Oxalosis is a disease caused by the deposition of calcium oxalate in extrarenal tissues, most commonly bone, myocardium, retina, blood vessels, and skin, causing the clinical manifestations of the disease. Involvement of the blood vessels of the skin can give rise to livedo reticularis, acrocyanosis, ulcers, and gangrene. We present the case of a 60-year-old woman with a history of recurrent renal lithiasis that had led to terminal renal failure requiring hemodialysis and, subsequently, peritoneal dialysis. The patient developed tender red-violaceous skin discoloration of sudden onset, consistent with livedo reticularis; the lesions progressed to form ulcers. Skin biopsy revealed oxalate vasculopathy. In this article we describe the characteristics of this rare disorder, its differentiation from calciphylaxis, and the therapeutic options.
La oxalosis es una enfermedad derivada del depósito de oxalato cálcico fuera del aparato urinario. Los lugares de depósito extrarrenales más frecuentes incluyen el hueso, el miocardio, la retina, los vasos sanguíneos y la piel, lo que da lugar a las manifestaciones clínicas de esta enfermedad.
En la piel las alteraciones pueden deberse a la afectación de los vasos sanguíneos, lo que da lugar a la aparición de cuadros de livedo reticularis, acrocianosis, úlceras y gangrena.
Presentamos el caso de una mujer de 60 años con historia de litiasis renal recidivante, que le llevó a una insuficiencia renal terminal que requirió hemodiálisis y posteriormente diálisis peritoneal. La paciente desarrolló de forma súbita la aparición de elementos cutáneos de color rojo-violáceo, dolorosos a la palpación compatibles con livedo reticularis que evolucionaron a úlceras. La biopsia cutánea reveló una vasculopatía por oxalato.
En este artículo se describen las características de este raro proceso, su diagnóstico diferencial con la calcifilaxis y las alternativas terapéuticas.
