Pigmented purpuric dermatoses (PPD) are a group of eruptive disorders characterized by petechiae and pigmentation affecting principally the lower limbs. These disorders follow a benign and chronic course punctuated by remissions and exacerbations; the etiology is unknown. Histopathology reveals a perivascular lymphocytic infiltrate and red blood cell extravasation in the early stages and hemosiderin-laden macrophages in mature lesions. Various treatments have been used, including include oral and topical corticosteroids, ciclosporin, pentoxifylline, oral bioflavonoid preparations, ascorbic acid, and phototherapy; results have been variable.1 Phototherapy is a widely used dermatologic treatment that has been shown to be effective in patients with PPD.2–4 We report a case in which PPD lesions resolved completely after narrow-band (NB) UV-B therapy.
The patient was a 74-year-old man who presented with somewhat itchy lesions in the lumbosacral region, buttocks, and thighs that had developed 3 months earlier (Fig. 1). He had no medical history of interest). Skin biopsy showed a perivascular lymphocytic infiltrate in the superficial dermis and the basal layer of the epidermis and extravasation of red blood cells. No significant abnormalities were found in complete blood count, liver or kidney function tests, protein electrophoresis, or biochemistry. Antinuclear antibodies and cryoglobulins were not detected on analysis. A diagnosis of pigmented purpuric lichenoid dermatosis of Gougerot and Blum was established, and NB–UV-B treatment was started with a frequency of 3 times per week following the standard phototherapy protocol for the patient's skin phototype. The starting dose was 150mJ/cm2 with 20% increments in sessions 2 and 3 followed by 10% increments per session up to the maximum tolerated dose. Complete clearance of the lesions was observed after 20 sessions and the patient was changed to a bi-weekly phototherapy regimen up to a maximum of 30 sessions and a cumulative dose of 25J/cm2 (Fig. 2). No PPD lesions reappeared during 9 months of follow up.
PPDs are chronic, benign, and usually asymptomatic eruptions.5 They are mainly classified according to the location and morphology of the lesions and a common pathogenesis is likely. Owing to the marked clinical and histopathological overlap between specific PPDs, they are considered to represent the spectrum of a single disease. The etiology is unknown, although some authors have advanced the hypothesis that PPDs are caused by weakened cutaneous blood vessels leading to capillary fragility. It has also been suggested that the presence of a perivascular infiltrate consisting of CD3+, CD4+, and dendritic CD1+2 cells indicates a mechanism involving cellular immunity. The inflammatory infiltrate and the skin lesions may disappear following the topical application of high-potency corticosteroids or after treatment with psoralen UV-A (PUVA) therapy.1 The good response to phototherapy can probably be explained by this immunomodulatory mechanism.6 There is no consensus on the most appropriate treatment for this group of disorders. Since PPDs affect large areas of the skin but have a benign course, phototherapy is a good therapeutic option compared to topical or systemic treatments, which are of doubtful efficacy.
