Spiradenocarcinoma is a very rare malignant tumor that arises from a preexisting spiradenoma of a sweat gland.1
We present the case of a 72-year-old woman with a history of systemic hypertension. She came to our outpatients for a tumor that had appeared 40 years earlier and that had increased progressively in size; this growth had accelerated over the previous 6 years. The tumor was situated over the middle third of the left clavicle and measured 13×10×7cm. It was firm to palpation, had a smooth and shiny surface with telangiectasias, well-defined borders, and was not adherent to deeper planes (Fig. 1). It was not tender. There were no palpable lymph nodes. The patient denied weight loss.
We considered a soft-tissue tumor and therefore performed ultrasound study, which demonstrated a cystic lesion in the subcutaneous cellular tissue of the supraclavicular region; the muscle planes were not affected. The lesion was excised surgically, including the subcutaneous cellular tissue. The center of the tumor was pasty or semiliquid, and firm nodules were present at each pole.
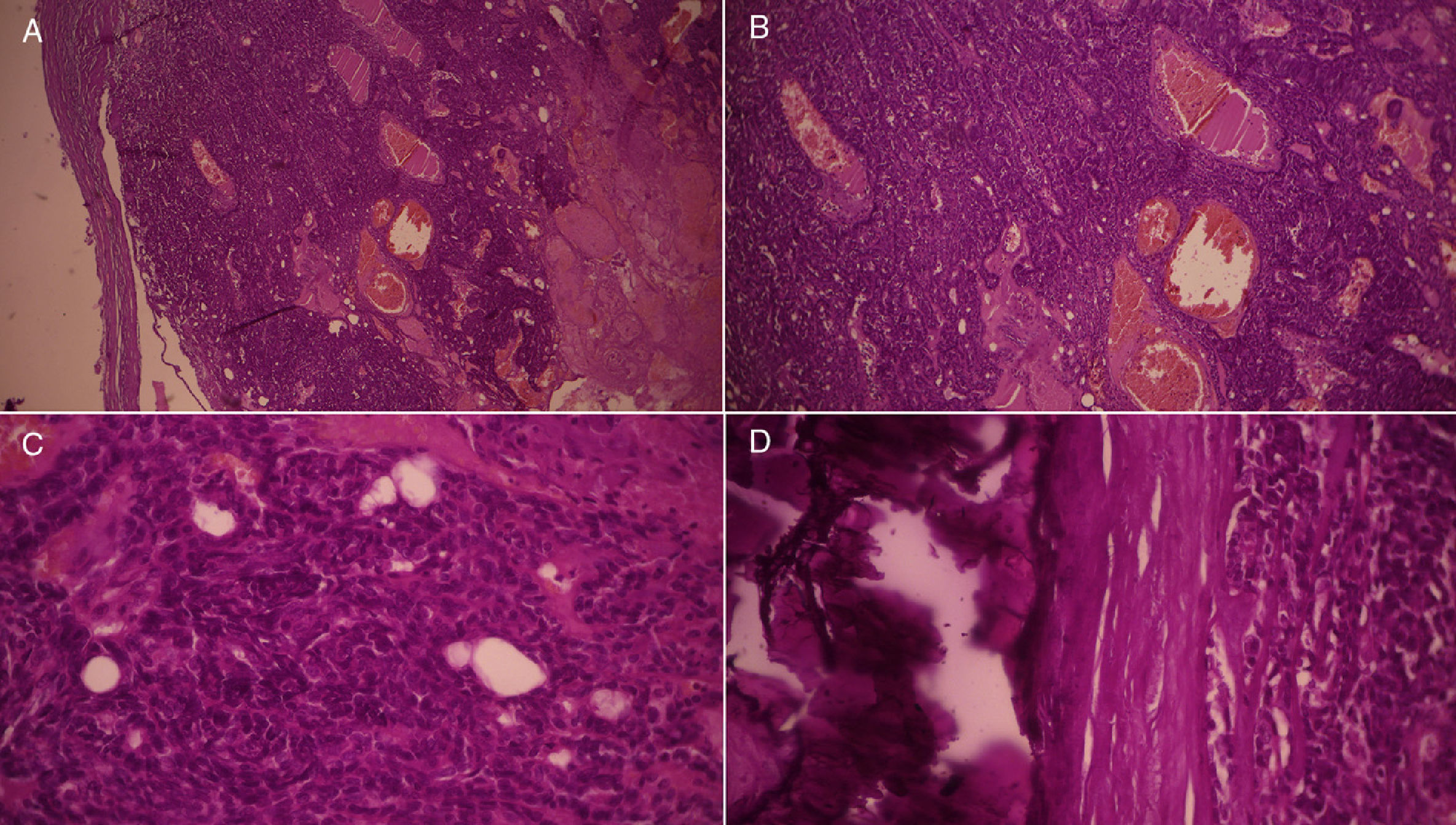
Histology revealed nodules of epithelial cells that, in some areas, had a peripheral cell population with a basaloid appearance, and cells with scant clear cytoplasm that lined tubular glandular lumina. In other areas, the cells showed less differentiation, with a clear predominance of hyperchromatic basaloid cells with scant cytoplasm; no ductal structures were present. Mitoses were observed (1 per high-power field). Calcification was also observed and the stroma presented edema and dilated and congested vascular channels (Fig. 2). Based on these findings, we made a diagnosis of malignant spiradenoma. Eighteen months after the operation, there were no signs or images of recurrence.