Oxalosis is defined as the systemic accumulation of calcium oxalate, an insoluble salt of oxalic acid, outside of the urinary tract. The pathologic processes responsible for systemic oxalosis include primary and secondary hyperoxalurias. Kidneys, bone, myocardium, blood vessels, and skin are the sites most susceptible to oxalate deposition and, therefore, to the appearance of clinical manifestations of oxalosis.
The cutaneous findings associated with primary hyperoxaluria are usually caused by oxalate deposition in the blood vessel walls; this can cause livedo reticularis, acrocyanosis, ulceration, and peripheral gangrene. Skin changes caused by hyperoxaluria secondary to renal insufficiency, however, are rare. When such changes do occur, they are the result of extravascular calcium oxalate deposition, which leads to the appearance of calcified nodules and milium-like papules.
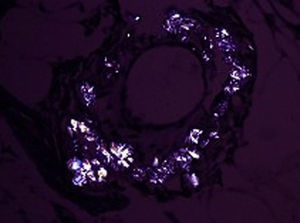
Case DescriptionThe patient was a 60-year-old woman with terminal renal failure secondary to chronic lithiasic pyelonephritis who had been on hemodialysis followed by peritoneal dialysis for 3 years. She presented red-violaceous, racemose, macular skin lesions that had appeared suddenly on the lower limbs and were very tender to palpation (Fig. 1).
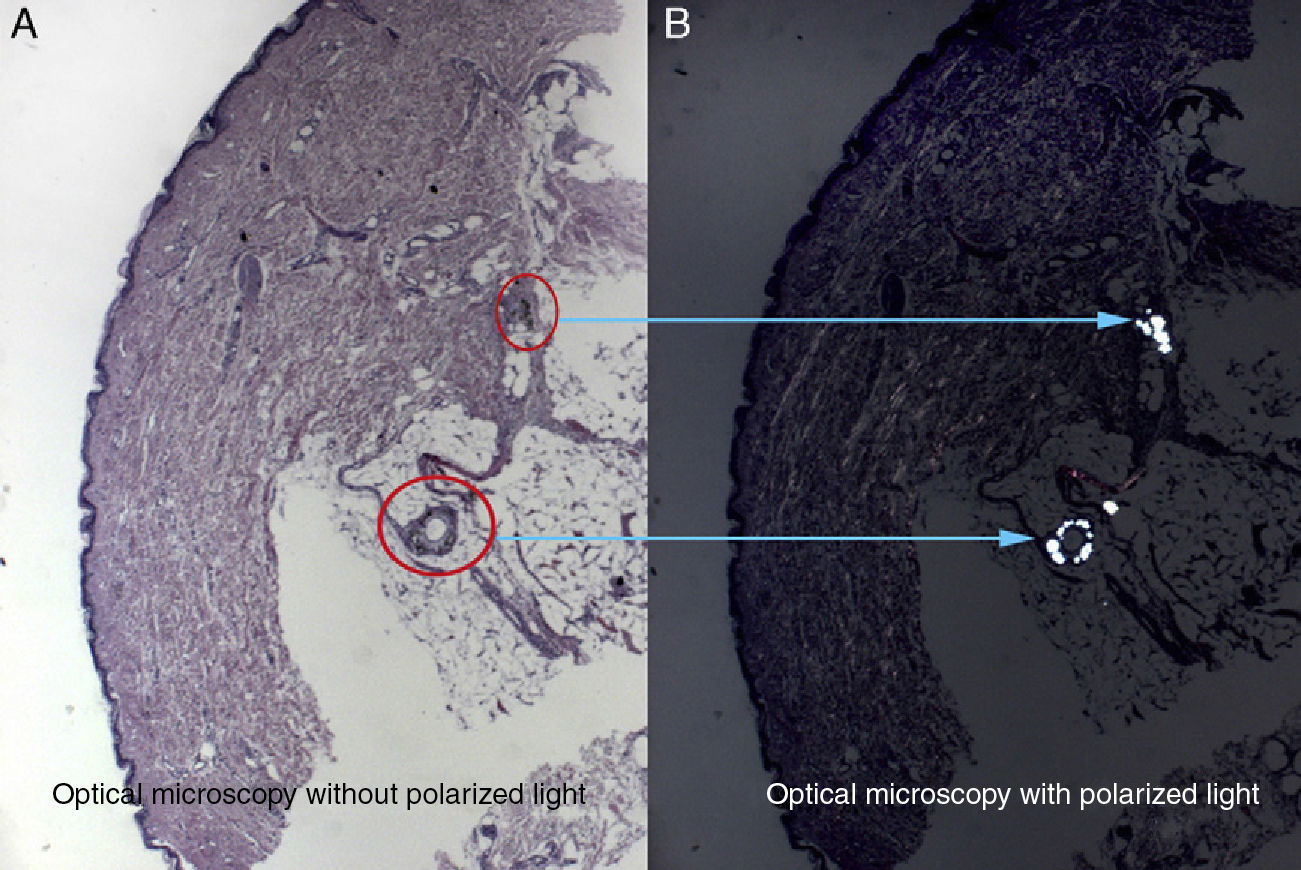
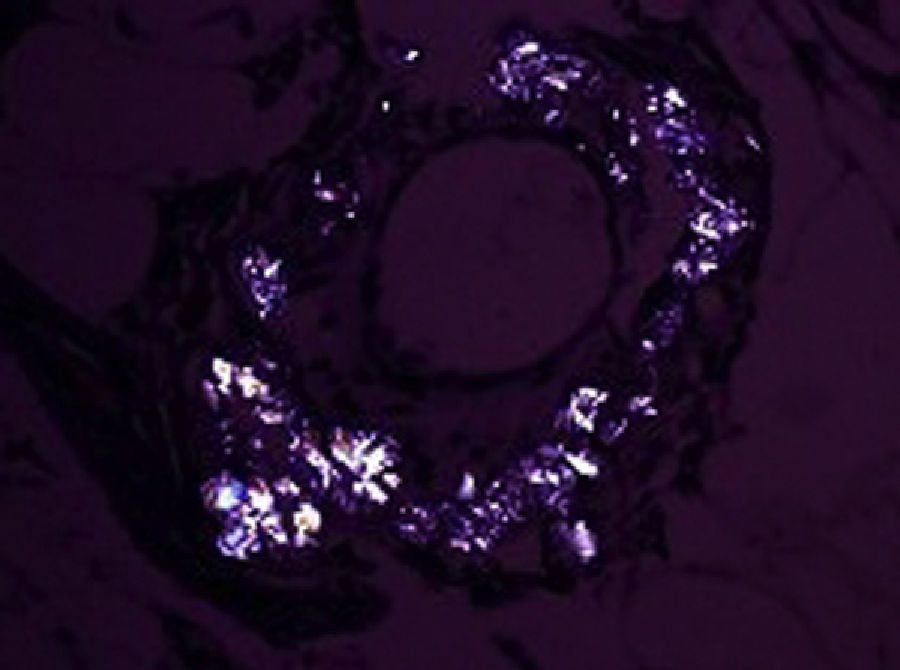
Biopsy revealed the presence of deposits composed of a brownish material in the media of arterioles in the reticular dermis and hypodermis (Fig. 2 A) The deposits were intensely birefringent under polarized light (Fig. 2 B) and the classic spiculated crystals of oxalate salts were observed (Fig. 3). Fat necrosis was also observed. On the basis of these histopathologic findings, a diagnosis of oxalate crystal–induced vascular disease was established.
