Nail disorders in newborns can show independently or as components of systemic illnesses or genodermatoses. The examination of these abnormalities is complex and sometimes challenging. However, familiarity with these disorders can significantly contribute to uncovering potential underlying conditions.
This review includes the physiological nail changes seen within the first few months of life, such as Beau's lines, onychoschizia, koilonychia, congenital nail fold hypertrophy of the first digit, and onychocryptosis. This review also focuses on the most relevant congenital disorders reported and how to perform differential diagnosis. Finally, this review highlights those hereditary diseases in which nail involvement is crucial for diagnosis, such as nail-patella syndrome, congenital pachyonychia, or congenital dyskeratosis, among others.
Las alteraciones ungueales en los recién nacidos pueden presentarse de forma aislada o formar parte de una enfermedad sistémica o una genodermatosis. Su estudio resulta complejo y en ocasiones supone un reto, sin embargo, el conocimiento de estas alteraciones puede resultar de gran utilidad a la hora de descubrir posibles dolencias ocultas.
Esta revisión incluye los cambios fisiológicos ungueales que aparecen en los primeros meses de vida: líneas de Beau, onicosquisis, coiloniquia, hipertrofia congénita de los pliegues ungueales del primer dedo y onicocriptosis. También se ocupa de las anomalías congénitas más relevantes y cómo realizar su diagnóstico diferencial. Por último, se destacan aquellas enfermedades hereditarias en las que la afectación ungueal es clave para hacer el diagnóstico, como el síndrome de uña-rótula, la paquioniquia congénita o la disqueratosis congénita, entre otras.
The nail apparatus consists of a series of structures that collectively have important functions, 3 of which are providing protection for distal phalanges, nerve fibers, and soft tissues; being an organ of touch and grip; and having an aesthetic and cosmetic function.1
In the anatomical approach to the nail, from its proximal to distal part, we find the proximal nail fold, which continues distally with the cuticle, which is firmly attached to the nail plate and protects the nail apparatus. Right underneath the proximal fold is the nail matrix, which is the germinative epithelium that gives rise to most of the nail plate. The matrix consists of a proximal part, which forms the dorsal portion of the plate, and a distal part, which produces the ventral portion of the nail. The distal matrix—also called the lunula—is the only visible part of the matrix, and is a whitish, opaque, crescent-shaped area located at the proximal end of the nail.1 The nail bed contributes to adhesion and whether it forms the ventral portion of the nail plate is still to be elucidated. The nail bed consists of a thin epithelium with numerous glomic bodies and connective tissue it supports; this bed continues with the hyponychium, where the nail plate ceases to be intimately adhered to the nail bed, thus acquiring a more whitish color.1 The nail plate is bounded by the proximal, distal, and lateral folds.
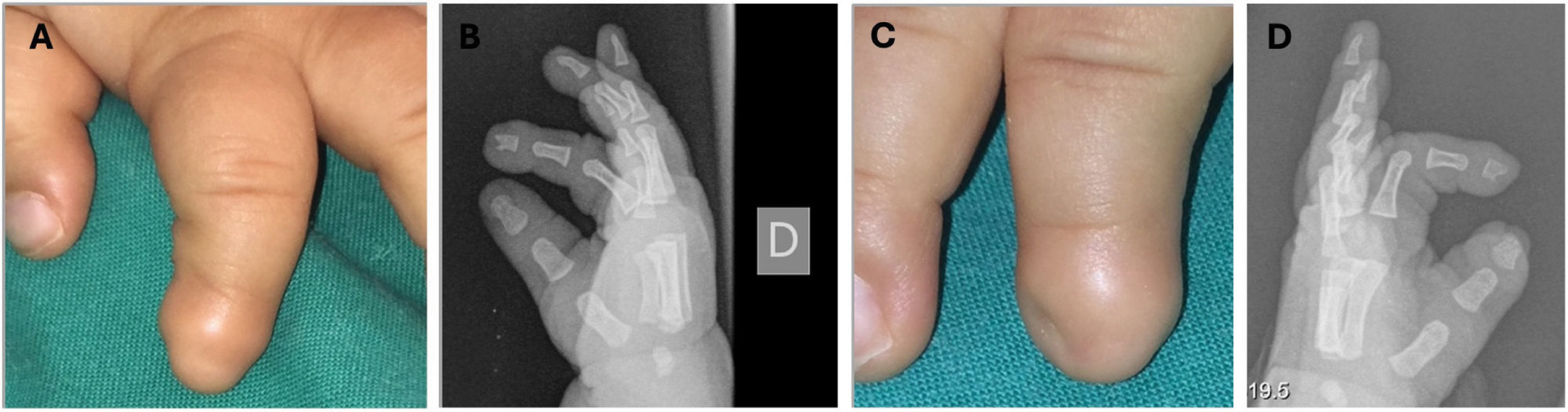
Nails are in a constant state of activity; within the first few months of life, they have a growth rate similar to that of young adults, but growth rate accelerates between 10 and 15 years of age. At birth, newborns’ nails are thin and soft, have a triangular morphology, and subsequently, with the child's development and growth, they become thicker and harder2 (Fig. 1A).
