The clinical distinction between basal cell carcinoma (BCC) and intradermal melanocytic nevus lesions on the face can be difficult, particularly in young patients or patients with multiple nevi. Dermoscopy is a useful tool for analyzing characteristic dermoscopic features of BCC, such as cartwheel structures, maple leaf–like areas, blue-gray nests and dots, and ulceration. It also reveals arborizing telangiectatic vessels and short curved vessels, which are typical of BCC, and comma vessels, which are typical of intradermal melanocytic nevi. It is, however, not always easy to distinguish between these 2 conditions, even when dermoscopy is used. We describe 2 facial lesions that posed a clinical and dermoscopic challenge in two 38-year-old patients; confocal microscopy showed separation between tumor nests and stroma and polarized nuclei, which are confocal microscopy features of basal cell carcinoma.
El diagnóstico clínico diferencial entre el epitelioma basocelular y el nevus melanocítico intradérmico facial puede ser a veces complicado, sobre todo en pacientes jóvenes o con múltiples nevus. La dermatoscopia es una herramienta útil que permite observar signos dermatoscópicos asociados a epitelioma como las ruedas de carro, las hojas de arce, los nidos y puntos azul grisáceos y la ulceración, además permite distinguir los vasos telangiéctasicos arboriformes y los vasos cortos curvados bien enfocados característicos de los epiteliomas basocelulares de los vasos en coma presentes en los nevus melanocíticos intradérmicos. Sin embargo, el diagnóstico diferencial clínico y dermatoscópico entre estas 2 afecciones dermatológicas puede ser complejo. Presentamos 2 