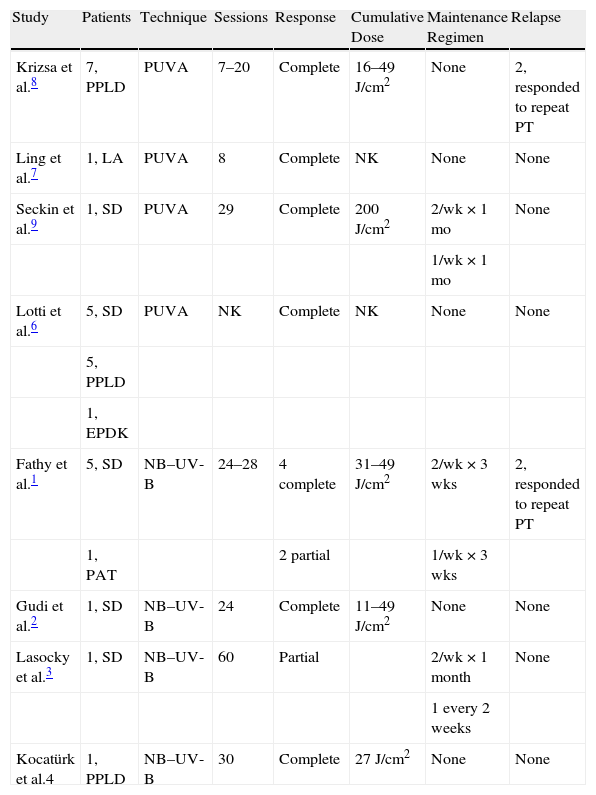
PUVA therapy has been shown to be effective in patients with Schamberg disease, lichenoid purpuric dermatosis, and lichen aureus (Table 1).7–9 Remission is reported between sessions 7 and 20, and in 2 cases of subsequent relapse and exacerbation, a second cycle of treatment once again achieved remission. Phototherapy may modify T-cell activity and decrease the production of IL-2, thereby achieving clearance of lesions. After the reported successes with PUVA treatments, good response to NB–UV-B was also reported.1–4 Significant clearance has been achieved even after 20 sessions, and most authors recommend continuing with a maintenance regimen of 1 session every 1 or 2 weeks for 2 to 3 months to prevent relapse. The cumulative doses reported range from 11 to 49J/cm2. NB–UV-B treatment has also been shown to be effective in treating recurrence.1The authors of one study reported that NB–UV-B therapy at 311nm induced T-cell apoptosis in the dermis and epidermis in plaque psoriasis.10 This mechanism may also explain the resolution of PPD lesions. Because phototherapy acts on the inflammatory component of PPD, findings that predict response to therapy might be a predominantly lichenoid lymphocytic infiltrate and a recent appearance of lesions. As red blood cell extravasation and hemosiderin deposits would not be affected by the anti-inflammatory effect of phototherapy, their presence could be predictive of a negative response. Extravasation of red blood cells and hemosiderin deposits are more common in lichen aureus and in long-standing lesions.1–4
Reported Cases of Pigmented Purpuric Dermatoses Treated With Phototherapy.
| Study | Patients | Technique | Sessions | Response | Cumulative Dose | Maintenance Regimen | Relapse |
| Krizsa et al.8 | 7, PPLD | PUVA | 7–20 | Complete | 16–49J/cm2 | None | 2, responded to repeat PT |
| Ling et al.7 | 1, LA | PUVA | 8 | Complete | NK | None | None |
| Seckin et al.9 | 1, SD | PUVA | 29 | Complete | 200J/cm2 | 2/wk×1 mo | None |
| 1/wk×1 mo | |||||||
| Lotti et al.6 | 5, SD | PUVA | NK | Complete | NK | None | None |
| 5, PPLD | |||||||
| 1, EPDK | |||||||
| Fathy et al.1 | 5, SD | NB–UV-B | 24–28 | 4 complete | 31–49J/cm2 | 2/wk×3 wks | 2, responded to repeat PT |
| 1, PAT | 2 partial | 1/wk×3 wks | |||||
| Gudi et al.2 | 1, SD | NB–UV-B | 24 | Complete | 11–49J/cm2 | None | None |
| Lasocky et al.3 | 1, SD | NB–UV-B | 60 | Partial | 2/wk×1 month | None | |
| 1every 2 weeks | |||||||
| Kocatürk et al.4 | 1, PPLD | NB–UV-B | 30 | Complete | 27J/cm2 | None | None |
Abbreviations: EPDK, eczematid-like purpura of Doucas and Kapetanakis; LA, lichen aureus; NB, narrow band; NK, not known; PAT, purpura annularis telangiectodes; PPLD, pigmented purpuric lichenoid dermatosis; PT, phototherapy; PUVA, psoralen UV-A therapy; SD, Schamberg disease.
Phototherapy is a treatment option in PPDs, especially when lesions are extensive and symptomatic. Good results have also been achieved in some cases of recurrent disease.
Please cite this article as: Ciudad C, et al. Respuesta satisfactoria de la dermatosis purpúrica pigmentada al tratamiento con fototerapia. Actas Dermosifiliogr. 2013;104:439-40.