A 27-year-old man with no relevant medical history presented with a scrotal lesion, preceded by localized pruritus, that had appeared in the previous 24hours. He reported painful swallowing, had a temperature of 38°C, and denied ingestion of drugs or toxic substances, engagement in high-risk sexual practices, local injury, and application of topical products.
Physical ExaminationPhysical examination revealed an ulcer of 30×25mm with necrosis in the center and slightly erythematous edges located on the right side of the scrotum (Fig. 1). There were no palpable lymph nodes in the groin area. Examination of the throat revealed extensive pharyngeal and tonsillar erythema.
Additional TestsBlood tests showed increased total leukocytes and acute phase reactants. Ultrasound examination of the soft tissue and Doppler ultrasound showed no evidence of epididymal or testicular abnormalities.
Serology for viruses (human immunodeficiency virus, hepatitis B virus, parvovirus B19, cytomegalovirus, Epstein–Barr virus) and syphilis were negative. Staphylococcus epidermidis was isolated in a culture from the base of the ulcer, although this was interpreted as a probable case of contamination. The direct immunofluorescence study and culture for herpes simplex virus were negative.
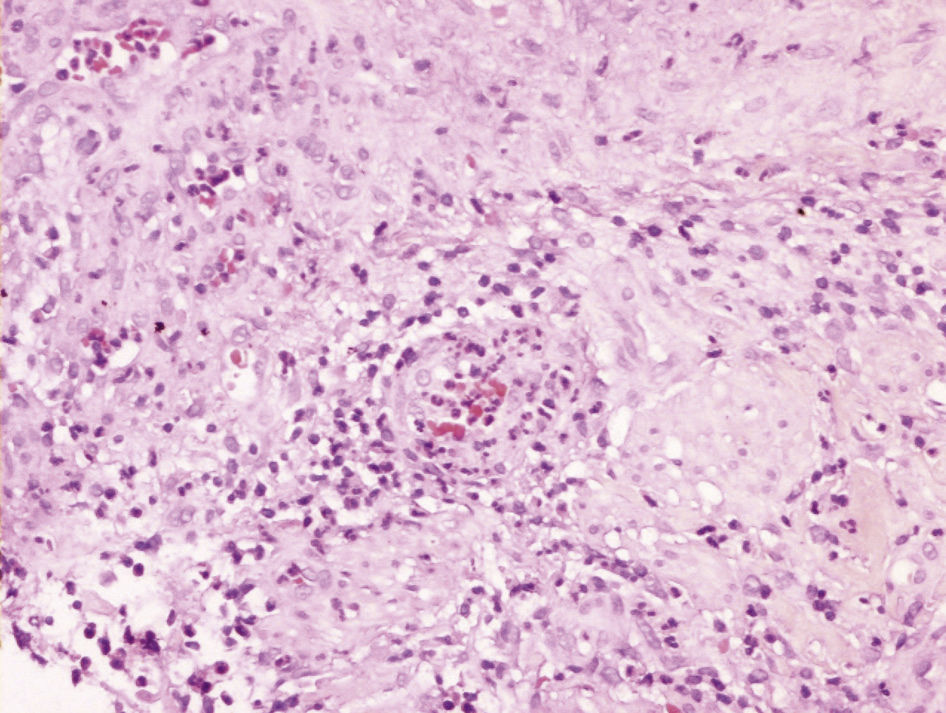
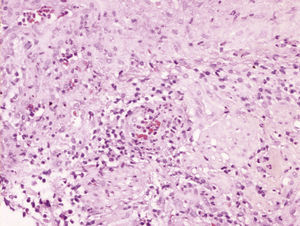
Biopsy of the edge of the ulcer showed a dense neutrophilic inflammatory infiltrate in the dermis, with a predominant perivascular distribution. Foci of neutrophil aggregates were seen in the walls of the small and medium-sized vessels, with no evidence of fibrinoid necrosis (Fig. 2).
What Is Your Diagnosis?
DiagnosisJuvenile gangrenous vasculitis of the scrotum.
Clinical CourseOnce other potentially serious causes of scrotal ulceration had been ruled out, the lesion was treated daily with physiological saline solution and petrolatum-impregnated dressings to provide protection. The pharyngeal and tonsillar erythema disappeared in 5 days and the ulcer healed gradually, resulting in complete reepithelialization. No new lesions were detected at follow-up.
DiscussionJuvenile gangrenous vasculitis of the scrotum is a variant of scrotal gangrene with unique clinical and histopathological characteristics first described by Piñol et al.1 The etiology is unknown and the condition presents almost exclusively in healthy young adults. Pruritus and/or burning in the scrotal area precedes the appearance of 1 or several areas of cutaneous necrosis. The infection tends to be accompanied by an increase in body temperature with no clear source of infection. Pharyngeal and tonsillar infection is common in the preceding days or weeks. Blood tests reveal increased total leukocytes and acute phase reactants. Blood cultures are sterile and no microorganisms are isolated from the lesions. Tests for antinuclear antibodies are negative and evaluation of other parameters indicative of autoimmune response gives normal values. Histopathology shows an area of extensive epidermal necrosis accompanied by a dense inflammatory infiltrate consisting of neutrophils. These polymorphonuclear leukocytes can invade the vessel walls, and imaging techniques reveal leukocytoclasia, without fibrinoid necrosis, in the walls of the small blood vessels of the dermis. However, focal presence of fibrinoid necrosis does not rule out a diagnosis of juvenile gangrenous vasculitis of the scrotum.2–4 The condition resolves spontaneously in less than a month, although good hygiene and suitable dressings around the lesion can accelerate reepithelialization. Nonrecurrence is listed as a main diagnostic criterion for this condition. Differential diagnosis should include other causes of acute scrotal ulceration such as Fournier gangrene, Behçet disease, polyarthritis nodosa, herpes virus infections, primary syphilis, trauma-induced scrotal ulcers, dermatitis artefacta, pyoderma gangrenosum,5 and cocaine consumption,6 among others.
In summary, we present the case of a rare and generally little-known entity that is significant for its benign course and clinical similarity to other causes of scrotal ulceration that have different therapeutic and prognostic implications.
Please cite this article as: Pulido-Pérez A, et al. Úlcera escrotal aguda. Actas Dermosifiliogr. 2012;103:239–40.