Squamous cell carcinoma is a rapidly growing tumor that can cause local damage and also has metastatic potential. Reconstruction of the nasal pyramid is a challenge for the surgeon as not only should functionality be maintained but the esthetic impact should also be minimized.
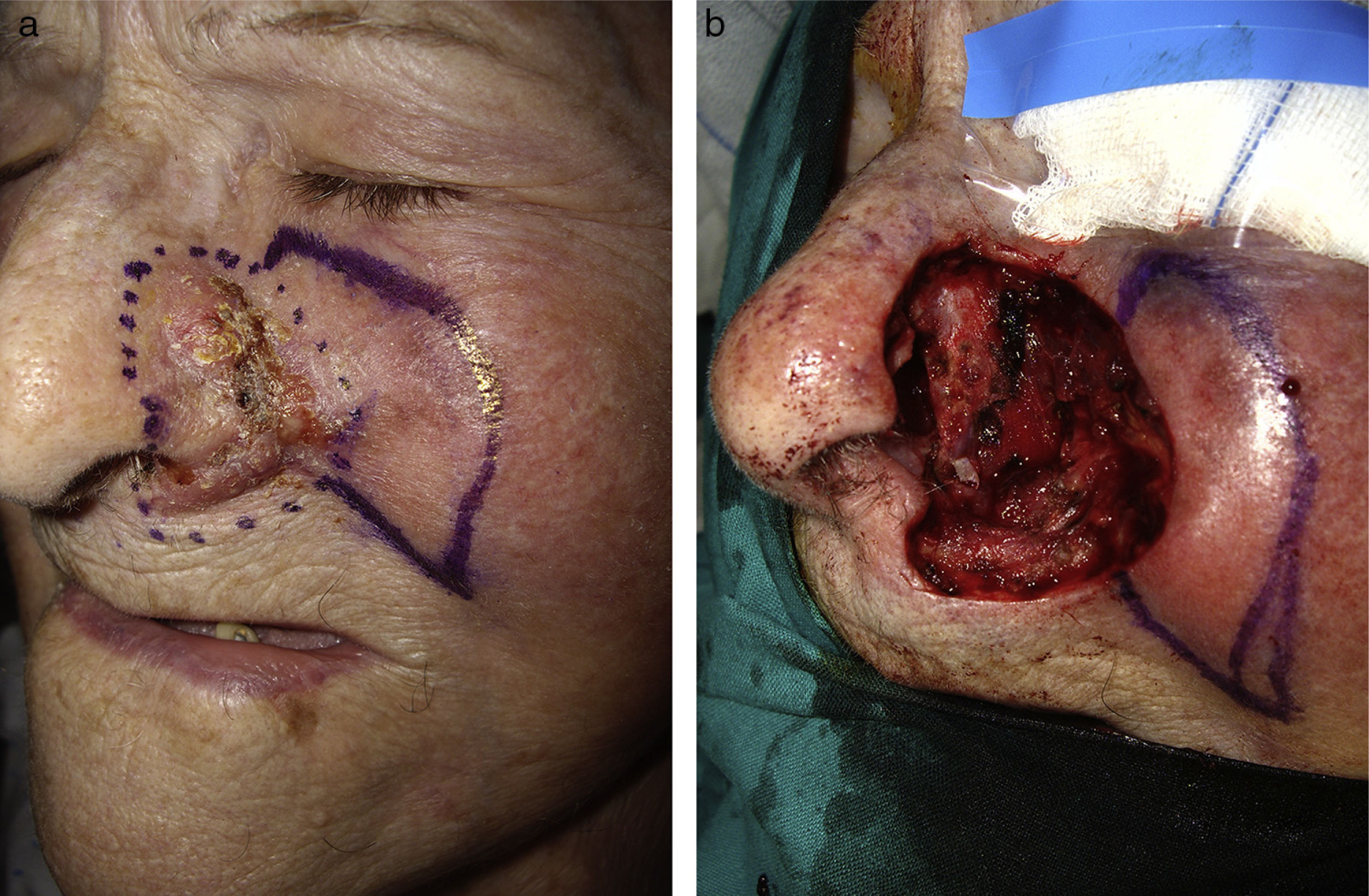
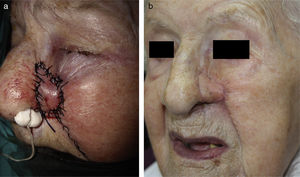
We present the case of a 97-year-old woman who attended our clinic with a very painful, fast-growing tumor, first noted 4 months earlier. The lesion, on the left nasal ala, was an ulcerated tumor and measured 3.5×4.5cm in its longest diameter (Figure 1). Biopsy confirmed the suspected diagnosis of squamous cell carcinoma and surgical excision was indicated.
