Alopecic and aseptic nodules of the scalp (AANS), also known as pseudocyst of the scalp, is a new, little known, and probably underdiagnosed entity.
AANS was first described in the Japanese literature in 1992.1 The condition was described as pseudocyst of the scalp because histologic examination revealed cyst-like cavities lacking a true cystic wall.1 The first cases in Western populations were reported by Chevallier and coworkers2 in 1998, who described the lesions as non-infectious and alopecic scalp abscesses. In 2009, Abdennader and colleagues introduced the term “alopecic and aseptic nodules of the scalp”, as they failed to consistently find the cystic cavities described in the Japanese studies.3,4 About 70 cases have been described to date; these are listed in Table 1.
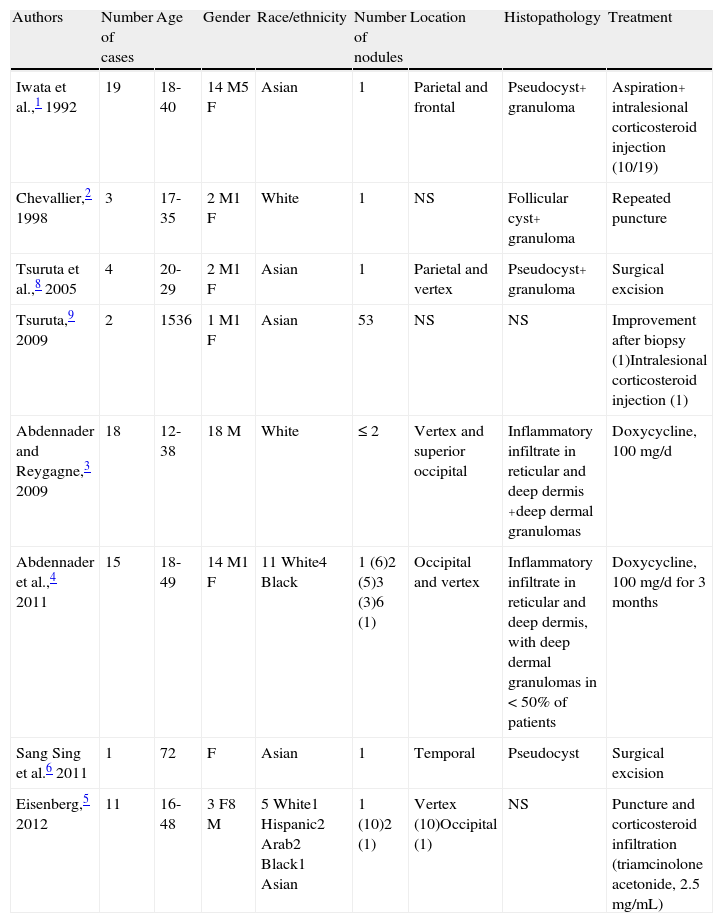
Summary of the Main Features of this Entity Described in the Literature.
| Authors | Number of cases | Age | Gender | Race/ethnicity | Number of nodules | Location | Histopathology | Treatment |
| Iwata et al.,1 1992 | 19 | 18-40 | 14 M5 F | Asian | 1 | Parietal and frontal | Pseudocyst+ granuloma | Aspiration+ intralesional corticosteroid injection (10/19) |
| Chevallier,2 1998 | 3 | 17-35 | 2 M1 F | White | 1 | NS | Follicular cyst+ granuloma | Repeated puncture |
| Tsuruta et al.,8 2005 | 4 | 20-29 | 2 M1 F | Asian | 1 | Parietal and vertex | Pseudocyst+ granuloma | Surgical excision |
| Tsuruta,9 2009 | 2 | 1536 | 1 M1 F | Asian | 53 | NS | NS | Improvement after biopsy (1)Intralesional corticosteroid injection (1) |
| Abdennader and Reygagne,3 2009 | 18 | 12-38 | 18 M | White | ≤ 2 | Vertex and superior occipital | Inflammatory infiltrate in reticular and deep dermis +deep dermal granulomas | Doxycycline, 100 mg/d |
| Abdennader et al.,4 2011 | 15 | 18-49 | 14 M1 F | 11 White4 Black | 1 (6)2 (5)3 (3)6 (1) | Occipital and vertex | Inflammatory infiltrate in reticular and deep dermis, with deep dermal granulomas in < 50% of patients | Doxycycline, 100 mg/d for 3 months |
| Sang Sing et al.6 2011 | 1 | 72 | F | Asian | 1 | Temporal | Pseudocyst | Surgical excision |
| Eisenberg,5 2012 | 11 | 16-48 | 3 F8 M | 5 White1 Hispanic2 Arab2 Black1 Asian | 1 (10)2 (1) | Vertex (10)Occipital (1) | NS | Puncture and corticosteroid infiltration (triamcinolone acetonide, 2.5 mg/mL) |
We are aware of the following 3 articles published in the Japanese literature, the originals of which are unavailable: Nukaga Y, Matsuura K, Matsushima Y. A case of pseudocyst of the scalp. Hifu Rinsho (Tokyo). 1995;37:1772-1773; Shibagaki N, Sugiyama H, Ohtake N, Furue M, Shimada S. Analysis of 3 cases of inflammatory granulomatous nodule with pseudocyst associated with follicular occlusion triad -Pseudocystic granuloma of skin. Jpn J Clin Dermatol. 1996, 50:105-110; Aiba S, Mukai H. Pseudocyst of the scalp. Pract Dermatol. 2002;24:893-6.
