The patient was a 35-year-old woman with no past history of interest. She consulted for a skin lesion that had arisen on the abdomen 8 months earlier. The lesion was asymptomatic and had not changed.
Physical ExaminationAn erythematous papule with a whitish halo, measuring 1×0.5cm diameter, was observed on the left side of the abdomen (Fig. 1).
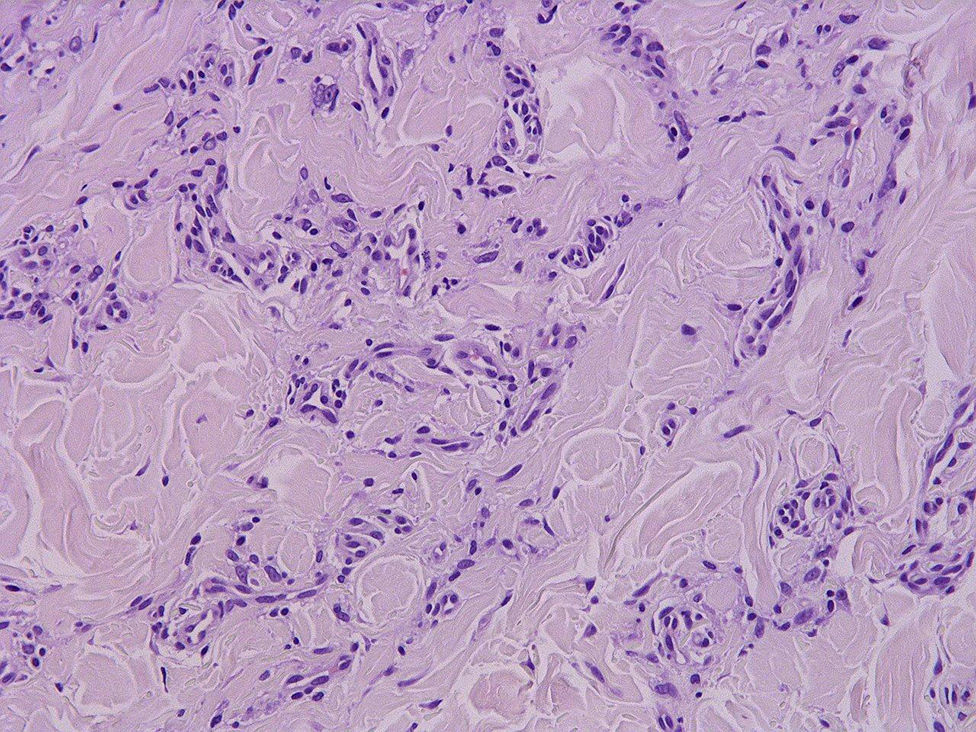
HistopathologyA biopsy of the lesion revealed a proliferation of uniform, small branching vessels in the dermis. The vessels had a collapsed appearance, with a very small lumen and prominent endothelial cells. No cell atypia or mitotic figures were observed. Immunohistochemistry for herpesvirus8 was negative (Fig. 2).
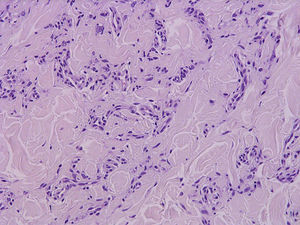
Additional TestsOn dermoscopy the lesion showed diffuse central erythema with desquamation and a delicate peripheral pigment network (Fig. 3).
What Is Your Diagnosis?
DiagnosisMicrovenular hemangioma.
Clinical Course and TreatmentThe excision biopsy performed at the first visit completely removed the lesion. No further treatment was required.
CommentMicrovenular hemangioma is a slow-growing, acquired benign vascular tumor that usually presents as a single erythematous papule, plaque, or nodule on the trunk or limbs of a young adult. The pathogenesis is unknown. The differential diagnosis includes benign (capillary hemangioma, pyogenic granuloma, and angioblastoma) and malignant (angiosarcoma and Kaposi sarcoma) vascular tumors and other lesions that present as erythematous-violaceous nodules, macules, or plaques that can resemble microvenular hemangioma. When multiple lesions are present, the differential diagnosis should include tumors and inflammatory lesions, such as eruptive dermatofibromas and leiomyomas, pityriasis lichenoides et varioliformis acuta, and drug eruption.1
The definitive diagnosis is histological, with the finding of a proliferation of small dermal vessels formed of capillaries and venules, with no atypia.2 Recent studies have described the immunohistochemistry of microvenular hemangioma, which is positive for WT1 (and angiogenesis marker) and negative for D2-40 (a marker of lymphatic differentiation), GLUT-1 (specific to infantile hemangioma), and HHV-8 (positive in Kaposi sarcoma).1,2
Although dermoscopy can reveal certain peculiarities, there are few published descriptions because of the low frequency of the disease. The first description was provided by Scalvenzi et al.,3 who reported diffuse erythema with multiple red globules of variably small size, and the presence of a fine peripheral pigment network. The red globules are defined as round structures, larger than dots.4
Based on the dermoscopic findings, the differential diagnosis should include Kaposi sarcoma, which presents a classic rainbow pattern in its papular and nodular phases.5 However, early lesions can be similar to microvenular hemangioma, with a fine peripheral pigment network and a homogeneous pinkish-red color or a homogeneous structure with reddish-blue areas; globules, characteristic of microvenular hemangioma, have not been reported. In the present case we did not observe globules, further increasing the difficulty of differentiation from Kaposi sarcoma.
The presence of erythema or small vessels, particularly when associated with a multicomponent pattern, increases the possibility of vascular tumors and malignant lesions.
The dermoscopic findings were similar to those of a variant of dermatofibroma, with a peripheral network and a homogeneously erythematous central area. To date there have been no descriptions of cases of microvenular hemangioma that mimic dermatofibroma on dermoscopy.
We have presented a case of microvenular hemangioma, a rare vascular tumor with dermoscopic features that can mimic other tumors and that must be included in the differential diagnosis of vascular tumors and of nonmelanocytic lesions with a pigment network.
Please cite this article as: Fernández-Morano T, Fernández-Canedo I, Fúnez-Liébana R. Pápula eritematosa abdominal. Actas Dermosifiliogr. 2016;107:62–63.