We report the case of a 62-year-old man who presented with a 1-month history of a painful, ulcerated lesion on the glans of his penis. The lesion had started as a papular lesion that then ulcerated spontaneously and oozed a whitish matter. It had remained stable since. The patient reported that he had no other symptoms or similar lesions and confirmed that he had not engaged in risky sexual behavior. His past history was remarkable for a moderately differentiated invasive rectal adenocarcinoma that had been detected 16 months earlier (T3, N2b, M1a). The tumor had been treated with surgery, chemotherapy, and radiotherapy, and the patient had been in complete remission for the last 6 months.
Physical ExaminationPhysical examination revealed a 4-mm ulcer on the lateral aspect of the glans. The ulcer had a pink-erythematous background and traces of fibrin at its edges (Fig. 1). It was located on a well-delimited, indurated 1.5-cm plaque that had a stone-like consistency and was painful to the touch. No other cutaneous or mucosal lesions were observed and the inguinal lymph nodes were not enlarged on palpation.
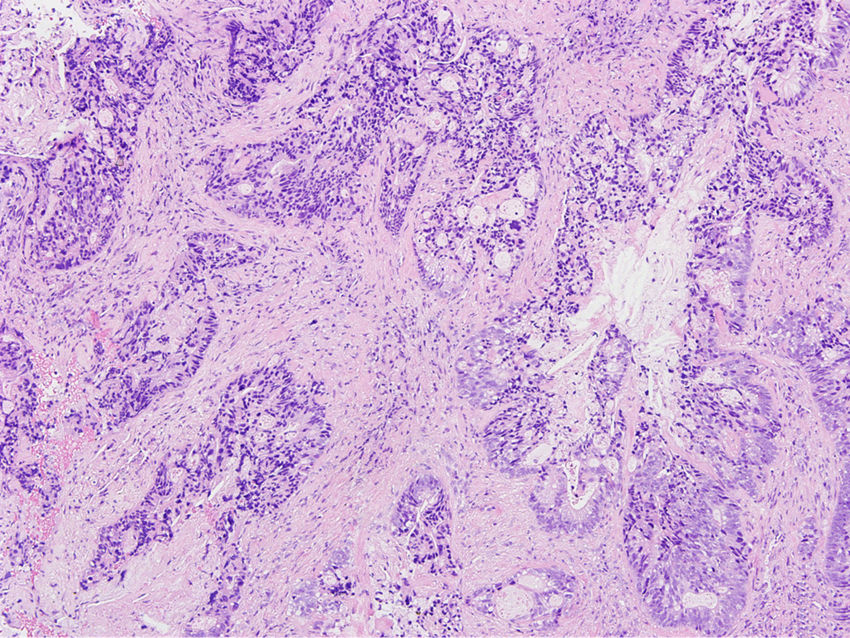
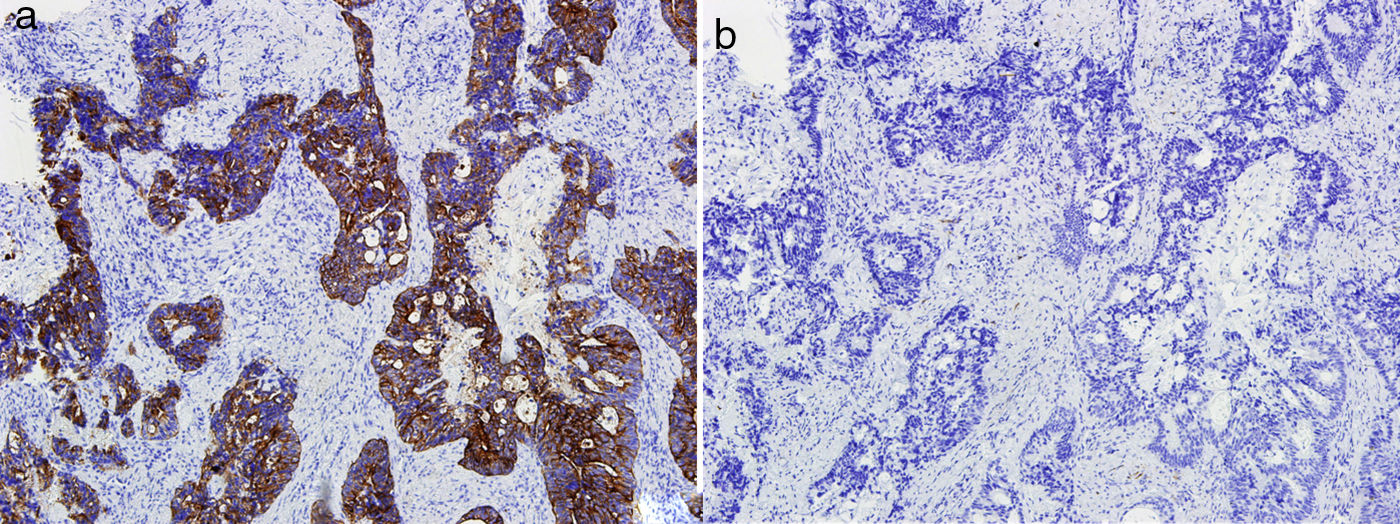
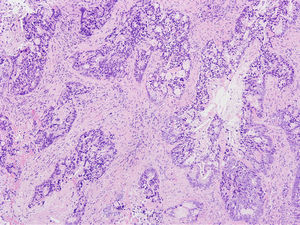
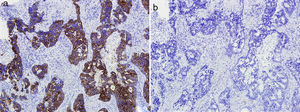
HistopathologyHistologic examination showed an infiltrate consisting of glandular formations (Fig. 2) that stained positively with cytokeratin 20 (Fig. 3) and negatively with cytokeratin 7 (Fig. 3B) in the immunohistochemical evaluation.
Additional TestsA basic blood workup including tumor markers and serology was normal, and the patient also tested negative for human papillomavirus. A computed tomography (CT) scan of the chest, abdomen, and pelvis ruled out locoregional and distant disease.
DiagnosisCutaneous penile metastasis from rectal adenocarcinoma.
Clinical Course and TreatmentA positron emission tomography–CT scan performed following diagnosis detected focal metabolic activity involving the glans, sacral alae, and iliac chains, indicating tumor invasion. The patient was started on palliative chemotherapy.