Abbreviation: NS, Not specified.
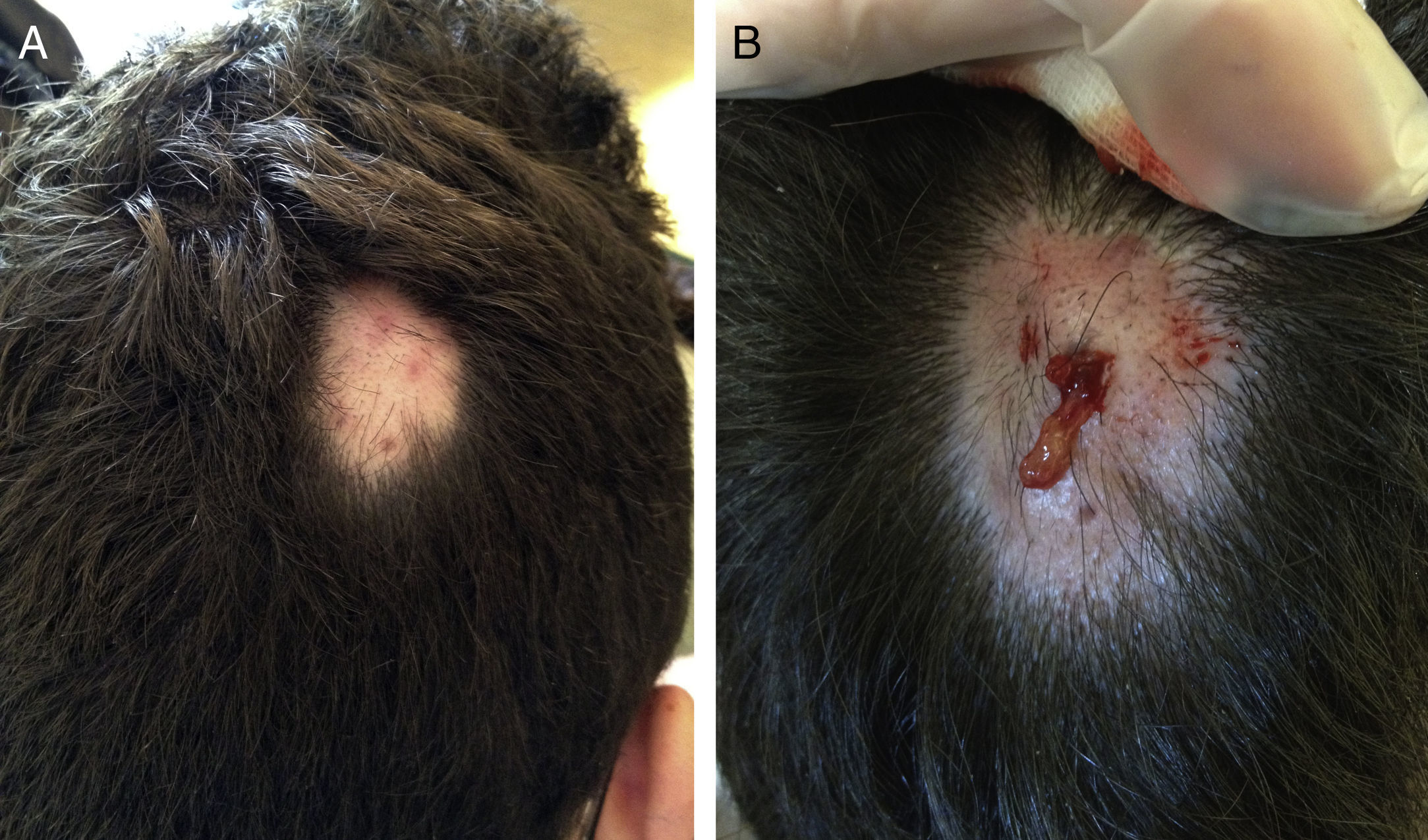
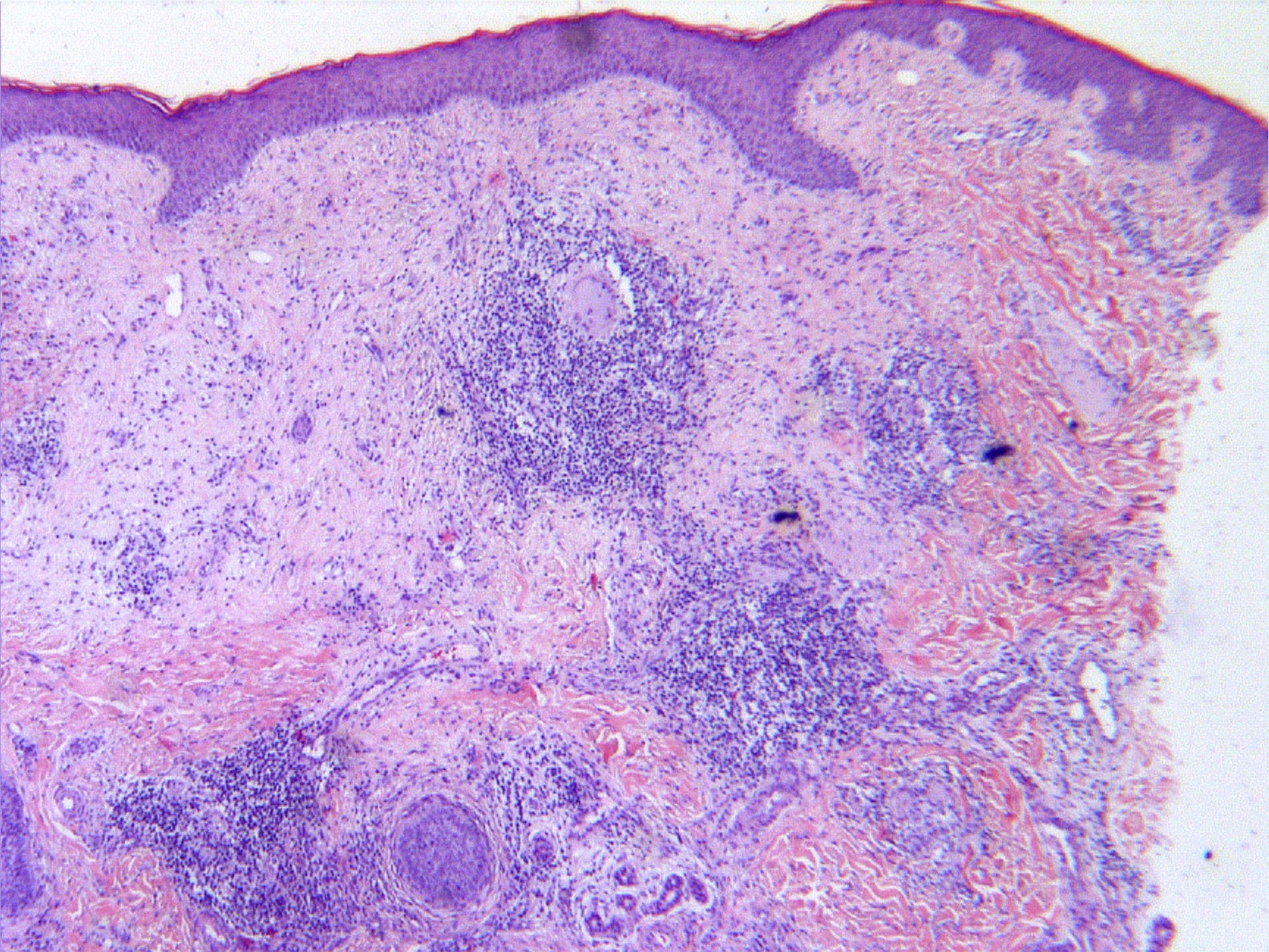
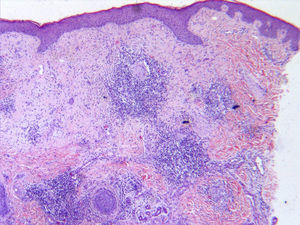
We report the case of a 16 year-old male with an asymptomatic alopecic plaque on the right parietal region of the scalp. A soft, domed, erythematous, and slightly alopecic nodule of 3cm in diameter surrounded by normal scalp was palpable on examination (Fig. 1). Biopsy showed an inflammatory lesion in the mid and deep dermis composed of granulation tissue, edema, reactive angioproliferation, and non-confluent granulomas, some with giant cells and others with central abscess formation (Fig. 2). Specific staining for microorganisms with Periodic acid Schiff (PAS), silver, Giemsa, and Ziehl-Neelsen was negative, as were mycological and bacteriological cultures. Treatment was initiated with doxycycline (100mg/d). Puncture of the lesion 2 weeks later revealed a yellowish orange material. After completing 2 months of treatment, the lesion resolved without scarring alopecia. No recurrence was observed after 5 months.