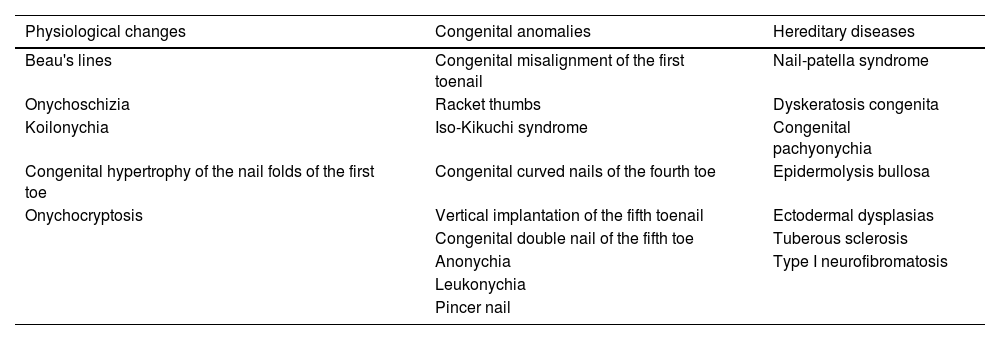
We must distinguish between physiological changes in the nails and pathological variants, which can be categorized into congenital anomalies and hereditary nail diseases (Table 1). The correct approach to nail disease can be key to diagnosing systemic diseases that would otherwise go unnoticed.
Nail changes that can occur early in life.
| Physiological changes | Congenital anomalies | Hereditary diseases |
|---|---|---|
| Beau's lines | Congenital misalignment of the first toenail | Nail-patella syndrome |
| Onychoschizia | Racket thumbs | Dyskeratosis congenita |
| Koilonychia | Iso-Kikuchi syndrome | Congenital pachyonychia |
| Congenital hypertrophy of the nail folds of the first toe | Congenital curved nails of the fourth toe | Epidermolysis bullosa |
| Onychocryptosis | Vertical implantation of the fifth toenail | Ectodermal dysplasias |
| Congenital double nail of the fifth toe | Tuberous sclerosis | |
| Anonychia | Type I neurofibromatosis | |
| Leukonychia | ||
| Pincer nail |
Beau's lines result from a temporary cessation of nail growth at the proximal matrix.3–5 They appear in 92% of newborns at 4 weeks of life and tend to disappear at around 14 weeks. Clinically, they appear as single or multiple transverse grooves or moat-like depressions in the nail plate. Their thickness and depth of provide information on the duration and intensity of the causative process.2
They are believed to be due to the loss of fetal well-being or physiological changes during childbirth, reflecting the neonate's adaptability to the environment.4 When this alteration appears only in 1 nail, it is often of traumatic origin. However, when it occurs in several nails, a systemic etiology such as prolonged fever or infectious conditions, especially hand-foot-and-mouth disease, needs to be ruled out, as Beau's lines appear in up to 24% of cases.3,6
OnychoschiziaOnychoschizia is a transverse lamellar peeling at the distal free edge of the nail plate, mainly affecting the first fingers of the hands and feet. It appears in a third of newborns; onychoschizia may be favored by the fact that nails at this stage of life are very thin, repeated baths, or humidity.4,6 When it occurs on the first finger of the hand, it is usually associated with sucking of such finger.7
KoilonychiaKoilonychia or spoon nail is a variant of normality in 33% of newborns and improves spontaneously with age. It mainly affects the first toe.7 It can be a clinical sign of trauma or diseases such as systemic lupus erythematosus, nail-patella syndrome, psoriasis, lichen planus, or iron deficiency anemia, among others.4,6,8,9 A systemic cause should be suspected when koilonychia affects both fingers and toes.7
Clinically, we can see loss of the normal curvature of the nail plate. The central part is depressed, and the lateral edges are everted, resulting in a concave transverse axis of the nail3,5,8 (Fig. 1B).