lesiones faciales en 2 pacientes de 38 años de difícil diagnóstico clínico y dermatoscópico en los que la microscopia confocal mostró nidos celulares con separación entre los nidos y el estroma, y polarización de los núcleos de las células tumorales, que son signos confocales asociados a epitelioma basocelular.
Reflectance confocal microscopy (RCM) is an imaging technique that uses a laser as a source of light. The light generated is reflected by the different structures of the skin, which have different sizes and refractive indices, to produce a 2-dimensional digital image. Images are obtained in vivo and in real time and have a similar resolution to that of optical microscopy images. RCM is a very useful tool for clinically distinguishing between intradermal melanocytic nevus lesions and basal cell carcinoma (BCC) on the face.
Case 1A 39-year-old woman under follow-up for severe psoriasis being treated with ustekinumab, and with no other remarkable history, presented with a pigmented lesion on her left cheek. The lesion had been present for 10 years, but had become elevated from the skin surface in the last 3 months.
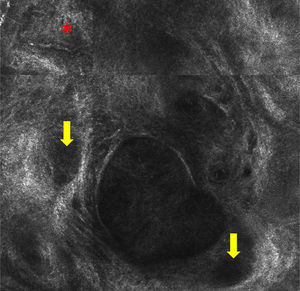
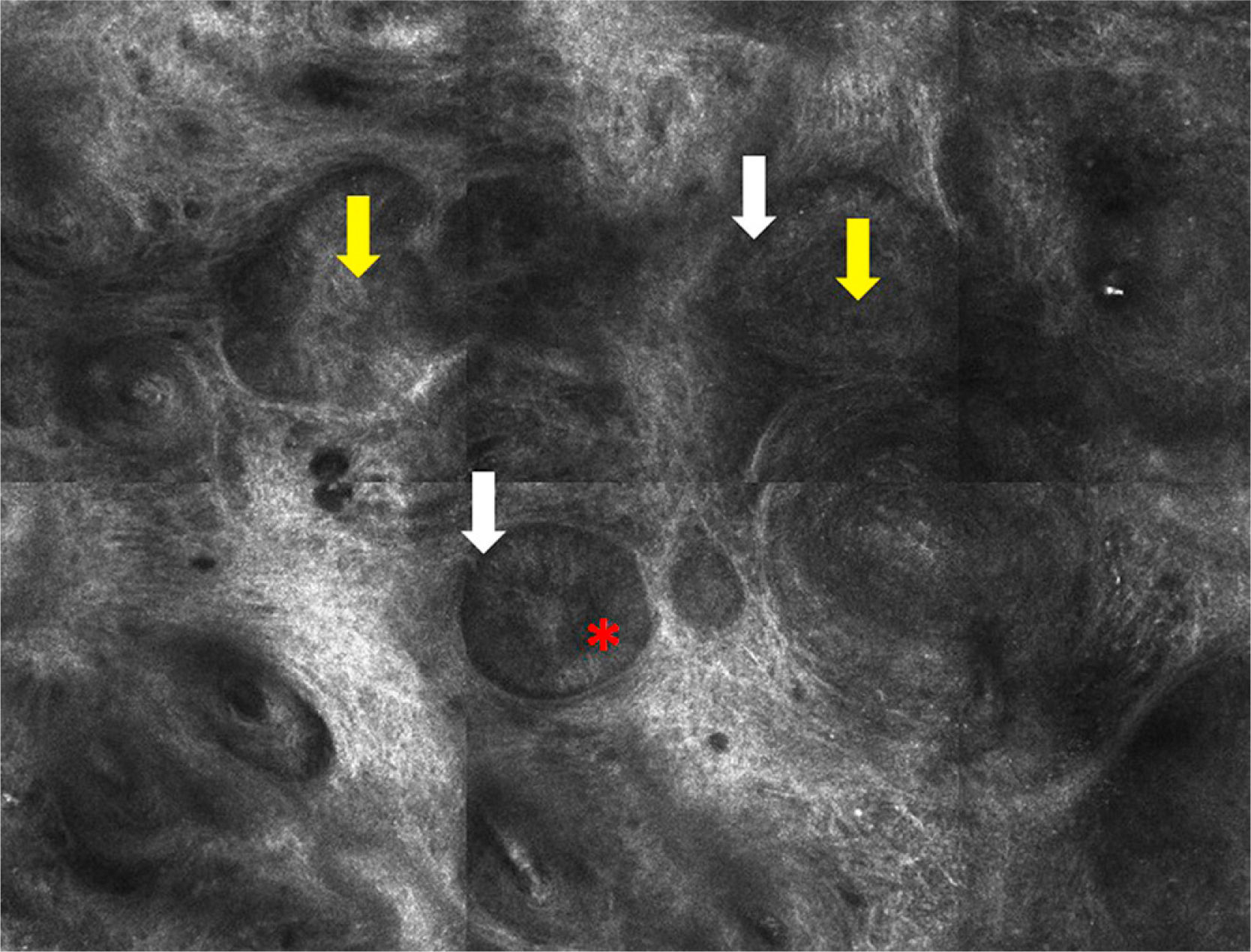
The only dermoscopic features observed were brown and gray oval structures (Fig. 1). Examination by RCM showed nests or islands of tumor cells separated from the stroma by dark spaces. Some of these tumor nests showed peripheral palisading, consisting of elongated nuclei arranged perpendicularly to the tumor lobules. There were refractive cells both inside and outside the nests (Fig. 2).
Histology confirmed a diagnosis of pigmented BCC with a micronodular pattern.