The entire nasal ala was excised under local anesthetic, with a 5mm margin, including the mucosal and cartilaginous layers as well as the tissue adjacent to the upper lip and left malar region (Figure 1B). Given that most of the nasolabial fold had been excised, it was decided to use a malar turnover island pedicle flap for reconstruction.
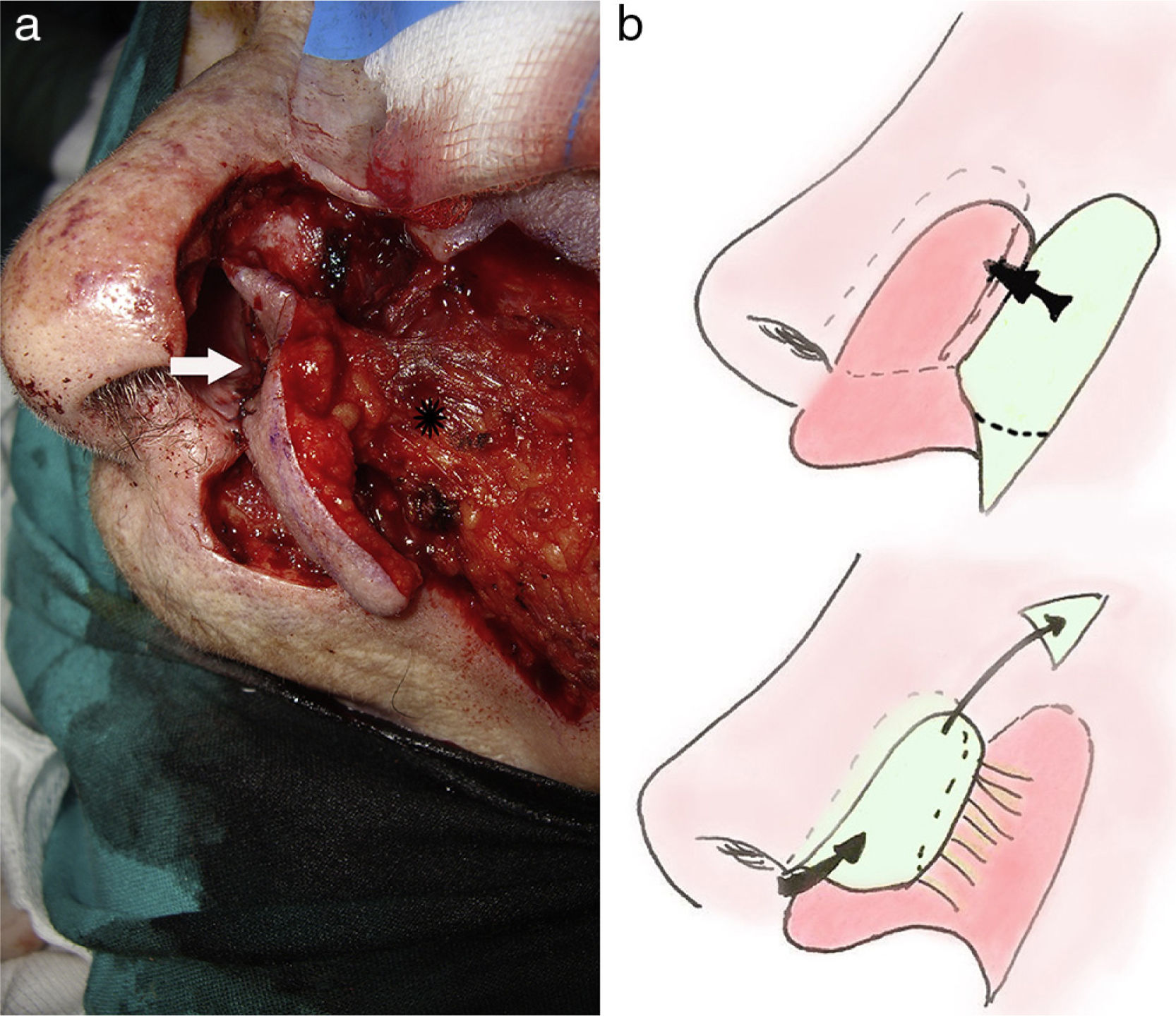
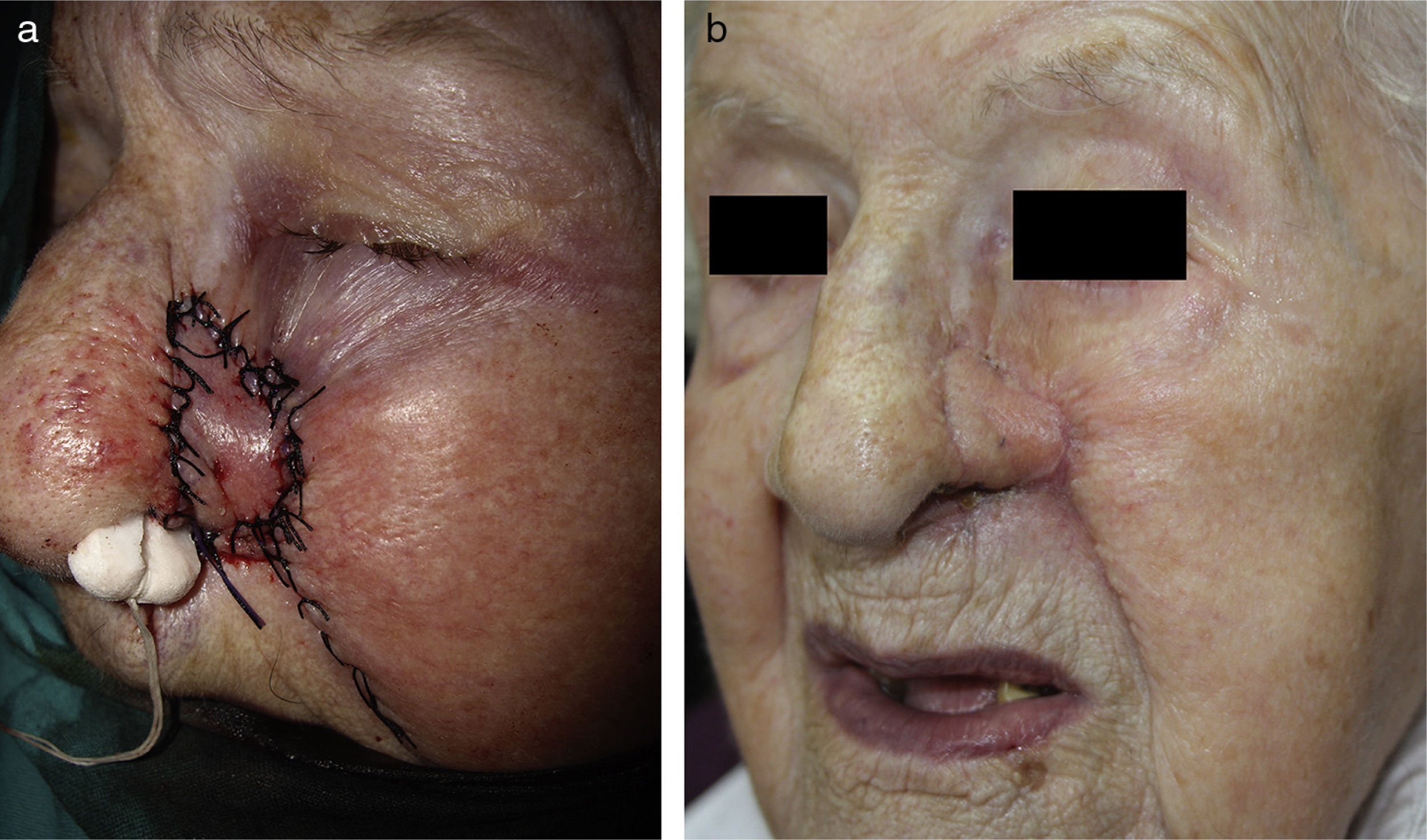
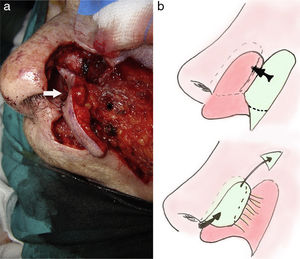
The design of the skin island flap aligned the upper edge with the upper border of the mucosal defect. The lower half of the flap was marked out to reflect the length of the nasal skin defect. The pedicle of the flap was dissected below the subcutaneous cell tissue, such that it retained a diameter of at least 1.5cm and its base was located in the most proximal part of the surgical defect (Figure 2A), retracting the subcutaneous tissue from the base of the rest of the flap. After turnover of the island, the mucosal defect was sutured with resorbable material (Figure 2A [arrow] and B). A guide suture (single 4-0 silk stitches) was used along the edge of the nasal ala. After layer closure of the defect of the upper lip and the malar area using an advancement flap, the flap was folded onto the nasal ala and the skin defect was reconstructed. The flap was cut to adapt it to the defect and sutured (Figure 3) with single stitching with nonresorbable material (4-0 silk). A transfixion suture was used for the alar flap to facilitate its complete coaptation and avoid ischemia. Antibiotic prophylaxis was prescribed and anterior nasal packing was applied with a compressive dressing for the first 48h.