Congenital hypertrophy of the nail folds of the first toeThis condition appears at birth or within the first few days of life and usually resolves spontaneously within the first year. It is due to the asynchrony between the growth of the nail plate and periungual tissues.3,4,6,8 It is characterized by hypertrophy of the periungual soft tissues—preferably the lateral folds although the distal folds are involved too—of the first toe.3,4,6,8 It can occasionally partially or completely cover the nail plate (Fig. 1C). Possible complications include paronychia, misalignment of the nail plate, koilonychia, or onychocryptosis.4,6 No therapy is necessary, only massaging the hypertrophied fold. Occasionally, treatment with topical corticosteroids or antibiotics is prescribed to control associated secondary inflammation or infection, sparing surgical management for cases that do not resolve within the first year of life.3,4,8
OnychocryptosisOnychocryptosis is the painful inflammation of the distal periungual skin due to nail embedding. This condition may appear around the 6th day of life in the fingernails due to the newborn's grasp reflex and tends to resolve spontaneously around the 4th month of life.6 It can also affect the toenails, which in the newborn are short, thin, and poorly aligned in relation to the correctly directed toe. During infancy, the distal phalanx has not yet ossified, so the pressure to the nail plate can embed it in the underlying soft tissue.4 This triggers an inflammatory reaction that can result in granulation tissue with exudate, bleeding, and infection, along with pain and hypertrophy of the nail fold.4,6,8 In situations in which there is congenital misalignment of the nail of the first toe, onychocryptosis may persist and require surgical treatment for correction.4,5
Congenital nail anomaliesCongenital misalignment of the first toeThis is a disease of unknown etiopathogenesis; some describe it as caused by an anomaly of the ligament connecting the nail matrix to the periosteum of the distal phalanx, while others relate it to excessive traction of the extensor tendon of the hallux, although genetic or embryological factors may also condition this entity.10,11
In this condition, the nail matrix is oriented laterally in relation to the longitudinal axis of the distal phalanx, submitting the nail being to constant trauma. Repetitive mechanical changes cause the appearance of Beau's lines, thickening, and discoloration of the nail plate, and morphological changes, becoming more triangular or trapezoidal (Fig. 2). Over time, the nail acquires an “oyster shell” appearance.3,11 Sometimes it may begin late in adolescence and be associated with pronounced hallux valgus.12
It is usually an isolated, unilateral or bilateral condition, with a tendency for spontaneous improvement in up to half of the cases.3 Treatment depends on the severity of the deviation: in mild forms, conservative measures such as “taping” are recommended, which involves the use of bandages that exert forces opposite to the deviation to correct it, or the use of appropriate footwear12; in more severe cases, surgical intervention is recommended, preferably within the first years of life.3
Racket thumbsRacket thumbs are a predominantly female congenital malformation with an autosomal dominant inheritance.13 It is generally an isolated finding, although it has been associated with the Rubinstein-Taybi syndrome and the trichorhinophalangeal syndrome.10,13
Brachyonychia is described as nails in which the width of the nail plate and bed is greater than the length of the nail, contrary to normal conditions. It can occur in isolation or be associated with shortening of the distal phalanx and limited to the thumbs or affect more nails. Numerous syndromes and diseases have been associated with brachyonychia. In racket thumbs, the first fingers of the hand are shortened and widened due to premature closure of the epiphysis, which interrupts the longitudinal growth of the terminal phalanx, while transverse growth goes on.6
Iso-Kikuchi syndromeCongenital onychodysplasia of the index finger is a little-described benign entity. Although its etiopathogenesis is unknown, several theories describe mutations in the Wnt signaling pathway during embryogenesis, changes to the osteogenesis of the phalanx, intrauterine ischemia of arterioles dependent on the radial artery, or the use of teratogenic drugs such as anticonvulsants.14
It is characterized by unilateral or bilateral dysplasia or anonychia of the index fingernail, and sometimes other nails of the hands and feet. It can be associated with underlying bone abnormalities; the most characteristic one is the distal narrowing of the last phalanx of the affected finger or the “Y” morphology of the distal phalanx15 (Fig. 3). There is often no systemic involvement.14
