The systemic vasculitides make up a heterogeneous group of disorders that affect various organs and systems through blood vessel inflammation and damage. Some of these disorders have high mortality rates, which can only be reduced by early diagnosis and prompt treatment. However, the absence of a definitive diagnostic test for vasculitis and the rarity and clinical heterogeneity of these disorders inevitably lead to delayed diagnosis in most cases. The situation could be improved by the development and validation of well-defined classification and diagnosis criteria, which currently do not exist for the systemic vasculitides. In the absence of such criteria, the classification of vasculitis proposed by the American College of Rheumatology in 19901 and the nomenclature and definitions proposed by the 1994 Chapel Hill Consensus Conference have often been used as a substitute.2
The classification for vasculitis proposed by the American College of Rheumatology (ACR) was designed primarily to identify homogeneous groups of patients for inclusion in clinical and epidemiological studies, but the criteria are less useful when used for diagnostic purposes. Over the years, the ACR criteria have proven unreliable in the diagnosis of vasculitides, an outcome that is not surprising since they were never designed to be used for that purpose.3 For example, they do not include microscopic polyangiitis as one of the vasculitic processes. Nor do they include the presence of antineutrophil cytoplasmic antibodies (ANCA) as a tool for the diagnosis of Wegener's granulomatosis, microscopic polyangiitis, or Churg-Strauss syndrome, (or the lack of ANCA in the case of polyarteritis nodosa [PAN]).
The goal of the first Chapel Hill Consensus Conference,1 held in 1994, was to define the nomenclature of the most common forms of vasculitis, including microscopic polyangiitis. The definitions proposed for each of the vasculitides included a list of the characteristics that had to be present in any patient to justify the use of the term for the diagnosis or classification of the condition; however, they did not specify what observations or criteria should be used to make a definitive decision on the type of vasculitis present in a specific patient. The reason for this lies in the importance of distinguishing between definitions, diagnostic criteria, and classification criteria. For example, it is easy to understand that, while a definition may include very precise histopathologic descriptions, in practice the diagnosis of the disease does not require that these processes be demonstrated histologically in a tissue specimen from a biopsy. For instance, in an appropriate clinical context, the observation of a cavitary lesion in the lung documented by imaging studies may constitute sufficient evidence to conclude that a patient has a necrotizing granulomatous pulmonary inflammation even without histologic confirmation. Likewise, clear clinical manifestations of mononeuritis multiplex may constitute sufficient diagnostic or classification criterion for vasculitis affecting the peripheral nervous system even in the absence of a nerve biopsy and histologic confirmation of the vasculitis. Logically, later attempts to validate the Chapel Hill definitions as diagnostic criteria were unsuccessful.4,5 To remedy this deficiency, a joint project is underway involving the European League Against Rheumatism and the American College of Rheumatology. The goal of this project is to establish new criteria for the classification and diagnosis of vasculitides.6 As part of this project, pediatricians, convened through various organizations and societies, have already proposed and reached consensus on a set of diagnostic criteria for the childhood vasculitides.7