The postoperative period was satisfactory, with no complications. The stiches were removed 7 days after the operation. The nasal cavity did not collapse and good ventilatory function was maintained (Figure 3B).
Complete reconstruction of surgical defects in the nasal ala is often encountered in everyday surgical practice. Traditional use of the nasolabial fold is not practical in cases in which the surgical defect includes this region. In 1987, Spear et al.1 reported a variation of the nasolabial flap in which the flap was inverted, maintaining the subcutaneous pedicle. The turnover malar flap of the subcutaneous pedicle is a variant of this procedure and extremely useful when the surgical defect includes the nasolabial fold.
In the design, the cutaneous island should be adjusted to the size of the defect. The width should be the same as the horizontal size of the region to be reconstructed. The length should be at least twice that of the defect to enable mucosal and cutaneous reconstruction. The pedicle should be cut to a depth of 2-3mm at the level of the subcutaneous cellular tissue. The distal three-quarters of the pedicle should be freed from the underlying tissue, with only one-quarter remaining anchored.2 Excess fatty tissue in the island should be removed to improve the esthetic result.3 It is recommended to prescribe antibiotic prophylaxis both intraoperatively and postoperatively in these patients.4
The complications are those inherent in all flap interventions. Necrosis is generally caused by an insufficiently large or twisted pedicle. The trap door effect may not necessarily occur if the fatty material is removed from the flap. It should be remembered that there may be facial hair on the nasal pyramid, and this could be avoided by leaving out hair-covered areas when designing the cutaneous island.
A major limitation lies in the absence of cartilaginous structure or support, which would not only improve the esthetic outcome, but would also prevent collapse with inspiration. This could be overcome by adding a free cartilage graft from the concha of auricle5,6 or a titanium mesh,5 although such procedures were considered unnecessary in this case given the age of the patient. Other reconstruction options requiring a single intervention are nasolabial transposition flap or subcutaneous turnover pedicle,1,7 but these are not useful in this case because the surgical defect would include this region.
Reconstructive surgery was performed in a single intervention of the nasal ala and perialar region, using a malar turnover island pedicle flap. The functional and esthetic outcomes were good. This technique is a very useful tool for the reconstruction of large defects in the nasal ala with involvement of the nasolabial fold, which rules out use of this structure for the flap design.
Please cite this article as: Godoy-Gijón E, Palacio-Aller L, González-Sabin M. Reconstrucción del ala nasal mediante colgajo malar invertido de pedículo subcutáneo. Actas Dermosifiliogr. 2015;106:233-235.