The nail anomalies we can find are very varied: anonychia, micronychia of the ulnar side, polydactyly, hemionychogryphosis, and irregularity or abnormal alignment of the nail plate.14 Baran and Stroud have proposed a series of criteria for its diagnosis: 1) unilateral or bilateral hypoplasia/aplasia of the index finger and/or other fingers; 2) radiological changes to the distal phalanx of the affected finger, and 3) congenital, sporadic, or hereditary (autosomal dominant) disease.16
Congenital curved nail of the 4th toeIt is an autosomal recessive disorder, rarely published in the literature, mainly affecting Asian patients. It shows as a curved nail of the 4th toe from the dorsal to the plantar area, often bilateral, and is accompanied by visible bone disorders on a simple X-ray. Although it is often an isolated condition, it can occasionally be associated with other congenital anomalies.3,11,17
Vertical implantation of the 5th toe nailAlthough it is a rare disorder of unknown etiopathogenesis, a proximal nail fold disorder has been described acting as a guide for normal horizontal nail growth.18 Other authors propose that it is due to the involvement of the underlying phalanx, lateral nail folds, and nail bed.18,19 The 5th toe nail grows in a vertical direction, predisposing it to trauma and, over time, favoring the appearance of aesthetic and functional issues.3,10,11
Congenital double nail of the 5th toe or accessory nail of the 5th toeIt is a common but little-described disorder in the scientific medical literature, probably of an autosomal dominant inheritance with variable expression, although acquired cases have also been published due to trauma.20 It presents as a wider than usual nail, with a longitudinal split that separates it in 2; the part corresponding to the accessory nail is the smallest (Fig. 4). It is often bilateral and bone disorders in the distal phalanx are not a common finding.20–22
Anonychia or micronychiaAnonychia or micronychia is the partial or complete absence of one or more nails and can be congenital or acquired. The congenital form appears more frequently in isolation as a result of a mutation in the RSPO4 and FZD6 genes or as part of a syndrome, such as the nail-patella syndrome or the Iso-Kikuchi syndrome, among others.3,6,8,11,23
LeukonychiaLeukonychia is the white discoloration of the nail. There are various classifications for this condition; depending on the time of onset, we speak of congenital or acquired leukonychia. The latter is the main cause of the nail plate color change in childhood. Other classifications of leukonychia are made depending on where the disorder occurs to differentiate among true leukonychia, apparent leukonychia, and pseudoleukonychia. When considering its morphology, we speak of punctate, transverse, longitudinal, total leukonychia, etc.24.
Congenital leukonychia can appear in isolation and affect all the nails of hands and feet or be syndrome-related. The most important of these is the Bart-Pumphrey syndrome of autosomal dominant inheritance due to a defect in connexin 26. It presents with leukonychia associated with palmoplantar keratoderma and sensorineural hearing loss and, occasionally, koilonychia. Another case has been reported of a family affected by total leukonychia along with pilose dysplasia and acanthosis nigricans-like lesions due to a defect in chromosome 12.24
Pincer nailsPincer nails are characterized by an acquired or congenital increased curvature of the transverse axis of the nail plate. In hereditary cases, there is usually an autosomal dominant inheritance, and nails are symmetrically affected, predominantly the first toes. The acquired form is more common; nail involvement is usually asymmetrical and is related to trauma, systemic diseases, and drugs, among others.24,25
The pincer nail is a nail morphological disorder, generally of the toes, manifested by narrowing of the nail width and excessive transverse curvature, much more prominent from the mid to the distal area.24,25
Hereditary diseasesFong disease or the nail-patella syndromeIt is a rare autosomal dominant disease caused by mutations in the LMX1B gene, located on the long arm of chromosome 9, which encodes the 1-beta factor and regulates the expression of type IV collagen.6,26 The characteristic clinical tetrad includes nail disorders (95% up to 98%), absence or hypoplasia of the patella (90% up to 95%), elbow dysplasia (90%), and iliac horns (70% up to 80%) which are pathognomonic. Additionally, open-angle glaucoma can be found in 30% of patients.26 Nail changes go from aplasia, hypoplasia, and nail dysplasia with longitudinal grooves, to roughness of the nail plate and hypoplasia of the distal part of the nail plate (Fig. 5). Although the triangular lunula is typical of this entity, it has also been observed in trisomy 21 and post-trauma.6 Less frequently, the absence of skin folds on the dorsal part of the distal interphalangeal joint has been reported.6
Fong disease or nail-patella syndrome. Nail hypoplasia of the first, second, fourth, and fifth fingers of both hands with typical triangular lunulae on the third fingers. Additionally, the nail plate of the second, fourth, and fifth fingers of both hands does not reach the free edge of the finger.