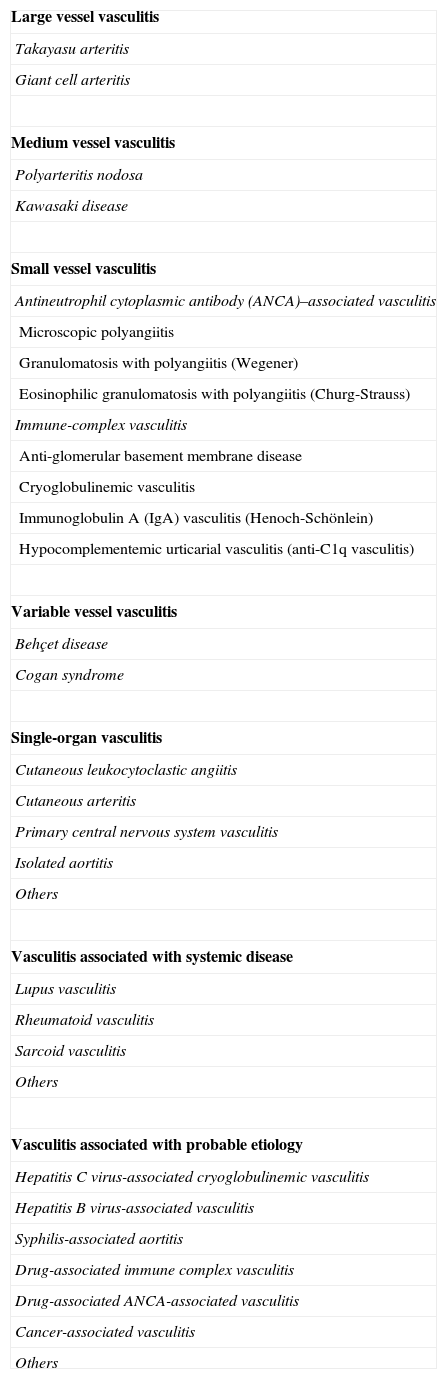
Advances in our understanding of vasculitides made another international consensus conference necessary (Chapel Hill, 2012).8 The goal of the second conference was to improve the existing nomenclature by modifying names and definitions where necessary and adding important categories of vasculitis that had been omitted from the 1994 consensus. Table 1 shows the revised definitions adopted at the 2012 International Chapel Hill Consensus Conference on the Nomenclature of Vasculitis. In this article we will discuss some of the most important changes and highlight those of particular interest to dermatologists.
Names for Vasculitides Adopted by the 2012 International Chapel Hill Consensus Conference on the Nomenclature of Vasculitides.
| Large vessel vasculitis |
| Takayasu arteritis |
| Giant cell arteritis |
| Medium vessel vasculitis |
| Polyarteritis nodosa |
| Kawasaki disease |
| Small vessel vasculitis |
| Antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis |
| Microscopic polyangiitis |
| Granulomatosis with polyangiitis (Wegener) |
| Eosinophilic granulomatosis with polyangiitis (Churg-Strauss) |
| Immune-complex vasculitis |
| Anti-glomerular basement membrane disease |
| Cryoglobulinemic vasculitis |
| Immunoglobulin A (IgA) vasculitis (Henoch-Schönlein) |
| Hypocomplementemic urticarial vasculitis (anti-C1q vasculitis) |
| Variable vessel vasculitis |
| Behçet disease |
| Cogan syndrome |
| Single-organ vasculitis |
| Cutaneous leukocytoclastic angiitis |
| Cutaneous arteritis |
| Primary central nervous system vasculitis |
| Isolated aortitis |
| Others |
| Vasculitis associated with systemic disease |
| Lupus vasculitis |
| Rheumatoid vasculitis |
| Sarcoid vasculitis |
| Others |
| Vasculitis associated with probable etiology |
| Hepatitis C virus-associated cryoglobulinemic vasculitis |
| Hepatitis B virus-associated vasculitis |
| Syphilis-associated aortitis |
| Drug-associated immune complex vasculitis |
| Drug-associated ANCA-associated vasculitis |
| Cancer-associated vasculitis |
| Others |
Source: Jennette et al.8
In line with the trend evident in other specialties, the use of eponyms in the nomenclature of vasculitis was considered to be outdated. Eponymous names were, therefore, generally replaced by a descriptive term relating to the pathophysiologic mechanism of the type of vasculitis. However, the original eponym was retained if the mechanism was not yet sufficiently understood to form the basis of an alternative name. For instance, the participants agreed to retain, for the moment, the eponymous term Takayasu arteritis but to replace the following eponyms with more descriptive names: Wegener's syndrome (changed to granulomatosis with polyangiitis), Churg-Strauss syndrome (eosinophilic granulomatosis with polyangiitis), and Henoch-Schönlein purpura (immunoglobulin A [IgA] vasculitis).
