To the Editor:
Photodynamic therapy (PDT) is a light therapy that involves the production of reactive oxygen species and free radicals to induce oxidation in biological tissues. The effect is achieved through the application of a photosensitizing agent, which is then activated by exposure to wavelength-specific light.1 The most commonly used photosensitizer is methyl aminolevulinate (MAL). PDT is primarily used in the treatment of basal cell carcinoma, actinic keratosis, and Bowen disease, although it can also be used to treat certain non-neoplastic diseases. The most common side effects are pain and local inflammation; wheals are very rare.2 We present the cases of 2 pediatric patients who developed urticarial reactions to PDT.
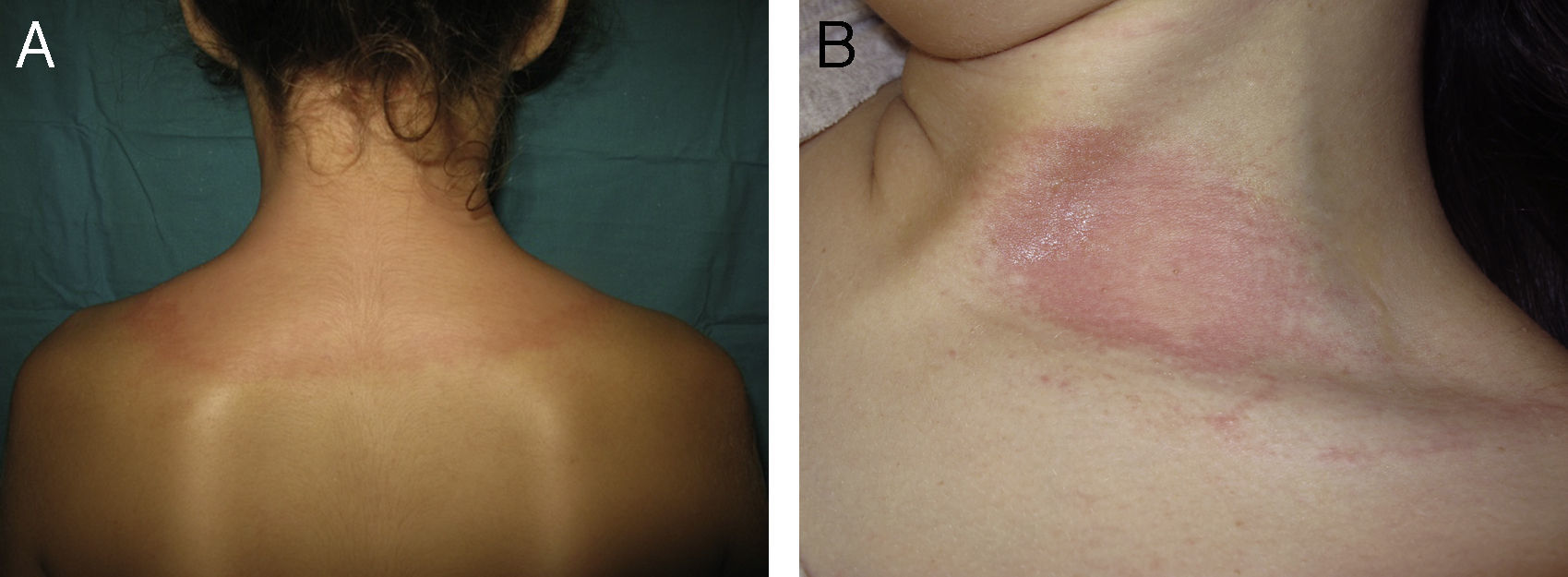
The first patient was an 11-year-old girl with nevoid basal cell carcinoma syndrome (Gorlin syndrome) who presented with the characteristic clinical manifestations, including frontal bossing, hypertelorism, small ears, syndactyly, palmar pits, and a large number of small, pedunculated, papular lesions on the neck, axillas, groin, and popliteal fossae. Histologic examination of these lesions revealed basal cell carcinoma. The lesions had previously been treated with cryotherapy, electrocoagulation, and imiquimod. PDT treatment was prescribed and administered on several lesions on the upper back and the neck according to the standard protocol: MAL 160mg/g cream (Metvix) applied under occlusion for 3hours followed by illumination using an Aktilite lamp at a dose of 37J/cm2. Three minutes after starting illumination, semicircular wheals appeared in the area being treated, and light exposure was stopped (Fig. 1A). The lesions disappeared after a few hours without treatment and did not recur. Some months later the patient underwent provocation testing with the MAL cream applied under occlusion for 3hours followed by illumination. Wheals appeared in the illuminated area where the cream had been applied, but no lesions were observed in the area exposed to light without prior application of cream (Fig. 1B). The wheals disappeared spontaneously and there was no recurrence.