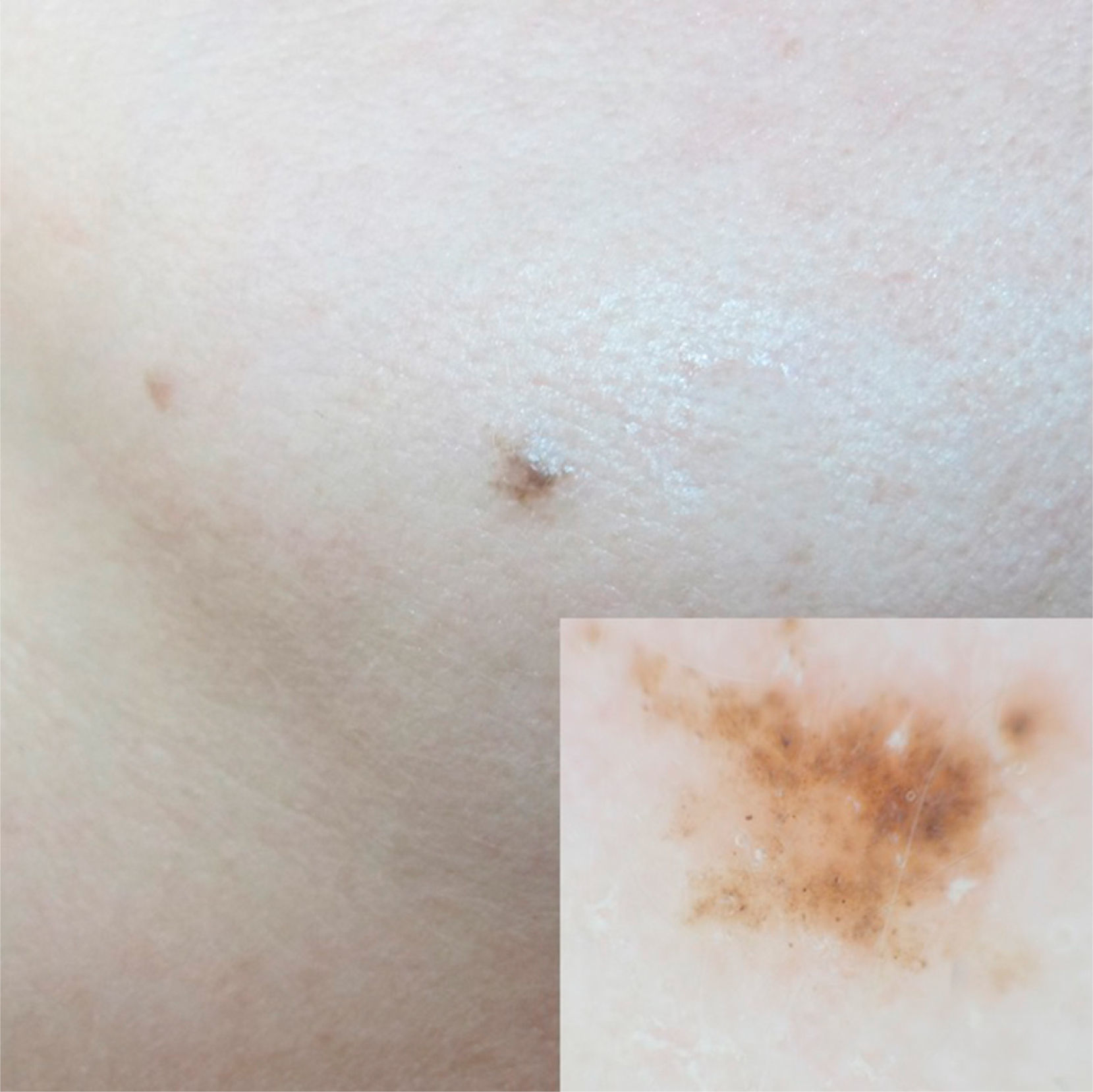
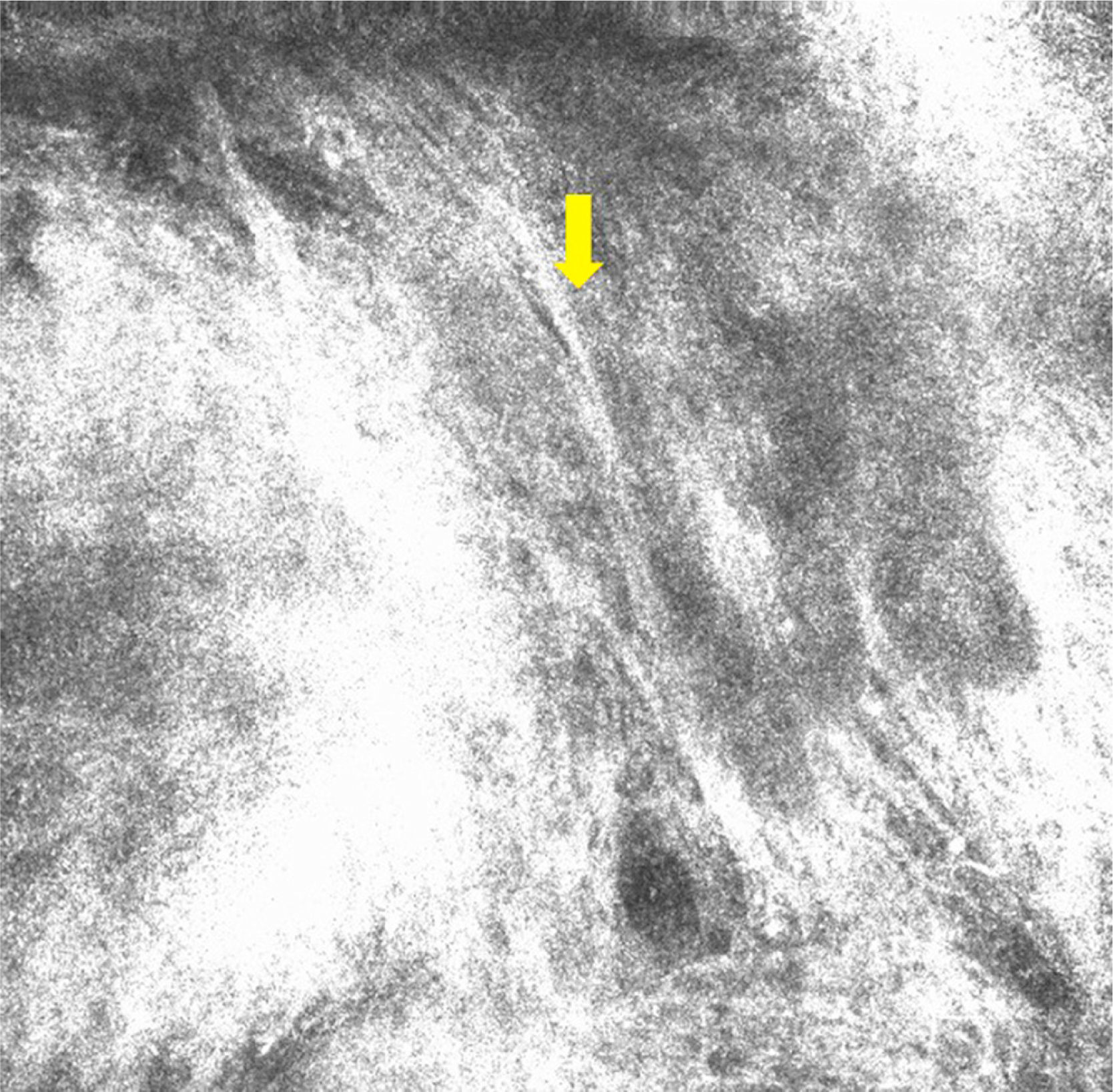
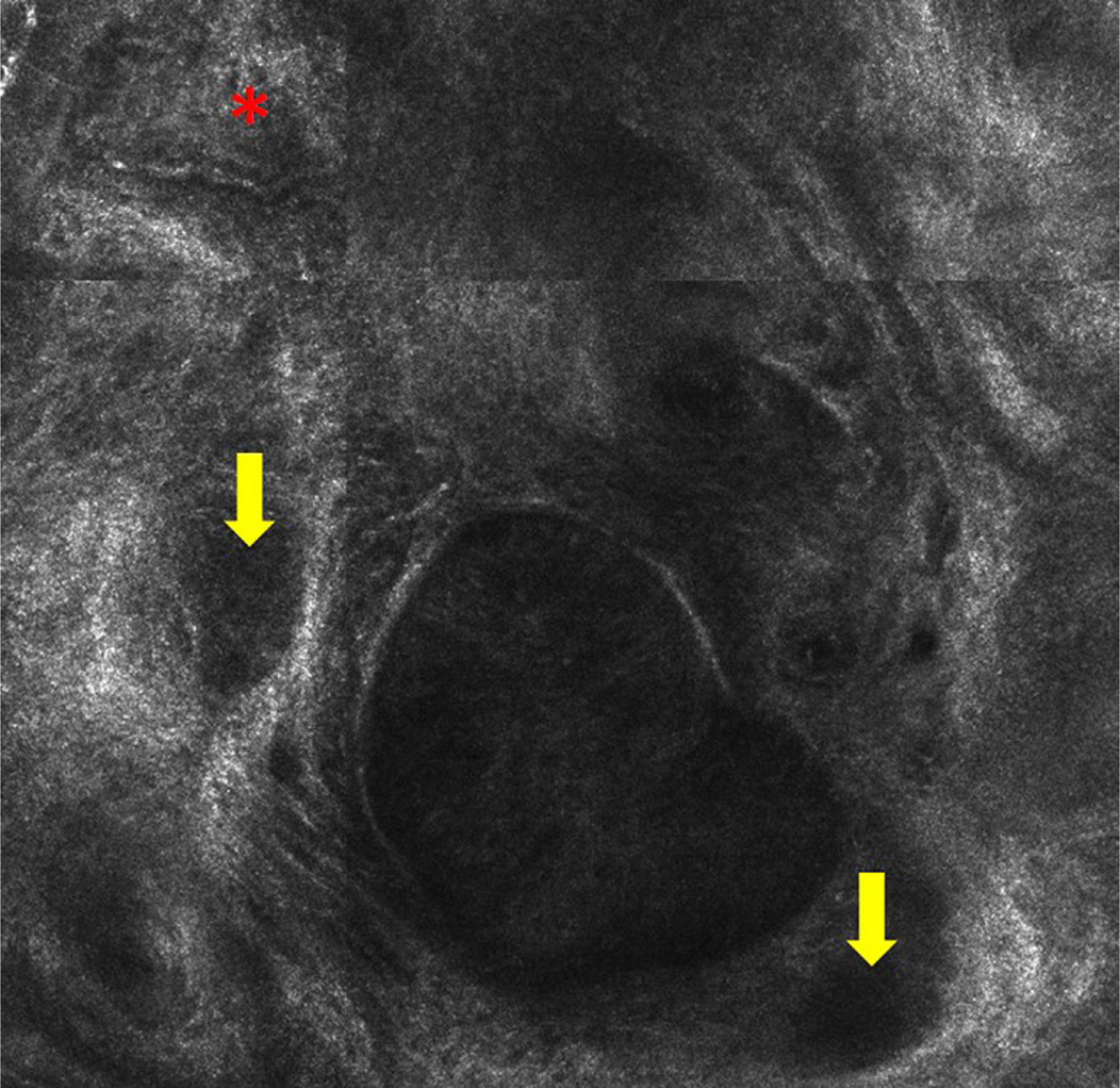
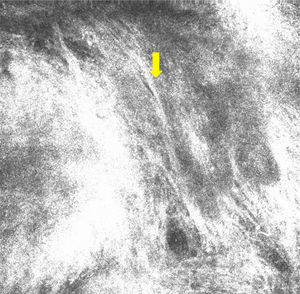
Case 2A 38-year old woman with no relevant past medical history presented with multiple melanocytic nevi. She reported no personal or family history of melanoma, or past episodes of sunburn or prolonged sun exposure. The physical examination revealed an erythematous papule in the left preauricular region that had been present for over 3 months. Dermoscopy showed well-defined vessels (Fig. 3), while RCM showed polarized nuclei in the epidermal tumor cells, tumor nests or islands with clefting between the nests and the stroma, and peripheral palisading in some of the nests. Tortuous vessels and several nonrefractive nests (dark silhouettes) were also visible (Figs. 4-6). The lesion was excised and the suspected diagnosis of BCC was confirmed by histology, which showed nests with a superficial multicentric pattern in the epidermis and a multinodular pattern in the dermis.
BCC and intradermal melanocytic nevus lesions on the face are very common. A correct diagnosis can be reached in most cases with a thorough history and physical examination. Dermoscopy can also help by revealing typical features of BCC and melanocytic nevus. BCCs present blue-gray ovoid nests, blue dots, ulceration, cartwheel structures, and maple leaf–like areas, in addition to arborizing telangiectatic vessels and short, short curved vessels. Typical dermoscopic features of intradermal melanocytic nevus lesions, in turn, are brown globules and comma vessels.
