Many patients admitted to hospital by doctors other than dermatologists have skin disease in addition to the illness that caused hospitalization; this leads to a considerable number of interdepartmental dermatology consultations. While some of these referrals produce significant changes in the patient's diagnosis, treatment, and prognosis, others are completely unrelated to the patient's principal disease.
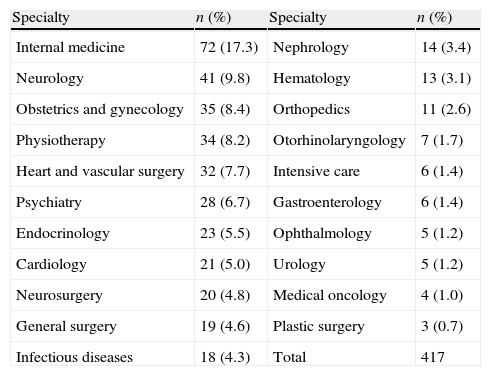
We retrospectively analyzed 417 interdepartmental consultations to dermatology from a 5-month period in a tertiary hospital, the İzmir Atatürk Training and Research Hospital (IATRH) in İzmir, Turkey. No pediatric referrals were included. The male to female ratio of the patients was 1,16 and the average age at the time of consultation was 56.13 years. The most common referrals were from the internal medicine department (17%), followed by the neurology (9%) and obstetrics and gynecology (8%) departments. The distribution of consultations according to specialty is shown in Table 1.
Distribution of referrals according to specialty.
| Specialty | n (%) | Specialty | n (%) |
| Internal medicine | 72 (17.3) | Nephrology | 14 (3.4) |
| Neurology | 41 (9.8) | Hematology | 13 (3.1) |
| Obstetrics and gynecology | 35 (8.4) | Orthopedics | 11 (2.6) |
| Physiotherapy | 34 (8.2) | Otorhinolaryngology | 7 (1.7) |
| Heart and vascular surgery | 32 (7.7) | Intensive care | 6 (1.4) |
| Psychiatry | 28 (6.7) | Gastroenterology | 6 (1.4) |
| Endocrinology | 23 (5.5) | Ophthalmology | 5 (1.2) |
| Cardiology | 21 (5.0) | Urology | 5 (1.2) |
| Neurosurgery | 20 (4.8) | Medical oncology | 4 (1.0) |
| General surgery | 19 (4.6) | Plastic surgery | 3 (0.7) |
| Infectious diseases | 18 (4.3) | Total | 417 |
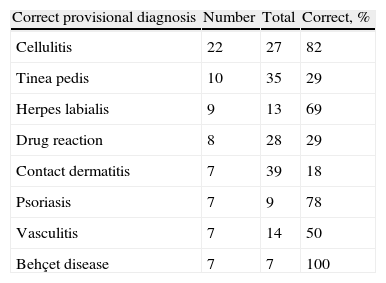
The interdepartmental consultation forms submitted by the relevant specialist teams were often incomplete. The reason for hospital admission was missing from a third of these forms. The description of the skin lesions was either incorrect or absent on 87% of the forms; and when the lesions were described, lay terms were often used instead of specifying the elementary lesions. A dermatologic differential diagnosis was submitted in only 45% of cases, and in only 29% (122/417) was the provisional dermatologic diagnosis considered correct after evaluation by a dermatologist. In similar studies, a correct provisional dermatologic diagnosis was reported in 23.9% by Davila,1 25% by Adışen,2 38% by Falanga,3 39% by Walia,4 and 45% by Ahmad.5
A correct provisional diagnosis by the referring specialty was most common in cases of infectious disease, such as cellulitis, tinea pedis, and herpes labialis, followed by drug reactions and contact dermatitis. The provisional diagnoses most frequently correct are listed in Table 2.
