Psoriasis is associated with high treatment costs due to the increasing use of biologic drugs. Phototherapy has been demonstrated to be safe and cost effective for the treatment of psoriasis, although it is limited by the requirement for patients to visit a hospital various times a week.
ObjectivesTo evaluate the efficiency of home-based phototherapy with narrow-band UV-B radiation compared with biologic drugs for the treatment of moderate to severe psoriasis under normal practice conditions in our setting.
MethodsA retrospective cost-effectiveness study was undertaken in 12 patients with moderate to severe psoriasis. Half of the patients were treated with biologic drugs (2 with etanercept, 2 with adalimumab, and 2 with infliximab) and the other half with home-based phototherapy using a Waldmann UV100 TL-01 lamp. Clinical effectiveness was determined on the basis of achieving a 75% improvement in Psoriasis Area and Severity Index (PASI-75) within 16 weeks of treatment.
ResultsTreatment was considered to be effective in 5 out of 6 patients (83%) treated with biologics and 4 out of 6 patients (66%) treated with home-based phototherapy. The direct costs required to achieve PASI-75 were 8256€ per patient for biologics and 903€ per patient for home-based phototherapy. The costs associated with effective treatment using biologic drugs in a single patient would provide effective home-based phototherapy for 9.1 patients.
LimitationsThe study included a limited number of patients analyzed over a short time period (16 weeks) and the comparison group included multiple treatments with different predicted responses.
ConclusionsAlthough biologic drugs exhibited greater efficacy, home-based phototherapy was more efficient for the treatment of moderate to severe psoriasis. Home-based phototherapy represents a cost-effective treatment option for patients with psoriasis and may be appropriate for use in the Spanish health care system.
La psoriasis ocasiona un elevado coste terapéutico debido a la creciente utilización de los fármacos biológicos. La fototerapia ha demostrado ser un tratamiento seguro y coste-efectivo para la psoriasis, aunque presenta la limitación del desplazamiento del paciente varios días en semana a un centro hospitalario.
ObjetivosEvaluar la eficiencia de la fototerapia domiciliaria con ultravioleta B de banda estrecha frente a los fármacos biológicos en el tratamiento de la psoriasis moderada-grave en condiciones reales de nuestro entorno.
MétodosEstudio de evaluación económica de coste-efectividad, con carácter retrospectivo, sobre 12 pacientes con psoriasis moderada-grave. La mitad recibió tratamiento con fármacos biológicos—dos etanercept, dos adalimumab y dos infliximab—y la otra mitad recibió fototerapia en su domicilio con una lámpara Waldmann UV100L-T. La medida de efectividad clínica fue la obtención de un PASI-75 antes de la semana 16 de tratamiento.
ResultadosEn 5 de 6 pacientes (83%) con terapia biológica y en 4 de 6 pacientes (66%) con fototerapia domiciliaria el tratamiento fue efectivo. Los costes directos por PASI-75 alcanzado fueron de 8.256 euros para los biológicos y de 903 euros para la fototerapia domiciliaria. Con el coste requerido para que un fármaco biológico fuera efectivo en un único paciente podía obtenerse respuesta en 9,1 pacientes tratados con fototerapia domiciliaria.
LimitacionesNúmero reducido de pacientes, horizonte temporal limitado a 16 semanas, grupo de comparación heterogéneo, con fármacos de perspectivas de respuesta diferente.
ConclusionesA pesar de que los fármacos biológicos presentaron una mayor efectividad, la fototerapia domiciliaria fue más eficiente para el tratamiento de la psoriasis moderada-grave. La fototerapia domiciliaria representa una alternativa terapéutica coste-efectiva para los pacientes con psoriasis con potencial aplicación en nuestro sistema sanitario.
Psoriasis is a chronic inflammatory skin disease of unknown etiology characterized by recurrent outbreaks. It is a prevalent disorder that affects between 1% and 2% of the population,1,2 and 5% to 10% of those affected have moderate to severe forms of the disease.3 While no definition of moderate to severe psoriasis has been universally accepted, a recent Spanish consensus document defined it as psoriasis that requires (or has previously required) systemic therapy with conventional drugs, a biologic agent, phototherapy, or photochemotherapy.1 The same consensus document specified that systemic treatment is indicated in patients who meet the following criteria: disease not controlled with topical treatment; extensive disease (body surface area affected≥5%–10%); Psoriasis Area Severity Index PASI≥10; rapid worsening; involvement of visible areas; functional impairment (palmoplantar or genital involvement); subjective perception of severity (Dermatology Life Quality Index>10); extensive erythroderma or pustular psoriasis; or disease associated with psoriatic joint disease.