A review of the patient's records revealed that she had had repeated episodes of nephrolithiasis in both kidneys since the age of 40 years. Previous tests had found a 24-hour urinary oxalate level of 101mg/1.73m2 (normal range, 4-44mg/1.73m2); at the time the patient was seen in our clinic, the level of oxalic acid in the blood was 11.3mg/l (normal value, <6mg/l). The results of further tests to rule out the possibility of associated calciphylaxis (calcium levels, phosphorus levels, and arteriography) were normal. Electrocardiography and echocardiography showed no evidence of cardiac involvement and funduscopy revealed no retinal deposits.
The patient's clinical state gradually worsened. The livedo reticularis increased in intensity on all of the limbs and necrosis appeared on the left heel, the buttocks, and the tips of the second and third fingers of the right hand. She subsequently developed acute, intense abdominal pain, vomiting, and refractory hypotension that led to her death.
DiscussionIn a patient with terminal renal failure and a history of lithiasis, the appearance of livedo reticularis should alert the clinician to consider a diagnosis of hyperoxaluria.1
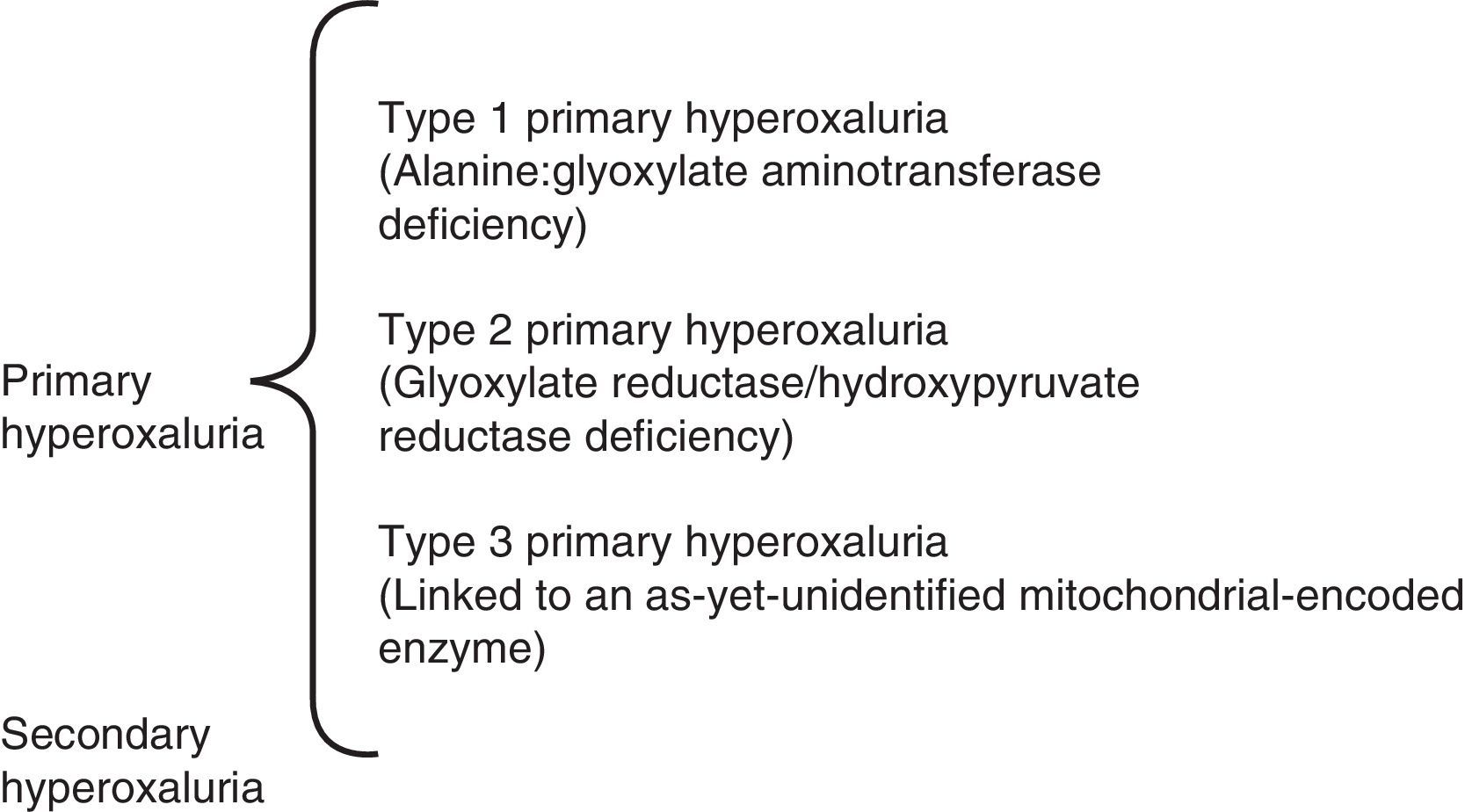
Hyperoxaluria is classified as primary or secondary (Table 1). The primary hyperoxalurias, which have an autosomal recessive inheritance, are divided into various subtypes that are distinguished from one another on the basis of the enzyme deficiency in the hepatocytes. Type 1 primary hyperoxaluria is the most common. It is caused by a deficiency of the pyridoxine-dependent hepatic peroxisomal enzyme alanine:glyoxylate aminotransferase. The gene that encodes this protein consists of 11 exons located on chromosome 2q37.3. About 30 mutations of this gene have been described to date. Type 2 primary hyperoxaluria is caused by a deficiency of the cytosolic enzyme glyoxylate reductase/hydroxypyruvate reductase. Type 3 primary hyperoxaluria is linked to a mitochondrial-encoded enzyme. It is likely that other as-yet-unidentified alterations also exist.2,3 Secondary hyperoxaluria, which is caused by excessive oxalate intake, is seen in the context of other processes, including hemodialysis.4 Because oxalate is excreted only via the kidneys, renal failure of any origin that requires hemodialysis can lead to the saturation of oxalate salt in the tissues, but always to a lesser extent than in the primary hyperoxalurias. The excess oxalate precipitates as calcium oxalate, first in the kidneys and later in other tissues. It has been suggested that the appearance of renal calculi caused by primary hyperoxalurias—smooth, whitish surface, unorganized section, and pure or virtually pure calcium oxalate monohydrate composition—is different from that of common calculi.5
Cutaneous manifestations of hyperoxaluria are uncommon and very few cases have been reported in the literature.6–10 Most skin lesions of the primary hyperoxalurias are caused by vascular complications resulting from oxalate deposition in the arterial walls, which leads to the appearance of livedo, acrocyanosis, and gangrene. In secondary hyperoxaluria, mild cutaneous manifestations are caused by extravascular deposition, which leads to the appearance of acral or facial papules or nodules.11
