An 83-year-old man with no relevant past history visited our emergency service for evaluation of asymptomatic nodular lesions on the right leg. The patient reported that the lesions had appeared 5 months earlier and had grown gradually, but that multiple similar lesions had suddenly started to appear close to the original lesions approximately 4 weeks earlier. The patient did not present constitutional symptoms or any other systemic symptoms.
Physical ExaminationThe patient presented skin lesions in the form of nodules and indurated plaques grouped on the posterior aspect of the right leg; the lesions measured between 8 and 13mm in diameter, were reddish-pink and infiltrated on palpation (Fig. 1). An enlarged lymph node could be felt in the right groin on palpation; the node was hard and attached to the deeper layers.
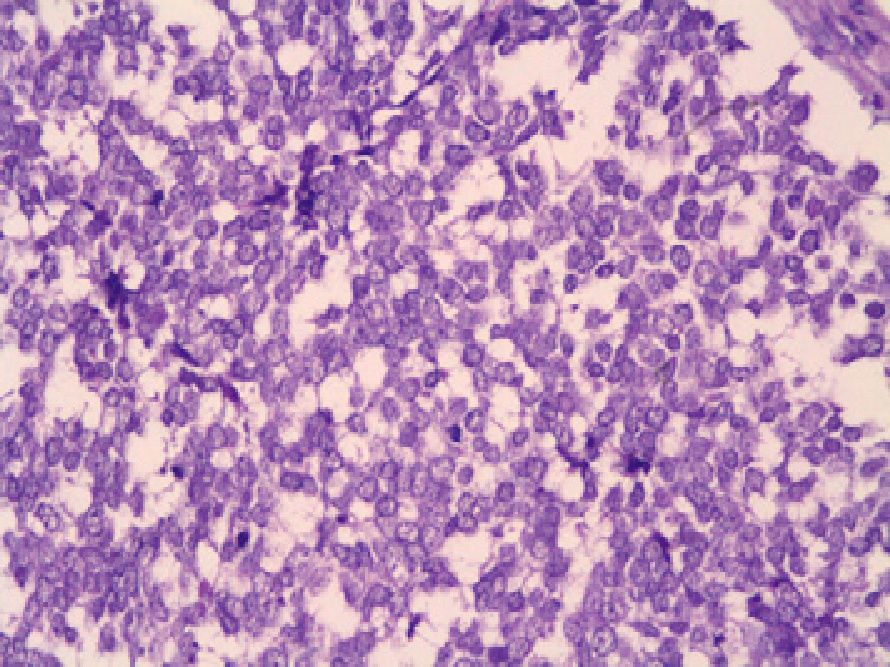
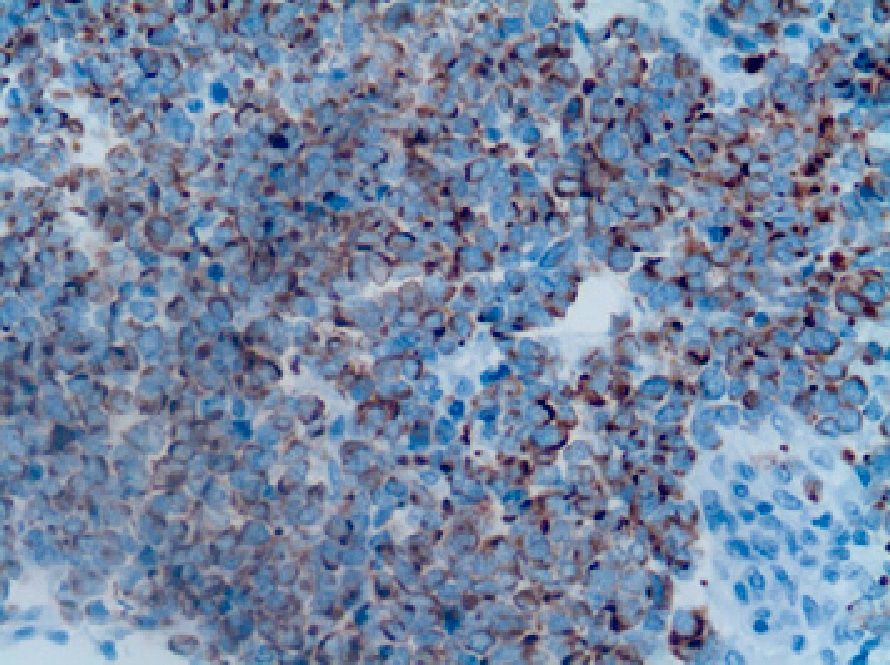
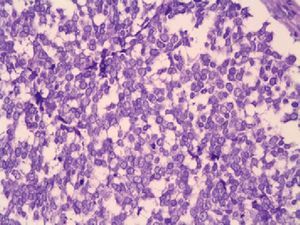
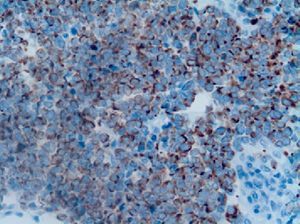
HistopathologyThe histopathology study revealed an infiltrate composed of atypical small blue cells in the dermis and subcutaneous cellular tissue. These cells presented a round vesicular nucleus with fine chromatin granules, multiple nucleoli, and abundant mitotic figures (Fig. 2). The epidermis was not involved. Immunohistochemistry was positive for neuron specific enolase (NSE) and cytokeratin (CK) 20 (Fig. 3). Staining with protein S-100, leukocyte common antigen, and CK7 was negative.