The dermoscopic distinction between the 2 conditions, however, is not always clear. For example, there are cases in which the typical nests seen in BCC (round structures) are brown rather than blue-gray and thus difficult to distinguish from the brown globules seen in melanocytic nevus. Furthermore, the characteristic short prominent vessels in BCC may be confused with the comma vessels seen in melanocytic nevus, and likewise, melanocytic nevus lesions may show the typical arborizing vessels seen in BCCs. In one study that analyzed 609 BCCs and 200 melanocytic nevi, 40% of the BCCs (largely pigmented lesions) showed typical dermoscopic characteristics of melanocytic lesions, namely brown-back globules and dots, a blue-white veil, and nonarborizing vessels.1
In the first case described in this report, the patient's age (39 years) and the duration of the lesion (10 years) were both suggestive of melanocytic nevus. However, the presence of brown or gray round structures and the gray blue color on dermoscopy made it necessary to rule out BCC and lichenoid keratosis, respectively.
In the second case, the diagnosis was complicated by the age of the patient, the presence of multiple nevi, and the absence of typical dermoscopic features of BCC other than prominent vessels.
RCM has demonstrated its value in differentiating between BCC and intradermal melanocytic nevus.2,3 When examined by RCM, intradermal melanocytic nevi tend to show a cobblestone pattern formed by multiple monomorphic shiny pigmented keratinocytes. Common findings in the dermis are nests of nevus cells (dermal nests), which appear as nests of tightly packed uniform cells, without atypia.4,5
RCM features of BCC include tumor nests or islands with peripheral palisading, formed by elongated tumor cell nuclei arranged perpendicularly to the tumor lobules.6–8 Other features include a dark cleft between the nests and the stroma and polarized tumor cell nuclei (all located on the same axis). These tumor nests are occasionally very dark and completely hyporeflective but are surrounded by a brighter stroma (dark shadows). The images show an increase in the number and diameter of capillaries attributable to tumor angiogenesis. Reflective dendritic cells may also be observed inside and outside the nests. The cells inside tend to be melanocytes while those outside are generally Langerhans cells.9
RCM provided key diagnostic clues in the 2 cases described in this report. The diagnosis of BCC was suggested by the presence of tumor nests separated from the stroma and occasional peripheral palisading in both patients, and by the presence of polarized nuclei in the epidermis and tortuous dilated vessels in the second patient.
RCM is a noninvasive technique that produces images with near-histologic resolution and permits in vivo distinction between intradermal melanocytic nevus lesions and BCC.
Ethical DisclosuresProtection of humans and animalsThe authors declare that no tests were carried out in humans or animals for the purpose of this study.
Confidentiality of dataThe authors declare that they have followed their hospital's protocol on the publication of data concerning patients.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects referred to in this article. This document is held by the corresponding author.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Gamo R, Floristan U, Pampín A, Caro D, Pinedo F, López-Estebaranz JL. Utilidad de la microscopia confocal en el diagnóstico diferencial de epiteliomas basocelulares y nevus melanocíticos intradérmicos de localización facial. Actas Dermosifiliogr. 2014;106:e41–e44.

