the development of others at extrafacial sites. Clinically, lesions are usually well-demarcated papules, plaques, or nodules.
There is no generally accepted pathophysiological hypothesis. However, UV radiation appears to be involved, as most cases are found in the facial region in middle-aged to elderly patients with high cumulative sun exposure or even chronic sun-induced damage. Other authors propose an immunologic etiology for this disorder, postulating a delayed hypersensitivity reaction or vasculitis mediated by immune complexes.2
The histopathologic characteristics of extrafacial granuloma faciale have been widely described and include a normal or moderately atrophied epidermis. Almost all cases are characterized by a well-demarcated Grenz zone and a polymorphous inflammatory infiltrate rich in eosinophils and arranged in a distinctive periadnexal and vascular pattern. Extrafacial granuloma faciale shares common features with erythema elevatum diutinum. Both conditions involve what Carlson and LeBoit called chronic fibrosing vasculitis, although the presence of this histologic feature will depend on the stage of evolution of the lesion because the initial stages point to classic leukocytoclastic vasculitis.3,4
Caldarola et al5 have recently contributed to furthering our knowledge of extrafacial granuloma faciale by defining its dermoscopic pattern. A uniform grayish-white background with whitish streaks reveals elongated vascular loops, whose morphology varies significantly after treatment with tacrolimus. The pattern is not specific to this condition and is found in others such as sarcoidosis and lupus.
Treatment of extrafacial granuloma faciale is complicated and often ineffective and there is no first-line therapy or well-defined therapeutic pathways. Some authors have reported a good response to topical tacrolimus,5,6 which is emerging as the treatment of choice because of its good risk-benefit profile. Other interesting options include intralesional corticosteroids, dapsone, cryosurgery, and pulsed dye laser, although recurrence is common after discontinuation of treatment.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Galán-Gutiérrez M, et al. Placa atrófica en cuero cabelludo de 8 años de evolución. Actas Dermosifiliogr. 2013;104:161–2.