Prognosis is determined by renal involvement (12% up to 62%), and it presents with proteinuria, glomerulonephritis of varying severity, and even with end-stage renal disease in 10% of patients. Early diagnosis is essential to avoid possible complications. In this regard, nail disorders play an essential role, as they are visible from birth.6,26,27
Dyskeratosis congenitaDyskeratosis congenita is a rare hereditary disorder of different inheritance patterns, in which a telomerase disorder leads to the premature shortening of telomeres.2–4
The classic clinical triad is characterized by the presence of nail dystrophy, leukokeratosis of the oral mucosa, and abnormal reticulated skin pigmentation.3 Nail changes are the first sign of the condition and usually appear before the first year of life. Fingernails are more affected than toenails, presenting with very lichen-like features with longitudinal grooves and ridges, pterygium, and, in some cases, anonychia.3,4 It can be accompanied by systemic involvement, such as pulmonary disorders, GI disorders, and neoplasms, among others, and in 50% up to 90% of cases of bone marrow failure, which is the main cause of death.3,4,6,8
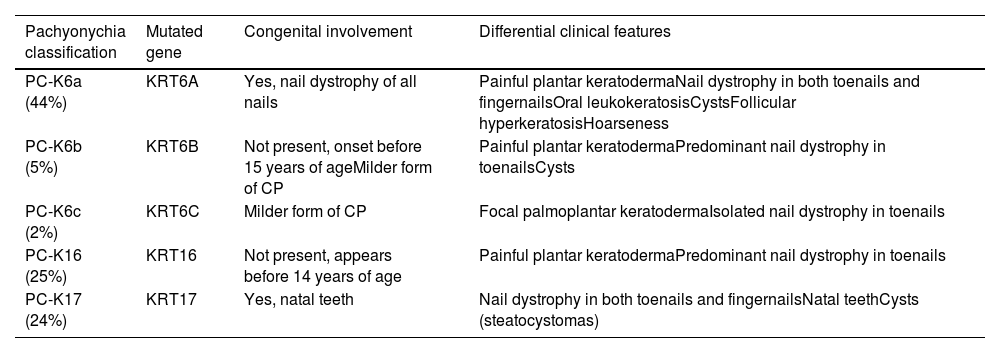
Congenital pachyonychiaIt is a rare genodermatosis characterized by keratinization defects affecting the nails, skin, and mucous membranes. Generally, it follows an autosomal dominant inheritance, although a few cases of autosomal recessive inheritance and acquired cases have been reported.6 In congenital pachyonychia (CP), mutations have been described in the genes associated with keratin. Currently, the classification of CP is based on these 5 mutated genes: PC-K6a, PC-K6b, PC-K6c, PC-K16, and PC-K1728–30 (Table 2). The classical classification divided mutations into 2 phenotype-based subtypes: CP-1 or the Jadassohn-Lewandowsky syndrome—the most common—caused by mutations in the KRT6A and KRT16 keratin genes; and CP-2 or the Jackson-Lawler syndrome, due to mutations in the KRT6B and KRT17 genes.3,6,30
Classification of congenital pachyonychia.
| Pachyonychia classification | Mutated gene | Congenital involvement | Differential clinical features |
|---|---|---|---|
| PC-K6a (44%) | KRT6A | Yes, nail dystrophy of all nails | Painful plantar keratodermaNail dystrophy in both toenails and fingernailsOral leukokeratosisCystsFollicular hyperkeratosisHoarseness |
| PC-K6b (5%) | KRT6B | Not present, onset before 15 years of ageMilder form of CP | Painful plantar keratodermaPredominant nail dystrophy in toenailsCysts |
| PC-K6c (2%) | KRT6C | Milder form of CP | Focal palmoplantar keratodermaIsolated nail dystrophy in toenails |
| PC-K16 (25%) | KRT16 | Not present, appears before 14 years of age | Painful plantar keratodermaPredominant nail dystrophy in toenails |
| PC-K17 (24%) | KRT17 | Yes, natal teeth | Nail dystrophy in both toenails and fingernailsNatal teethCysts (steatocystomas) |
CP, congenital pachyonychia.