Our patient's advanced age at the time of diagnosis is noteworthy. Primary hyperoxalurias generally have an early onset, between the ages of 7 and 13 years; however, there have been cases, like that of our patient, in which the disease presents in the sixth decade of life. Because of their rarity, the primary hyperoxalurias are usually diagnosed between 24 and 33 years of age, by which time many patients have already developed terminal renal failure. Diagnosis of the primary hyperoxalurias is very challenging for clinicians.12 Measurement of 24-hour urinary oxalate levels, L-glycerate levels, and the oxalate to creatinine ratio can be useful in the diagnostic process. However, once the patient has developed anuria these tests are no longer relevant. When a primary hyperoxaluria is suspected, the clinician can measure serum oxalate levels (which were very high in our patient) and, depending on the results, order liver biopsy and genetic testing (which our patient did not undergo, due to her rapid deterioration and death). We suspect that our patient died as a result of acute mesenteric ischemia, which has been described as a frequent cause of death in patients with primary hyperoxaluria.13
The differential diagnosis should particularly include calciphylaxis. Calciphylaxis has clinical manifestations similar to those found in our patient, but it is usually seen in patients who are on long-term hemodialysis, have alterations of the calcium/phosphorus product or of parathyroid hormone levels, or who present radiologic and histopathologic findings of soft-tissue calcification with basophilic calcium deposits.14
Treatment of hyperoxaluria depends on the cause. Patients who retain kidney function can be prescribed oral pyridoxine, which increases the activity of the deficient liver enzyme by acting as a cofactor. In patients who have developed renal failure, the only effective treatment is a combined liver and kidney transplant. Because the liver is the site of the enzyme problem, it must be transplanted at the same time as the kidney. Conventional dialysis is not suitable for patients with renal failure because it cannot eliminate the excess oxalate synthesized in the liver. Hemodialysis is more effective than peritoneal dialysis in eliminating oxalate.15 Our patient's switch to peritoneal dialysis could explain the appearance of her cutaneous manifestations.
In summary, we have presented the case of a 60-year-old woman with a history of recurrent nephrolithiasis and terminal renal failure who developed livedo reticularis and skin necrosis after starting a program of peritoneal dialysis. Histopathology revealed the existence of calcium oxalate deposits in the arterial walls, which supported a diagnosis of an underlying primary hyperoxaluria. The patient's condition then deteriorated rapidly and she died a few months later, before the type of primary hyperoxaluria could be confirmed by genetic testing or liver biopsy.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for the purpose of this study.
Confidentiality of data.The authors declare that no patient data are disclosed in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Jorquera-Barquero E, Súarez-Marrero MC, Fernández Girón F, Borrero Martín JJ. Oxalosis y livedo reticularis. Actas Dermosifiliogr. 2013;104:815–818.