The therapeutic arsenal available to treat psoriasis includes phototherapy, various topical treatments, the classic systemic treatments (acitretin, methotrexate, and ciclosporin), and the modern biologic agents (etanercept, adalimumab, infliximab, and ustekinumab). Given the high prevalence of the disorder and the development of new therapies, such as the biologic agents, the cost associated with the treatment of patients with moderate to severe psoriasis has increased dramatically in recent years.4,5
At the same time, there has been a decline in the prescription of phototherapy, despite the fact that this therapeutic option has been shown to be both safe and cost-effective.6–9 One of the main reasons for this decline appears to be that patients find it difficult to attend the outpatient clinic for phototherapy sessions 3 or 4 days a week because of the loss of work time, and consequently of income, involved. Most of these logistic drawbacks can be overcome by home-based phototherapy, that is, by the patients carrying out the phototherapy sessions in a controlled manner in their own home. Several studies have shown home phototherapy to be an inexpensive, safe, and effective treatment for psoriasis.4,10–13 However, this treatment modality has not yet been used in the Spanish public health care system.
ObjectiveThe aim of this study was to assess the efficiency of narrowband UV-B phototherapy administered in the home to treat moderate to severe psoriasis under normal practice conditions in our setting, and to compare it with that of biologic drug therapy.
Materials and MethodsWe designed a cost-effectiveness study to analyze the efficiency of home narrowband UV-B phototherapy and biologic agents (etanercept, adalimumab, and infliximab) for the treatment of moderate to severe psoriasis. Using hospital funding, our dermatology department acquired 3 home phototherapy units; the patients bore no part of the cost of this acquisition.
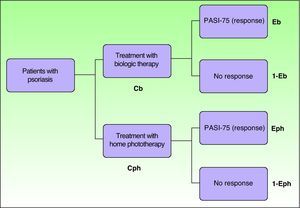
Study Type and General InformationThis was a retrospective cost-effectiveness study carried out in the psoriasis unit of a tertiary hospital between September 2009 and September 2010 to compare home narrowband UV-B phototherapy with biologic therapy. Decision trees were constructed (Fig. 1) to calculate the direct costs, effectiveness, and efficiency (cost/effectiveness) of the 2 types of treatment studied (home phototherapy and biologic therapy with etanercept, adalimumab and infliximab). As the analysis was carried out from the payer's perspective, it only took into account direct costs. Consequently, we calculated the cost to the Spanish National Health Service of providing home phototherapy or biologic therapy to these patients. The treatment period stipulated for both therapeutic options was 4 months. It was not necessary to apply a discount rate for future costs and results because both the cost and the effective outcomes occurred within a maximum of 4 months.
Simplified model of the decision tree used. Cb indicates cost of biologic therapy; Cph, cost of phototherapy; Eb, probability of PASI-75 response with biologic therapy; Eph, probability of PASI-75 response with phototherapy; 1-Eb, probability of no PASI-75 response to biologic therapy; 1-Eph, probability of no PASI-75 response to phototherapy. Incremental cost-effectiveness of the biologic therapy=(Cb−Cph)/ (Eb−Eph).
Twelve patients were included retrospectively, including the first 6 patients treated with home phototherapy and the first 2 patients treated with each of the 3 biologic agents (etanercept, adalimumab, and infliximab) after the dermatology department acquired the home phototherapy units. The choice of treatment (home phototherapy or a biologic agent) was made on the basis of clinical criteria, without randomization. The inclusion criteria for all treatments were moderate to severe psoriasis (PASI>10) and prior treatment with at least 1 systemic therapy (psoralen-UV-A [PUVA], methotrexate, or ciclosporin) or intolerance of or inability to receive such treatments (contraindications or inability to attend the outpatient clinic for PUVA sessions). Patients were excluded if they had joint disease or contraindications for biologic drugs or phototherapy.