CommentThe first case of penile metastasis from rectal adenocarcinoma was reported in 19501 and just 25 cases have been published since. Metastases of this type are rare, even though the penis is highly vascularized and located very close to the rectum. The mechanism of spread to this rare location is still unknown.2 The theory with the greatest support is hematogenous spread resulting from retrograde embolization of the deep pudendal venous system; other theories include lymphatic spread through the hypogastric nodal group, spread through the perineural space, direct spread, and even inadvertent spread during surgery. Metastatic tumors of the penis usually appear within 18 months of primary diagnosis, although one-third occur synchronously.3 Cutaneous metastases to the penis have a highly variable clinical presentation,3 the most common of which is an indurated plaque or nodule that may or may not be ulcerated. The lesions are generally asymptomatic, although there may be perianal pain, priapism, hematuria, and urinary obstruction. They are typically located on the body of the penis and are rarely found on the glans or prepuce.
Both primary and secondary tumors of the penis should be included in the differential diagnosis. Primary tumors that should be contemplated include squamous cell carcinoma, adenosquamous carcinoma,4 and other penile adenocarcinomas, such as Littré gland carcinoma, melanoma, and sarcoma. Secondary tumors account for just 0.8% of all tumors of the penis, but of note in this category are genitourinary tumors (tumors of the bladder and prostate adenocarcinoma), which account for approximately 70% of primary tumors that metastasize to the penis.3,5
Cutaneous metastases have a dismal prognosis,5 and those involving the penis are associated with an overall survival of less than 1 year after diagnosis,3 as their presence tends to reflect disease spread. There is no established treatment. Management tends to be palliative, with chemotherapy and/or radiotherapy. Surgery is reserved for solitary metastases.
We have reported a rare case of cutaneous metastasis from rectal adenocarcinoma. The case is of particular interest because of its atypical location and its occurrence in a patient who appeared to be in complete remission at the time of diagnosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We thank the Hospital of Toledo and the Oncology Department at this hospital for their help.
Please cite this article as: Lorenzo ERM, Torres BM, Moya AIS. Lesión ulcerada en pene. Actas Dermosifiliogr. 2018;109:643–644.