The ideal approach for the categorization or subdivision of the vasculitides would be one based on etiology. However, this approach is not feasible at the moment because the etiology of most vasculitides is still poorly understood. Consequently, the group of experts who participated in the 2012 consensus conference categorized the vasculitides on the basis of the entire body of knowledge available at the time relating to the etiology, pathogenesis, microscopic features, demographic aspects, and clinical manifestations of each one. In the revised nomenclature, the first level of categorization is still based on the type of vessel predominantly affected in each case, a system that gives rise to 3 major categories: large vessel vasculitis, medium vessel vasculitis, and small vessel vasculitis. These terms refer not only to the size of the vessel but also to structural and functional attributes that determine a particular susceptibility to the different pathogenic mechanisms and specific variants of vasculitides. It is, however, essential to remember that vasculitides falling into any of the 3 major categories can affect vessels of any size. It is important to be aware, for example, that small arteries may also be affected in cases of large or medium vessel vasculitis.
A second level of categorization is based on the epidemiological, clinical, and laboratory variables that define a series of subgroups. For example, age of onset continues to be a key clinical criterion differentiating Takayasu arteritis and giant cell arteritis (the term temporal arteritis is no longer used) when the histopathologic features are indistinguishable. Some authors have suggested that these two disorders may be the same disease but, in the absence of clear evidence of a common etiology, the consensus was that Takayasu arteritis is a disease that predominantly affects young people while giant cell arteritis affects older adults.9 The introduction of ANCA as an additional criterion for the subcategorization of certain small and medium vessel vasculitides is another new element in the revised nomenclature, reflecting advances in our knowledge of these antibodies with respect to what was known at the time of the 1994 Chapel Hill Consensus Conference.10,11 ANCA are clearly not associated with PAN, a fact reflected in the definition of that condition. By contrast, the presence of ANCA is definitively linked to the ANCA-associated vasculitides, a category that includes microscopic polyangiitis, granulomatosis with polyangiitis (Wegener), eosinophilic granulomatosis with polyangiitis (Churg-Strauss), and ANCA-associated single-organ vasculitis. A prefix indicating the specific reactivity of the associated ANCA should be added to the name of each of these vasculitides; for example, MPO-ANCA (ANCA specific to myeloperoxidase) or PR3-ANCA (ANCA specific to proteinase 3). If no specific reactivity has been identified, the prefix ANCA-negative should be added (a situation similar to that of seronegative rheumatoid arthritis or lupus). Although the role of ANCA in the pathogenesis of these vasculitides has not been fully elucidated, many studies have confirmed that these antibodies are a key marker for the categorization of small and medium vessel vasculitides, which can have indistinguishable clinical and histologic features.
The category of vasculitides affecting the medium vessels (defined in this setting as the main visceral arteries and their branches) now includes Kawasaki disease in addition to PAN. Kawasaki disease is defined as an arteritis associated with the mucocutaneous lymph node syndrome that predominantly affects the small and medium arteries, in particular the coronary arteries although the aorta and large arteries may also be involved. In this case, as with Takayasu arteritis, the consensus was in favor of retaining the eponymous name Kawasaki disease because the eponym was considered to be more effective than the alternative term proposed—mucocutaneous lymph node syndrome arteritis.
The group of small vessel vasculitides includes, in addition to the ANCA-associated disorders, the immune complex small vessel vasculitides, which are subdivided according to the predominant component in the formation of the immune complex. This group includes anti-glomerular basement membrane disease (formerly Goodpasture's syndrome), cryoglobulinemic vasculitis, IgA vasculitis (Henoch-Schönlein), and hypocomplementemic urticarial vasculitis (anti-C1q vasculitis). When it is possible to identify the disease associated with the vasculitis or the cause of the disorder, the preferred approach is to categorize the disorder under the headings created in the revised nomenclature to cover that situation, that is, vasculitis associated with systemic disease and vasculitis associated with probable etiology. In this way, specific terms are proposed, including lupus vasculitis, rheumatoid vasculitis, and hepatitis C virus-associated cryoglobulinemic vasculitis (Table 1).