Treatment With Biologic AgentsTreatment with biologic agents was administered according to the treatment regimens14 specified in the Summary of Product Characteristics authorized by the Spanish Agency for Medicines and Health Products for the treatment of moderate to severe psoriasis (Table 1): etanercept, 50mg twice a week for 12 weeks followed by 50mg once a week; adalimumab, 80mg loading dose at week 0, 40mg at week 1, followed by 40mg every 2 weeks; and infliximab, 5mg/kg intravenously at weeks 0, 2, 6, and 14. The recommended screening protocol was followed prior to treatment with biologics (Table 2). All patients receiving biologic therapy attended the hospital for assessment 5 times during the 4-month study period (an initial consultation and 4 follow-up visits).
Characteristics of the Patients Treated With Biologic Agents or Home Narrowband UV-B Phototherapy.
| Biologic Agent | Dosage | Sex, Age (Weight) | Prior Treatmenta | Baseline PASI | Time to PASI-75 | Adverse Events |
| 1. Etanercept | 50mg twice weekly for 12 weeks and 50mg/wk thereafter | W, 41 (68kg) | MTX (not effective) | 11.8 | 4 months | |
| 2. Etanercept | 50mg twice weekly for 12 weeks and 50mg/wk thereafter | M, 39 (77kg) | CSP (nephrotoxicity) | 12.2 | Not achieved | Local reaction |
| 3. Adalimumab | 80mg initial dose, 40mg at week 1 and every other week thereafter | M, 48 (74kg) | MTX (not effective) | 10.2 | 4 months | |
| 4. Adalimumab | 80mg initial dose, 40mg at week 1 and every other week thereafter | M, 42 (84kg) | PUVA (not effective) | 12.4 | 4 months | |
| 5. Infliximab | 5mg/kg IV at weeks 0, 2, 6, and 14 | M, 50 (105kg) | PUVA, CSP (nephrotoxicity) | 15.5 | 2 months | Flu-like syndrome |
| 6. Infliximab | 5mg/kg IV weeks 0, 2, 6 and 14 | M, 45 (82kg) | PUVA, MTX (gastrointestinal side effects) | 13.8 | 2 months |
| Phototherapy | ProtocolInitial Dose, No. of Sessions, TCD, (Treatment Regimen) | Sex, Age (Skin Phototype) | Prior Treatmenta | Baseline PASI | Time to PASI-75 | Adverse Events |
| 1. Home phototherapy | 0.25J/cm2, 90 sessions, 98J, (3 ays’ treatment and 1 ay off) | M, 33 (III) | PUVA (not compatible with work) | 15.2 | 4 months | Mild erythema at start of treatment |
| 2. Home phototherapy | 0.15J/cm2, 78 sessions, 43J, (2 days’ treatment and 1 day off) | M, 29 (II) | PUVA (not compatible with work) | 10.8 | Not achieved | |
| 3. Home phototherapy | 0.20J/cm2, 80 sessions, 56J (2 days’ treatment and 1 day off) | M, 38 (III) | MTX (not effective) | 11.4 | 4 months | Pruritus |
| 4. Home phototherapy | 0.20J/cm2, 60 sessions, 33J, (2 days’ treatment and 1 day off) | W, 41 (III) | MTX (gastrointestinal side effects) | 10.2 | 2 monthsb | |
| 5. Home phototherapy | 0.20J/cm2, 62 sessions, 38J, (2 days’ treatment and 1 day off) | W, 42 (III) | PUVA (not compatible with work) | 10.8 | 2 monthsb | |
| 6. Home phototherapy | 0.15J/cm2, 82 sessions, 45J, (2 days’ treatment and 1 day off) | M, 46 (II) | Acitretin (elevated transaminases) | 11.2 | Not achieved |
Abbreviations: CSP, ciclosporin; M, man; MTX, methotrexate; PUVA, psoralen plus UV-A therapy; TCD, total cumulative dose; W, woman.
Cost of Additional Tests Required Prior to Biologic Therapy.
| Additional Tests | Cost € |
| Mantoux test with booster | 30 |
| Laboratory workup including complete blood count, biochemistry, liver function tests and lipid analysis | 21 |
| HIV, HBV, and HCV serology | 216 |
| Antinuclear antibodies | 43 |
| Chest radiograph | 18 |
| Total | 328 |
Abbreviations: HBC, hepatitis B virus; HCV, hepatitis C virus; HIV, human immunodeficiency virus.