Histopathology: inflammatory lesion in the mid and deep dermis consisting of granulation tissue, edema, reactive angioproliferation, and mixed inflammatory infiltrate, with non-confluent granulomas, some with giant cells and others with central abscess formation (hematoxylin eosin, original magnification ×20).
This condition most often affects young males and presents as alopecic, dome-shaped nodules surrounded by normal skin; it can be asymptomatic or cause occasional discomfort.2,4 Hair loss coincides with the formation of the nodules, which are located mainly at the vertex, but can occur in any area of the scalp. Usually 1 to 2 nodules develop as an isolated event, although some cases involve recurring nodules5; the nodules heal without causing scarring alopecia.
When material is obtained on puncturing the nodule, it can be serous, purulent, or yellowish, depending on the characteristics of the infiltrate and the type of vessel eroded by the infiltrate; yellow indicates erosion of a lymph vessel, as in the present case; pink indicates erosion of a blood vessel; and purulent material indicates the predominance of polymorphonuclear infiltrate.4 Cultures are negative in all cases.
Histologically these nodules exhibit mixed inflammatory infiltrates (lymphocytes, histiocytes, and giant cells) and in most cases granulomas in the deep dermis or pseudocyst-like architecture without a true wall. Histological differences are thought to be due to race-related differences in hair type or the comparison of superficial with nonsuperficial samples.4
These nodules respond well to treatment with doxycycline (100mg/d),4 intralesional corticosteroids,5 and aspiration or drainage of the nodule.2 Cases of spontaneous regression have been described,5 and in general surgical excision is not necessary.
While the etiology of AANS is unknown, it is considered to be a type of deep folliculitis secondary to follicular occlusion or a foreign body reaction. It is characterized by a granulomatous reaction with inflammatory infiltrate composed of lymphocytes, histiocytes, and giant cells. Subsequent central necrosis and erosion of blood and lymph vessels results in exudate production and pseudocyst formation. Some authors have suggested that AANS may lie within the spectrum of diseases associated with follicular occlusion, although immunological processes cannot be ruled out.3,6
Differential diagnosis with superinfected trichilemmal cyst, alopecia areata, bacterial and dermatophyte folliculitis, metastasis, and dissecting cellulitis should be established. Dissecting cellulitis, unlike AANS, presents clinically as multiple, painful, erythematous nodules, which form abscesses that fistulize and cause scarring alopecia.7
We agree with Abdennader and coworkers that alopecic and aseptic nodules of the scalp and pseudocyst of the scalp are the same entity, the former being a more appropriate name, as the nodules are always alopecic, the material obtained on puncturing the nodule is sterile, and histopathology does not always reveal pseudocysts.4 However, Sang Sing and coworkers6 argue that the 2 are distinct conditions, as biopsies reveal pseudocysts in the latter but not in the former.
In conclusion, AANS is an emerging entity in the literature, is relatively unknown, and thus is likely underdiagnosed. It is diagnosed by the presence of alopecic, aseptic nodules on the scalp and the absence of scarring alopecia. In general, it is easily managed and responds well to treatment. A better understanding of this condition is necessary for proper treatment and to avoid unnecessary interventions.
We thank Dr. Roger Llatjos and Dr. Valeri Novell of the Pathology Laboratory, BCN Patòlegs, Barcelona.
Please cite this article as: Fischer-Levancini C, Iglesias-Sancho M, Collgros H, Sánchez-Regaña. M. Nódulos asépticos y alopécicos del cuero cabelludo. Actas Dermosifiliogr. 2014;105:208–211.