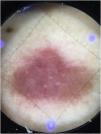
An 80-year-old woman, with no relevant past medical or surgical history presented to the Dermatology Department with an 8-month history lesion on her back that had shown slow, progressive growth. On physical examination, a single 2cm×1.5cm erythematous-violaceous papule, firm to palpation, was observed in the thoracolumbar region (Fig. 1).
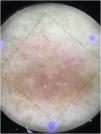
What is your diagnosis?A non-contact dermoscopic examination revealed the presence of white circles and lines along with arborizing vessels on a salmon-colored background (Fig. 2), which turned yellowish when contact dermoscopy was performed (Fig. 3).
During dermoscopic examination, the observation of orange-yellowish areas and branching linear vessels initially suggested a differential diagnosis with granulomatous lesions. However, given the patient's age, trunk location, and the presence of a single lesion, a cutaneous lymphoma was considered the most likely diagnosis, prompting an excisional biopsy.
Histopathologic examination revealed the presence a neoplastic infiltration of lymphoid lineage (Fig. 4) with a clonal rearrangement of the IgH gene. The staging study turned out negative.
Therefore, a diagnosis of primary cutaneous marginal zone lymphoma (PCMZL) was established. After complete excision, the patient remained asymptomatic and free of systemic disease to date.
PCMZL is a primary cutaneous B-cell lymphoma (PCBCL) that typically affects middle-aged adults and is slightly more frequent in men. Its usual clinical presentation consists of erythematous-violaceous papules, plaques, or nodules located on the trunk or extremities, characterized by slow growth.
Histologically, a nodular or diffuse neoplastic proliferation is observed in the reticular dermis. The involved cells are B lymphocytes that do not express CD5 and cyclin D1 antigens (markers of small mantle-zone lymphocytes), CD10 antigen (characteristic of follicle center lymphomas), and often also lack the CD23 antigen expression (a marker of chronic lymphocytic leukemia cells).
Clinical diagnosis can be challenging due to variability in presentation, rarity of the disease, and its clinical resemblance to more common cutaneous disorders.1 Dermoscopy, therefore, may facilitate an initial presumptive diagnosis.
Piccolo et al. conducted an initial study correlating dermoscopy and histopathology in 10 cases of PCBCL, all described clinically as solitary erythematous-violaceous nodules (two of them PCMZL). They found that the dermoscopic pattern differed from other diseases with similar clinical features, typically showing white circles on a salmon-orange background, often accompanied by scales and arborizing vessels. The arborizing vessels were smaller and less sharply focused than those seen in basal cell carcinoma.2
Subsequently, Geller et al. analyzed 58 dermoscopic images of PCBCL, identifying most frequently a salmon-colored background (79.3%) and prominent blood vessels (77.6%), mostly arborizing in morphology (67.2%).3 These findings were further supported by isolated reports and small case series.4,5
A later retrospective study compared dermoscopic features of primary cutaneous lymphomas of nodular/plaque type with clinically similar mimickers such as pseudolymphomas, tumors, and inflammatory lesions, identifying structureless salmon-colored areas and focal whitish structures as the main dermoscopic predictors of these lymphomas.6
In conclusion, although dermoscopic findings are not specific, dermoscopy is a harmless and accessible tool with significant value for the initial diagnostic approach to PCBCL. The main diagnostic clues include a salmon-colored background with white areas or circles and arborizing vessels.
Conflicts of interestThe authors declare no conflicts of interest.