The phototherapy device used was a Waldmann UV 100 T-L home phototherapy unit (Fig. 2). The lamp was delivered to the patient's home by a delivery service company, remained there for the duration of treatment, and was collected at the end of treatment by the same company. No additional tests were performed before or during phototherapy. Each patient received 30minutes of training. This comprised a 10-minute session given by the physician in the dermatology office and 20minutes instruction on how to use the phototherapy unit given by the nurse, who also explained the need to protect the eyes and genitals. During the treatment sessions, patients protected their eyes with dark glasses and shielded their genitals with dark-colored underwear. The number of sessions prescribed depended on the patient's initial PASI score: patients with a PASI under 15 were prescribed a continuous regimen of 2 days of treatment followed by 1 day off, and patients with a PASI score above 15 followed a regimen of 3 days of treatment followed by 1 day off. Phototherapy sessions were continued for 16 weeks or until the patient achieved a 90% improvement in their PASI score (PASI-90); no maintenance regimen was used. All patients receiving phototherapy attended the hospital for assessment 5 times during the 4-month study period (an initial consultation and 4 follow-up visits).
The phototherapy dose was calculated for each patient on the basis of their Fitzpatrick skin phototype (the so-called American protocol)7,15: an initial dose of 0.20J/cm2 for phototype II and an initial dose of 0.25J/cm2 for phototype III. The dose was increased by 20% in each of the first 3 sessions and by 10% thereafter.
Measure of EffectivenessEffectiveness was determined on the basis of PASI scores. The specific indicator of effectiveness was a PASI-75 (75% improvement over the baseline score) at week 16. To compare the effectiveness of biologic therapy and home phototherapy, we calculated the incremental effectiveness, that is, the gain in terms of the proportion of patients who achieved a PASI-75 response with the biologic therapy compared to with home phototherapy. In Fig. 1 this is represented as Eb–Eph.
Cost Assessment and Statistical AnalysisWe calculated the direct cost of treatment in euro. In the case of biologic therapy, this included the cost of the drugs, consultations, and screening tests. In the case of home phototherapy, it included the cost of the phototherapy unit, delivery and collection of the unit, consultations, and tests. The unit cost of the drugs was calculated on the basis of the average price invoiced, and this information was obtained from the hospital's medication management system (Gestowin).
The unit cost of follow-up visits was obtained from the annual cost breakdown provided by the hospital management. The cost of a consultation was calculated on the basis of the total annual cost and the number of days used.
The cost of each home phototherapy machine was calculated on the basis of the price invoiced by the manufacturer. It was assumed that each unit would have a useful life of 10 years (a low estimate according to data provided by the supplier). The maintenance cost was based on data provided by the vendor and included the possible replacement of tubes and radiometric controls annually. Transport costs were based on the carrier's invoice in each case. No installation costs were included because all that was required was to plug the home phototherapy unit into the electrical system in the home.
The measure of cost-effectiveness was the cost per PASI-75 achieved. The cost of achieving a PASI-75 response was calculated by dividing the total cost in all patients by the number of patients who achieved this response. In the incremental cost-effectiveness ratio used, the denominator was the incremental effectiveness and the numerator was the cost associated with the gain (the difference in cost between the 2 treatments compared). The formula used was as follows: (cost of biologic therapy−cost of phototherapy)/(effectiveness of biologic therapy−effectiveness of phototherapy). This formula is shown in Fig. 1 as (Cb–Cph)/(Eb–Eph).
Since the analysis was conducted from the payer's perspective, it did not take into account indirect costs (lost productivity and absence from work), intangible costs (pain, suffering), or direct nonmedical costs (cost of travel to the consultation, for example).
We analyzed the robustness of our results using deterministic sensitivity analysis based on 3 scenarios (worst case, base case, and best case) constructed by introducing a 15% variation into the critical variables of effectiveness and cost.
Statistical analysis was performed using version 18.0 of the Statistical Package for Social Sciences (SPSS Inc.) software. Medians and interquartile range (P25-P75) were calculated for the variables that did not display a Gaussian distribution. The nonparametric Mann Whitney test was used to analyze the homogeneity of the 2 treatment groups. Values of P<.05 were considered to be statistically significant.