Another new aspect of the 2012 Chapel Hill revised nomenclature is the identification of two additional categories of vasculitis: variable vessel vasculitis and single organ vasculitis. Variable vessel vasculitis refers to the vasculitides not characterized by a predominance of any specific vessel size, which can affect small, medium, or large vessels. This new category includes Behcet disease and Cogan syndrome. In both these disorders, involvement of the capillaries, arterioles, and small arteries of the skin in the vasculitic process causes skin lesions, which in the case of Cogan syndrome have been described as urticarial and in the case of Behcet disease can be highly polymorphic (papules, pustules, nodules, etc.) depending on the size of the affected vessel.
Of particular interest to dermatologists is the recognition of a category referring to single-organ vasculitis. This term encompasses the vasculitides that affect arteries or veins of any size within a single organ in the absence of any evidence indicating that the condition is the expression of a systemic vasculitis limited to a single-organ. If such evidence is observed, it is preferable to classify the condition as systemic rather than single-organ vasculitis. In single-organ vasculitis, the organ and vessel type involved should be included in the name, giving rise to terms such as cutaneous small vessel vasculitis and cutaneous arteritis in the case of variants that affect the skin exclusively. The term cutaneous leukocytoclastic vasculitis still appears in the classification as a synonym for small vessel cutaneous vasculitis. The term cutaneous hypersensitivity vasculitis, used widely for years by dermatologists and dermatopathologists, was eliminated in the 1994 Chapel Hill Consensus Conference on the Nomenclature of Vasculitis. At that time, 2 new categories were created to encompass these disorders: microscopic polyangiitis and cutaneous leukocytoclastic vasculitis. The justification for eliminating the classic denomination was the clear evidence that the pathogenic mechanism involved in these vasculitides was not hypersensitivity.12 In the revised nomenclature, the term cutaneous polyarteritis nodosa, which dermatologists are accustomed to using, has been replaced by the term cutaneous arteritis. This condition, which is characterized by the presence of painful nodules, livedo reticularis, and—in some cases—ulceration on the lower limbs, has classically been considered to be a localized and not very severe form of PAN associated with low mortality and lesions that are highly resistant to conventional treatments.13 However, there is probably still insufficient etiologic and pathogenic evidence available to make a definitive decision on whether cutaneous arteritis should be considered a form of vasculitis affecting only the skin with no connection with systemic PAN, or whether it is a single-organ variant of PAN. In any case, it is always important to bear in mind that patients who are originally diagnosed with single-organ vasculitis may later develop additional disease manifestations that warrant reclassifying the condition as one of the systemic vasculitides.
As dermatologists, we should also remember that skin involvement is a component of most of the systemic vasculitides, particularly those affecting small and medium vessels. Thus, when a patient presents skin lesions in which necrotizing or leukocytoclastic vasculitis is confirmed histologically, irrespective of the size of the affected vessel, the possibility that the condition is a component of a systemic vasculitis must be ruled out. It is also essential to ascertain whether it is caused by an infection or a drug or is associated with a systemic disease (such as lupus erythematosus) before reaching the definitive diagnosis of a primary single-organ vasculitis affecting only the skin, such as cutaneous small vessel vasculitis or cutaneous arteritis.
In conclusion, changes in terminology and definitions are necessary to incorporate advances in medical knowledge and our understanding of diseases. The 2012 International Chapel Hill Consensus Conference identified new categories of vasculitis and modified certain terms and definitions to contribute to a more precise and valuable nomenclature that can really be useful in clinical practice.
Please cite this article as: Bielsa I. Actualización en la nomenclatura de las vasculitis. Conferencia de Consenso Internacional de Chapel Hill, 2012. Actas Dermosifiliogr. 2015;106:605–608.