The second patient was a 4-year-old girl with no relevant past history or family history who presented with brownish, erythematous, maculopapular lesions in a blaschkoid distribution affecting the dorsum and anterior aspect of the left forearm, thigh, and left leg. Porokeratosis was revealed on histology (Fig. 2A). The lesions had not responded to treatment with topical corticosteroids or retinoids. Treatment with PDT was administered using the standard protocol without pretreatment curettage. After 2minutes of light exposure, large erythematous, edematous lesions appeared in the area being treated and the procedure was stopped (Fig. 2B). The lesions disappeared after a few hours without treatment and did not recur. Provocation testing was not carried out due to the young age of the patient.
A, Observe the cornoid lamella—a column of stacked parakeratotic cells extending through the stratum corneum characteristic of porokeratosis. Hematoxylin-eosin, original magnification ×100. B, Large erythematous, edematous lesions on the left leg on the area where PDT treatment was applied.
In both patients, Giemsa staining of skin biopsies taken prior to PDT showed no significant increase in the number of mast cells.
Urticarial reactions to PDT using 5-aminolevulinic acid and MAL have been described in the literature.3–5 A 2008 study reported a 0.9% prevalence (12/1353 patients) for severe itching and wheals within the first minute of illumination.5 The patients most predisposed to reaction were those who had received more than 7 courses of treatment (3.8% prevalence).5 Those authors postulated that this type of urticaria may be mediated by immunoglobulin E with histamine release from mast cells in the dermis. This pathogenesis is consistent with the recurrent nature of the reactions in subsequent treatments, the satisfactory control of these reactions through the administration before treatment of an antihistamine such as cetirizine, and the immediate appearance of urticaria in areas not previously treated with PDT.5 In our patients, urticaria appeared during the first course of treatment. In the first patient, a subsequent provocation skin test confirmed that the reaction was produced by the combination of MAL and illumination, and not by either one separately.
Of particular note was the especially extensive reaction in our patients. We found no reports in the literature of nevoid basal cell carcinoma syndrome involving a similar reaction to PDT, despite the increasing use of PDT in these patients.6–8 Similarly, we found no reports of urticarial reactions in patients with porokeratosis treated with PDT.9,10 An additional associated factor could be the young age of these patients. We found no cases in the literature of reaction to PDT in children, but this treatment is rarely used in this age group. It has been suggested that mast cells may play a role in this type of reaction and at the same time participate in the nonspecific immune response that results in the tissue damage caused indirectly by PDT. We therefore postulated the possibility of high mast cell counts in the affected areas, but this hypothesis was ruled out by the results of Giemsa staining.
In summary, these 2 rare cases of urticaria during PDT in children, a previously unreported reaction in this age group, demonstrate the need for dermatologists to be aware of this reaction so that they will stop illumination promptly and treat the resulting lesions appropriately.
Please cite this article as: Miguélez A, et al. Reacción urticariforme secundaria a terapia fotodinámica en 2 pacientes pediátricos. Actas Dermosifiliogr. 2013;104:727–9.