ResultsPatientsThe characteristics of the patients in the 2 groups are shown in Table 1. Six patients treated with biologic agents were evaluated: 2 received etanercept, 2 adalimumab, and 2 infliximab (5 men and 1 woman; mean age, 44 years). Six patients treated with home phototherapy were evaluated (4 men and 2 women, mean age 41 years). The median baseline PASI was 12.3 (P25-P75, 11.4–14.2) in the biologic therapy group and 11.0 (P25-P75, 10.7–12.4) in the home phototherapy group. No statistically significant differences were found between the 2 groups in median baseline PASI (Mann–Whitney U>.05), indicating that, in this respect, the 2 groups were homogeneous.
EffectivenessPASI-75 was achieved within 4 months in 5 of the 6 patients (83%) on biologic therapy and 4 of the 6 patients (66%) who received home phototherapy (Figs. 3 and 4). The median (P25-P75) PASI of the group treated with biologic agents was 4.2 (1.3–4.9) at 2 months and 1.8 (0–2.9) at 4 months. The median (P25-P75) PASI of the group treated with home phototherapy was 6.0 (2.3–7.7) at 2 months and 2.3 (0–4.2) at 4 months. The mean time to PASI-75 was 2.8 months for the 5 patients receiving biologic therapy who achieved this result and 3 months in the 4 patients treated with home phototherapy in whom the treatment was effective.
Adverse events were mild in both groups and the incidence was similar (33%). The adverse events reported by the patients treated with biologic agents were injection-site reactions with etanercept and flu-like symptoms with infliximab. Adverse reactions reported by the patients treated with home phototherapy were mild erythema at the start of therapy and itching.
CostsThe cost of the biologic drugs was as follows: €223 for a 50mg syringe of etanercept; €486 for a 40mg pen of adalimumab; and €515 for a 100mg vial of infliximab. The cost of an initial consultation was €96 and the cost of each follow-up visit was €58. The cost of using the day hospital for 3hours to administer infliximab was estimated at €102 per session. The cost of the screening performed prior to biologic therapy was €328 (Table 2).
Each home phototherapy unit cost €3560. The annual cost of each unit was calculated as €356 based on an estimated average life span of 10 years, a low estimate according to data provided by the supplier. Since each patient had the unit for 4 months, the cost per patient was €118. Maintenance costs, including the possible replacement of tubes and radiometric controls annually, were estimated at €2000 over the 10-year life of the unit (€200 per year). Thus the maintenance cost per patient for each 4-month period was €67. The cost of delivering and collecting the unit from the patient's home was €120 per patient. Therefore, the overall cost associated with the provision of home phototherapy to each patient was €305 (the cost of the phototherapy unit+maintenance+transport).
The direct costs related to biologic therapy and home phototherapy are shown in Tables 3 and 4.
Cost Associated With Biologic Therapy.
| Treatment | Number of Doses Received | Cost of Drug€ | Total CostVisits+Tests | Total CostDrug+Tests | Total Cost to Achieve PASI-75 | |
| Unit Price | Total | € | € | |||
| 1. Etanercept | 28–50mg | 223 (50mg) | 6259 | 719 | 6978 | 6978 |
| 2. Etanercept | 28–50mg | 223 (50mg) | 6259 | 719 | 6978 | 6978 |
| 3. Adalimumab | 1× 80mg+8× 40mg | 486 (40mg) | 4862 | 719 | 5581 | 5581 |
| 4. Adalimumab | 1× 80mg+8× 40mg | 486 (40mg) | 4862 | 719 | 5581 | 5581 |
| 5. Infliximab | 4 doses of 500mg IV (patient's weight, 105kg) | 515 (100mg) | 10 301 | 1127 | 11 428 | 8853 |
| 6. Infliximab | 4 doses×400mg IV (patient's weight, 82kg) | 515 (100mg) | 8240 | 1127 | 9367 | 7307 |
| Average cost | 6.025 | 855 | 7652 | 6.880 | ||
Abbreviations: IV, intravenous; PASI, psoriasis area and severity index.