Additional TestsA full workup with tumor makers was normal, except for elevated levels of β2-microglobulin. A computed tomography scan of the chest, abdomen, and pelvis showed an enlarged lymph node in the right groin; the node measured 3.5 x 2cm and displayed tumorous characteristics.
What Is Your Diagnosis?
DiagnosisMetastatic Merkel cell carcinoma.
Clinical Course and TreatmentFine-needle aspiration biopsy of the lymph node was compatible with metastasis of neuroendocrine carcinoma. After studying the case in the skin cancer committee, it was decided to perform palliative treatment with radiation therapy.
CommentMerkel cell carcinoma is a rare but highly aggressive malignant skin cancer that originates in the Merkel cells located in the basal layer of the dermis.
It is more frequent in patients aged65 years or older and most commonly appears on exposed areas of the head and neck.1,2 However, pathogenesis of this tumor has recently been linked to the polyomavirus (approximately 80% of Merkel cell carcinoma tissue samples present the polyomavirus genome compared to between 8% and 16% of control tissue samples).3
Clinically, it develops rapidly, in weeks or months, as an asymptomatic, indurated, erythematous-violaceous nodule with a smooth, shiny surface.4 As well as these common hemispherical or nodular forms, the tumor may manifest as an indurated plaque, although this form of presentation is less common.5 Ulceration is rare and usually appears in advanced tumors.4 Nevertheless, satellite metastases, as occurred in our patient, are not uncommon.4
The disease predominantly affects the head and neck (>50% of cases); the limbs are involved in 40% of cases and the torso in less than 10% of cases.6
Because of the nonspecific nature of the clinical characteristics, diagnosis is determined by means of histopathology in most cases.2,4 Histopathology shows a dermal tumor that often extends to the subcutaneous cellular tissue. The papillary dermis, the epidermis, and the adnexa are usually not involved. The study shows a dense infiltrate of small basaloid monomorphous cells with a hyperchromatic nucleus and scant cytoplasm.6Because of its cytologic characteristics, the tumor should be differentiated from metastases of visceral neuroendocrine carcinomas (particularly small cell lung cancer) and from some types of lymphoma and melanoma.5 Immunohistochemistry makes is possible to distinguish Merkel cell carcinoma from these tumors. Merkel cell carcinoma expresses neuroendocrine markers (NSE, chromogranin, synaptophysin) and cytokeratin markers with a low molecular weight (CK20, CAM 5.2, CK AE1), and is negative for protein S-100 and leukocyte common antigen.2,4,5 Furthermore, thyroid transcription factor-1, which is positive in small cell lung cancer, is negative in Merkel cell carcinoma.4–6
Prognosis is poor owing to the high rate of recurrence (12%-50%), regional lymph node metastasis (17%-76%), and distant metastasis (12%-50%).2,5
The most important prognostic factor for survival and development of systemic disease is lymph node involvement.6
Traditional surgery with margins of between 2 and 3cm is the treatment of choice for patients with no metastatic disease.2,4–6 Lymph node metastasis should be treated with radical lymph node resection. Postoperative radiation therapy of the tumor and lymph node region is recommended in these cases.4 Radiation therapy is used in patients with systemic disease and may be accompanied by surgery and/or chemotherapy.2,4,5
Please cite this article as: Mota-Burgos A, et al. Lesiones tumorales agrupadas en la extremidad inferior. Actas Dermosifi-liogr. 2013; 104:159-60.