Clinical presentation is characterized by the triad of nail dystrophy, palmoplantar keratoderma, and plantar pain.2,4 Nail changes are the earliest signs and are usually present in most cases before the first year of life.4,11 Thickening of the nail plate—predominantly at the distal end—has been reported, along with hyperkeratosis of the nail bed of most nails, although in some patients the toenails are more affected, possibly due to the higher incidence of trauma.6,8,29 The nail thickens and lateral edges curve like a pincer nail. In the early stages, it shows a “V” shape and progressively it acquires a hook-like appearance, with yellow and brown discoloration3 (Fig. 6). At skin level, palmoplantar keratoderma is another early sign of the disease; it is often painful, disabling, and tends to form deep blisters due to friction and pressure, especially when it affects the sole of the foot.2,4,29,30
Congenital pachyonychia in a mother and her child. The toenails show a significant increase in the thickness of the nail plate and nail bed taking on the shape of a hook, along with a white-yellow coloration. Plantar keratoderma can also be seen on the inner edge of the first toe of the left foot. In the fingernails, pachyonychia can also be seen, along with a yellowish-brown coloration.
Depending on the type of CP we’re dealing with, other clinical findings can be observed such as follicular hyperkeratosis, leukokeratosis, dental disorders, or pilosebaceous cysts.4,6,8,29
Treatment is aimed at controlling the pain of plantar keratoderma and nail dystrophy. Systemic retinoids and urea preparations can be useful, while chemical or surgical ablation of the nails is spared for cases that are unresponsive to more conservative therapies.3,8,28,30 Currently, other therapeutic options are being evaluated to improve these patients’ quality of life.30
Congenital epidermolysis bullosaCongenital epidermolysis bullosa is an inherited skin disease characterized by blister formation. It is categorized into 4 types: simple, junctional, dystrophic, and Kindler syndrome.11,31 Nail involvement is very common but is not specific to any type of epidermolysis bullosa, as it results from matrix and nail bed involvement due to blister formation.3,6,8,11 The most common nail disorders are hemorrhagic paronychia, granulation tissue and scarring of the nail bed, pachyonychia, nail atrophy, parrot beak deformity, etc.6,11. In advanced stages of the disease and in severe forms of congenital epidermolysis bullosa, anonychia may occur.3,6,8,11
Ectodermal dysplasiasThese are a heterogeneous group of congenital disorders including about 200 different entities. They are characterized by the abnormal development of ectodermal structures, including the skin, hair, nails, teeth, and sweat glands.4,6 Nail disorders vary depending on the syndrome and are not specific.3,6 The most common phenotype of ectodermal dysplasia is type I or the Christ-Siemens-Touraine syndrome, caused by mutations in the X-linked EDA gene. Clinically, it is characterized by hypo or anhidrosis, koilonychia, hypotrichosis, and hypodontia with conical teeth.13
Tuberous sclerosisTuberous sclerosis is a rare genetic disorder of autosomal dominant inheritance due to mutations in tumor suppressor genes. Loss of functionality of these genes promotes tumor formation in several bodily parts. The major criteria for diagnosis include nail fibromas, known as Koenen's tumors, which appear more frequently in girls during puberty, particularly on the toes.32 They present as single or multiple—usually asymptomatic—reddish or skin-colored papules located on the periungual skin of the proximal nail fold and less frequently at subungual level.32,33 At times they can compress the nail matrix and create a longitudinal groove in the nail plate, even in the absence of a visible lesion.33 Other nail findings include splinter hemorrhages, capillary dilatation in the nail bed with a characteristic “red comet” morphology, and longitudinal leukonychia.33,34 This entity should be suspected in the presence of more than 1 fibroma in children.33
Type I neurofibromatosisType I neurofibromatosis is a rare genodermatosis of autosomal dominant inheritance and an estimated incidence of 1:2,500-3,000 live births. Half of the cases are due to a spontaneous mutation in the NF1 gene while the other half are inherited.35 It is characterized by the appearance of café-au-lait spots, axillary or inguinal freckling, and especially neurofibromas. The latter are benign tumors derived from the sheath of a peripheral nerve and can appear anywhere on the body, including the periungual fold.5,35,36 The presence of glomus tumors in this disease is less well-known; they present as bluish-red macules or as a band of longitudinal erythronychia in the nail bed and are accompanied by a characteristic pain to pressure or temperature changes.36
ConclusionsPhysiological nail disorders in newborns are relatively common and need to be recognized to distinguish them from other pathological conditions. Most of these physiological changes in the nails described within the first few months of life result from the intrinsic fragility of the nail at birth and resolve spontaneously with growth. Attention should be paid to unusual nail disorders whether they appear in the early years of life, childhood, or adolescence, as they may be the early signs of a more complex syndrome often accompanied by other skin and organ abnormalities.
Conflicts of interestNone declared.