A and B, Nodules of epithelial cells that, in some areas, have a peripheral population of cells with a basaloid appearance. A, Hematoxylin and eosin (H&E), original magnification ×4; B, H&E, original magnification ×10. C and D, Cells with scant, clear cytoplasm lining tubular glandular lumina; in other areas, the cells show less differentiation, with a clear predominance of hyperchromatic basaloid cells with scant cytoplasm. No ductal structures are formed. Mitoses are present. Calcification is present and the stroma shows edema and dilated and congested vascular channels. H&E, original magnification ×40 in both images.
Malignant spiradenoma is a rare tumor. Malignant tumors of the sweat glands account for approximately 0.005% of all skin tumors. Age at presentation varies from 21 to 92 years. In two thirds of patients, the diagnosis is made after age 50 years,2 and only 1 pediatric case has been reported.3 The majority of patients describe a rapid growth of the tumor, a change in color, or ulceration, and this prompts them to seek medical care.2,4
Diagnosis is based on clinical suspicion and is confirmed by histology, which shows malignant changes in areas of the spiradenoma.5 Sometimes the diagnosis can be difficult, and histology of the whole tumor is required to be able to observe the architecture of the lesion.6 The benign part accounts for 5% to 40% of the tumor.7 Some markers can be helpful to differentiate the malignant part; for example, in the malignant part, the Ki-67 proliferation index is increased whereas MYB expression is negative.7 Four histologic patterns of spiradenocarcinoma have been described: 1, similar to salivary gland type basal cell adenocarcinoma, low grade; 2, similar to salivary gland type basal cell adenocarcinoma, high grade; 3, invasive adenocarcinoma, not otherwise specified; and 4, sarcomatoid (metaplastic) carcinoma.8 Our patient presented a low-grade tumor similar to salivary gland basal cell adenocarcinoma.
Lymph-node and distant metastases reduce survival9; 17.5% of patients develop distant metastases or die from the disease.4
Consensus has not yet been reached on the management of this tumor. The treatment of choice continues to be surgical excision with wide margins of 1 centimeter2,9; this is associated with a 19% likelihood of local recurrence.7 Lymphadenectomy can help to improve the prognosis. Lymphadenectomy was performed in a series of 10 patients with lymph-node metastases10; 6 patients remained disease free. There is no difference in the prognosis of metastatic disease between surgery and surgery plus adjuvant therapy.9
Malignant spiradenoma continues to be a relatively unknown entity, the diagnosis of which can be difficult. Diagnosis is histologic and is based on the observation of areas of spiradenoma associated with malignant changes. The prognosis is known to be poorer if metastases are present at the time of diagnosis, there is a high-grade histologic pattern, or an associated Brooke-Spiegler syndrome. Surgery remains the treatment of choice.
Please cite this article as: Ruiz-González JF, Quiñones-Venegas R, Valdes-Rodriguez R, Solís-Ledezma G. Espiradenoma maligno: un tumor gigante de los anexos cutáneos. Actas Dermosifiliogr. 2016;107:259–260.