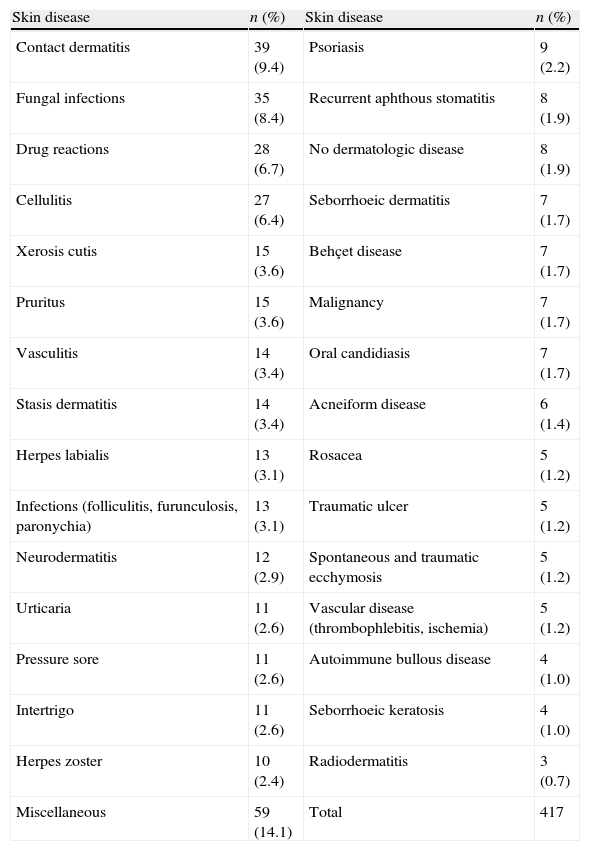
The most common diagnoses proposed by dermatology staff were contact dermatitis (39 cases, 9.4%), fungal infection (35 cases, 8.4%), drug reactions (28 cases, 6.7%), and cellulitis (27 cases, 6.4%). In similar studies, the most common diagnoses were dermatitis, drug reactions, and dermatophyte and herpes infections.1–4,6–8 The dermatologic diagnoses of the 417 patients are shown in Table 3.
Dermatologist's diagnosis.
| Skin disease | n (%) | Skin disease | n (%) |
| Contact dermatitis | 39 (9.4) | Psoriasis | 9 (2.2) |
| Fungal infections | 35 (8.4) | Recurrent aphthous stomatitis | 8 (1.9) |
| Drug reactions | 28 (6.7) | No dermatologic disease | 8 (1.9) |
| Cellulitis | 27 (6.4) | Seborrhoeic dermatitis | 7 (1.7) |
| Xerosis cutis | 15 (3.6) | Behçet disease | 7 (1.7) |
| Pruritus | 15 (3.6) | Malignancy | 7 (1.7) |
| Vasculitis | 14 (3.4) | Oral candidiasis | 7 (1.7) |
| Stasis dermatitis | 14 (3.4) | Acneiform disease | 6 (1.4) |
| Herpes labialis | 13 (3.1) | Rosacea | 5 (1.2) |
| Infections (folliculitis, furunculosis, paronychia) | 13 (3.1) | Traumatic ulcer | 5 (1.2) |
| Neurodermatitis | 12 (2.9) | Spontaneous and traumatic ecchymosis | 5 (1.2) |
| Urticaria | 11 (2.6) | Vascular disease (thrombophlebitis, ischemia) | 5 (1.2) |
| Pressure sore | 11 (2.6) | Autoimmune bullous disease | 4 (1.0) |
| Intertrigo | 11 (2.6) | Seborrhoeic keratosis | 4 (1.0) |
| Herpes zoster | 10 (2.4) | Radiodermatitis | 3 (0.7) |
| Miscellaneous | 59 (14.1) | Total | 417 |
The problem that led to the dermatology referral was present before the patient's admission in 66% of cases. Most consultations (71.5%) were found to be unrelated to the disease causing hospital admission. A total of 119 (28.5%) referrals were defined as relevant because the dermatologic disease was considered to be related to the patient's principal disease or to its treatment; the diagnosis of the patient's principal disease was reached as a direct result of the dermatology consultation in 59 of these 119 patients, the treatment of the principal disease was determined on the basis of dermatology consultation in 30, and the established treatment was changed in 30 because of complications of the previous treatments.
The dermatological opinion was an aid to the diagnosis and/or treatment of the patient's principal disease in 89 cases. For example, after the dermatology consultation, a patient under investigation by neurologists for ophthalmoplegia of unknown etiology was diagnosed with motor neuron involvement by herpes zoster. In another patient, unnecessary surgery was avoided by the accurate diagnosis of herpes zoster causing unbearable abdominal pain.
Dermatological examination was sufficient to reach the diagnosis in most of the referrals. However, laboratory tests were required to make the final diagnosis in 67 (16%) patients. Skin biopsies were performed in 8.2% of cases; this was lower than the rate reported by Davila1 (20%) but higher than the rate described by Adışen (4.4%).2
In our experience, common dermatologic diseases are often not correctly diagnosed by physicians from other specialties. In addition, there is room for improvement in the formal description and in the differential diagnosis of skin diseases. Expert dermatologic assessment usually facilitates inpatient diagnosis and management. Better training should be considered for medical students and residents and possibly even for medical staff in other specialties.
Please cite this article as: Özyurt S, Kelekçi KH¸ Şeremet S, Özçelik S. Analysis of Inpatient Dermatologic Consultations. Actas Dermosifiliogr. 2014;105:799–800.