Costs Associated With Home Phototherapy.
| Treatment | Cost of Phototherapy Unit | Cost of Transport | Total CostVisits + Tests | Total Cost of Phototherapy | Total Cost to Achieve PASI-75 | |
| Lamp € | Maintenance € | € | € | € | ||
| 1. Home phototherapy | 118 | 67 | 120 | 328 | 633 | 633 |
| 2. Home phototherapy | 118 | 67 | 120 | 328 | 633 | 633 |
| 3. Home phototherapy | 118 | 67 | 120 | 328 | 633 | 633 |
| 4. Home phototherapy | 118 | 67 | 120 | 328 | 633 | 540a |
| 5. Home phototherapy | 118 | 67 | 120 | 328 | 633 | 540a |
| 6. Home phototherapy | 118 | 67 | 120 | 328 | 633 | 633 |
| Average | 118 | 67 | 120 | 328 | 633 | 602 |
Abbreviations: PASI, psoriasis area and severity index.
The expenditure per PASI-75 was €8256 for biologic therapy and €903 for home phototherapy (Table 5). The incremental cost-effectiveness ratio (Fig. 1) of biologic therapy compared to home phototherapy was €37668 per additional patient with a PASI-75 response (calculated as follows: [€41280–€3612]/[5 patients in the biologic group with PASI-75 – 4 patients in the phototherapy group with PASI-75]). The cost associated with effective treatment using biologic drugs in a single patient would provide effective home-based phototherapy for 9.1 patients.
Cost-effectiveness of Biologic Therapy and Home Phototherapy.
| Percentage of Patients Who Achieved PASI-75 | Total Cost€ | Average Cost€ | Cost perPASI-75 € | Incremental C-E ratio | |
| Biologic therapy | 83% (5/6 patients) | 41280 | 6880 | 8256 | – |
| Phototherapy | 66% (4/6 patients) | 3612 | 602 | 903 | – |
| Incremental analysis | 37668 | 6278 | 7353 | 37668 |
Abbreviation: C-E, cost-effectiveness.
The sensitivity analysis, in which effectiveness and cost were varied by 15%, showed a cost per PASI-75 with biologic drugs of €5848 in the best case (a reduction in the average cost of 15% and an effective response in 6/6 patients), €8256 in the base case (average cost and effectiveness in 5/6 patients), and €11868 in the worst case (average cost increased by 15% and an effective response in 4/6 patients). The cost of home phototherapy was €614 per PASI-75 in the best case scenario (average cost reduced by 15% and effective response in 5/6 patients), €903 in the base case scenario (average cost and effective response in 4/6 patients), and €1384 in the worst case scenario (average cost increased by 15% and effective response in 3/6 patients).
In an even more unfavorable scenario in which, due to accidental breakage of the lamp or more frequent replacement of the tubes, the useful life of the unit was 5 times shorter (2 years) and the maintenance costs 5 times higher (€1000 per year), and assuming the effectiveness of phototherapy was even lower (with only 2/6 patients achieving an effective response), the average cost per patient treated with phototherapy would be €1047, representing the cost of 4 months use of the lamp (€3560 amortized over 2 years; €1780/3) plus maintenance costs for the 4 months (€1000/3), plus €120 for transport. Assuming that the treatment was effective in only 2 of the 6 patients, the cost per PASI-75 would be €3141.
The robustness of our results is demonstrated by the sensitivity analysis, which shows home phototherapy to be more cost-effective than biologic therapy in all 3 scenarios: base case, worst case, and best case.
DiscussionBiologic drugs have revolutionized the treatment of psoriasis,1 achieving success rates at week 16 as high as 60% to 80% PASI-75.2,16 However, since these treatments are expensive and not without adverse effects,5,17 they are not generally considered to be a first-line option. The results of a safety study in 988 patients with psoriasis treated with biologic agents showed that these drugs were associated with various adverse events, including reactions to infliximab infusion (34%), abnormal laboratory test results (13%), and infections (12%).18 Efficiency studies report a cost per PASI-75 of €8013 for adalimumab and between €9370 and €17112 for the other biologic agents.19
Recent studies indicate an increase among Spanish dermatologists in the prescription of biologic agents for the treatment of psoriasis, with up to 23% of patients with moderate to severe psoriasis being prescribed a biologic agent.3 The resulting increase in medication costs in dermatology has raised questions about the cost-effectiveness of biologic therapies. For example, according to data from the health service for the Community of Madrid (SERMAS), the increase in the number of patients in the Madrid area receiving biologic agents for psoriasis has doubled the cost of treatment in this setting between 2007 and 2009 (299 patients at a cost of €5306951 in 2007, 504 patients at €8210160 in 2008, and 674 patients at €10801524 in 2009). This upward trend continued throughout 2010 (909 patients at a cost of €12204234).