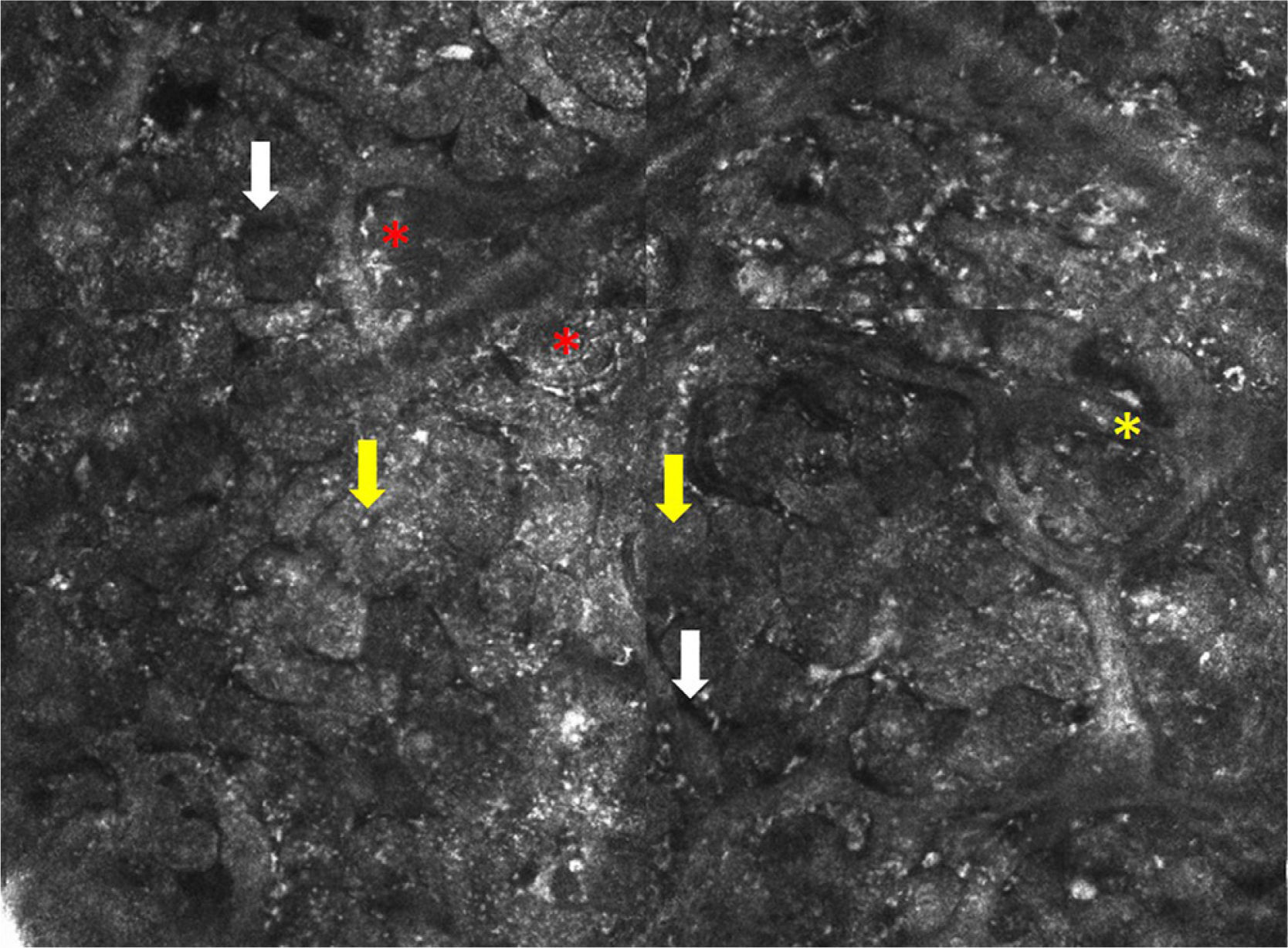


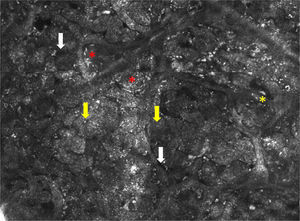

![Confocal microscopy image measuring 1×0.75mm. Note the nests of cells (yellow arrow and separation between the stroma and the nests [white arrow]). Peripheral palisading (red asterisk) can be observed in some of the nests. Confocal microscopy image measuring 1×0.75mm. Note the nests of cells (yellow arrow and separation between the stroma and the nests [white arrow]). Peripheral palisading (red asterisk) can be observed in some of the nests.](https://static.elsevier.es/multimedia/15782190/0000010600000008/v1_201510011018/S1578219015002073/v1_201510011018/en/main.assets/thumbnail/gr5.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)