While our study analyzed only a small number of patients, our findings with respect to the cost of achieving a PASI-75 with biologic therapy are in line with those reported in the literature.19
Phototherapy with narrowband UV-B at 311nm is a safe and effective treatment for patients with psoriasis.8,9 It is estimated that between 50% and 80% of patients achieve a PASI-75,6,7 and the remission rate of psoriasis 1 year after treatment has been reported to be around 38%.10 One variable that can improve the effectiveness of phototherapy is the frequency of sessions, and a regimen based on 5 sessions a week has been shown to be more effective than a regimen of 3 sessions a week, as long as the dose is increased gradually to avoid adverse effects.7,15
With respect to cost, Langan et al.20 determined the cost of narrowband UV-B phototherapy to be €325 for 2 years’ treatment with phototherapy, of which 70% was the cost of personnel. A more recent study estimated the annual cost of narrowband UV-B phototherapy, at $1734, to be lower than that of most other therapeutic options ($4235 for PUVA, $7768 for ciclosporin, $9163 for acitretin, $23538 for adalimumab, $23639 for infliximab, and $24439 for etanercept) except methotrexate, at $1197.5 Given that the average annual cost of biologic treatment for a patient with psoriasis is between €14000 and €18000,2,5,21 the much lower cost of phototherapy would appear to be a key consideration if we wish to optimize the efficiency of treatment in this very prevalent disease. In view of the striking difference in cost, it is remarkable that the number of patients being treated with biologic agents is growing steadily, while the number of patients being treated with UV-B is declining. One possible explanation for this phenomenon is that the chief barrier to phototherapy treatment for patients is the inconvenience and time involved in traveling to the hospital 3 to 4 days a week for treatment.22 Another factor may be that not all hospitals are equipped to offer phototherapy. Furthermore, the patient must bear the indirect costs associated with phototherapy, such as transportation costs, lost working hours, none of which are a factor in the case of biologic therapy. In many cases, all of these factors lead the dermatologist to choose biologic therapy, despite the fact that it is a much more costly option for the health care provider.
As a result, it appears that narrowband UV-B phototherapy, despite being an effective and efficient treatment, is underutilized for mainly logistic reasons.7 In order to overcome the limitations associated with phototherapy, the health care authorities in various Europe countries (Netherlands, United Kingdom) have recently changed their approach and shifted the location of phototherapy treatment to the patient's own home. Home phototherapy eliminates the main problems associated with outpatient phototherapy, namely, the lack of patient availability and the inconvenience of hospital visits.4,10,11
Home phototherapy has been shown to be a safe, effective, and inexpensive treatment for psoriasis.4,10,11 Adherence rates were higher for home phototherapy than oral acitretin in one study.23 Moreover, home phototherapy allows patients to increase the number of weekly sessions from 3 to 5, if necessary, to achieve increased treatment effectiveness without the inconvenience this would entail if they had to spend time traveling to and from the hospital for treatment. Narrowband UV-B phototherapy administered in the patient's home has been shown to be at least as effective in the treatment of psoriasis as the same therapy administered in an outpatient setting, and the total cost of treatment is the same in both cases.12
Despite being a safe and efficient therapeutic option, home phototherapy has not yet been used or regulated by the Spanish national health system. In some countries, there are other obstacles to home phototherapy treatment, including copayment by patients and the scant interest shown by health insurance companies in promoting this type of therapy,10 as well as difficulties in obtaining the lamps and the lack of the specific training needed to prescribe the therapy among dermatologists.24
Several authors have advocated home phototherapy as the treatment of choice for patients with psoriasis because of its efficiency, lower indirect costs, high patient satisfaction, and the increased adherence to treatment observed.10,22
One of the risks associated with home phototherapy is the possibility that the patient will misuse the lamp, a risk that can be minimized through minimal patient training on the operation of the unit.25 With respect to carcinogenicity, there is currently no evidence of an increased risk of skin tumors with narrowband UV-B therapy,26 while such an increase has been shown in the case of PUVA therapy. However, caution is recommended, and patients should not exceed 450 sessions. The total cumulative dose that would pose an increased risk of carcinogenesis has not yet been determined.27,28
The effectiveness of home phototherapy in our study (66%) is similar to that reported in the literature for outpatient phototherapy.6,7 There are very little data in the literature concerning the cost of home phototherapy. Koek et al.12 (the PLUTO study) reported an estimated cost of €800 per patient (of which €727 were direct costs) for an average treatment period of 17.6 weeks. Our analysis of the costs associated with home phototherapy (direct cost of €602 per patient) is the first published study on the cost of this modality in the Spanish health system and our findings are similar to those reported by Koek et al.12 The cost of home phototherapy is comparable to that of outpatient phototherapy.5,12 The advantage of the outpatient modality is that several patients can be treated each day with a single device, while in home phototherapy the lamp is used by only 1 patient during the whole treatment period. It is therefore our opinion that home phototherapy would be an interesting addition to outpatient phototherapy for use in certain patients, and that the outpatient modality would also continue to be useful.
The main limitation of our study was the small sample size (12 patients). However, the sizeable differences observed in the cost-effectiveness both in the base case scenario (cost per PASI-75 of €8256 for biologic therapy and €903 for home phototherapy) and between the best case scenario for biologic therapy and worst case scenario for home phototherapy (cost per PASI-75 of €5848 for biologic therapy and €3141 for home phototherapy) show home phototherapy to be a very attractive treatment option for patients with psoriasis. This hypothesis can be confirmed by larger studies. Other limitations of our study include the use of a 16-week time horizon (biologic drugs can achieve better effectiveness if measured through week 24) and the heterogeneity of the biologic therapy group, which included different drugs with differing response profiles.
The usefulness of biologic drugs in certain cases (severe psoriasis, very high PASI, and contraindications or resistance to other treatments) is not in question. Moreover, these drugs operate systemically decreasing inflammation, an effect not demonstrated with phototherapy. However, in view of the adverse events and the high cost associated with biologic therapy, we should use this treatment option with caution and consider treating patients with moderate to severe psoriasis and a moderate PASI with other alternatives, such as phototherapy (if possible) in view of its greater efficiency and good safety profile. It is interesting to note that the target patient groups for biologic agents and phototherapy appear to be different. In fact, the median PASI of patients prescribed biologic drugs in our study was slightly higher than that of the patients who received phototherapy. In recent years we have seen a gradual shift from the use of phototherapy to the prescription of biologic drugs in patients with moderate to severe psoriasis and a PASI between 10 and 15. This has occurred largely because biologic therapy is more convenient for the patient because, unlike phototherapy, it does not involve traveling to the hospital on a regular basis to receive treatment. In fact, the criterion for considering a patient as a candidate for biologic treatment is that he or she should have moderate to severe psoriasis and contraindications to or intolerance of other systemic therapies, including ciclosporin, methotrexate and PUVA; in practice, this often includes patients who are unable to travel to the hospital for PUVA therapy.2
In conclusion, our study represents the first experience of home phototherapy in the Spanish public health system and we have achieved excellent results in terms of efficiency. We do not advocate replacing treatment with biologic agents in patients who have severe psoriasis or extensive multiple resistance, but we do propose home phototherapy as an alternative option for patients with moderate psoriasis who are candidates for phototherapy but who have difficulty attending the outpatient clinic regularly for treatment.
ConclusionsAlthough the biologic drugs were more effective, the results of our pilot study indicate that home phototherapy was more efficient than biologic therapy in patients with moderate to severe psoriasis. Home-based phototherapy represents a cost-effective treatment for patients with psoriasis and may be appropriate for use in the Spanish health care system.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Vaño-Galván S, et al. Análisis coste-efectividad de la fotorerapia domiciliaria con ultraviolet B de banda estrecha frente a fármacos biológicos en el tratamiento de la psoriasis moderada-grave. Actas Dermosifiliogr. 2012;103:127–137.