Primary cutaneous follicle center lymphoma (FLC) is defined as a malignant proliferation of germinal center cells confined to the skin. It has 3 growth patterns: follicular, diffuse, and mixed. It usually presents clinically as erythematous papules, plaques, and tumors, generally without ulceration, that most often affect the head, the neck, and the trunk. There is, however, a less common variant known as reticulohistiocytoma of the back or Crosti lymphoma that affects the back and consists of plaques and tumors surrounded by macules and papules that extend outward from the tumor.1
We present a case with histologic findings that posed a diagnostic challenge and clinical features that were consistent with Crosti lymphoma. The patient was a 53-year-old man who consulted for a back lesion that had grown progressively over the previous 6 years. A previous biopsy performed at another center had shown an infiltrate composed of atypical lymphocytes with positivity for T-cell markers and abundant CD30+ cells. The suspected diagnosis was mycosis fungoides with CD30+ cells. No additional immunohistochemical information was available. A staging study consisting of computed tomography (CT) of the chest and abdomen and routine blood tests was normal.
Physical examination revealed several tumors and plaques surrounded by erythematous macules in the lumbar region and on the left flank (Fig. 1). There were no signs of organomegaly or lymph node enlargement.
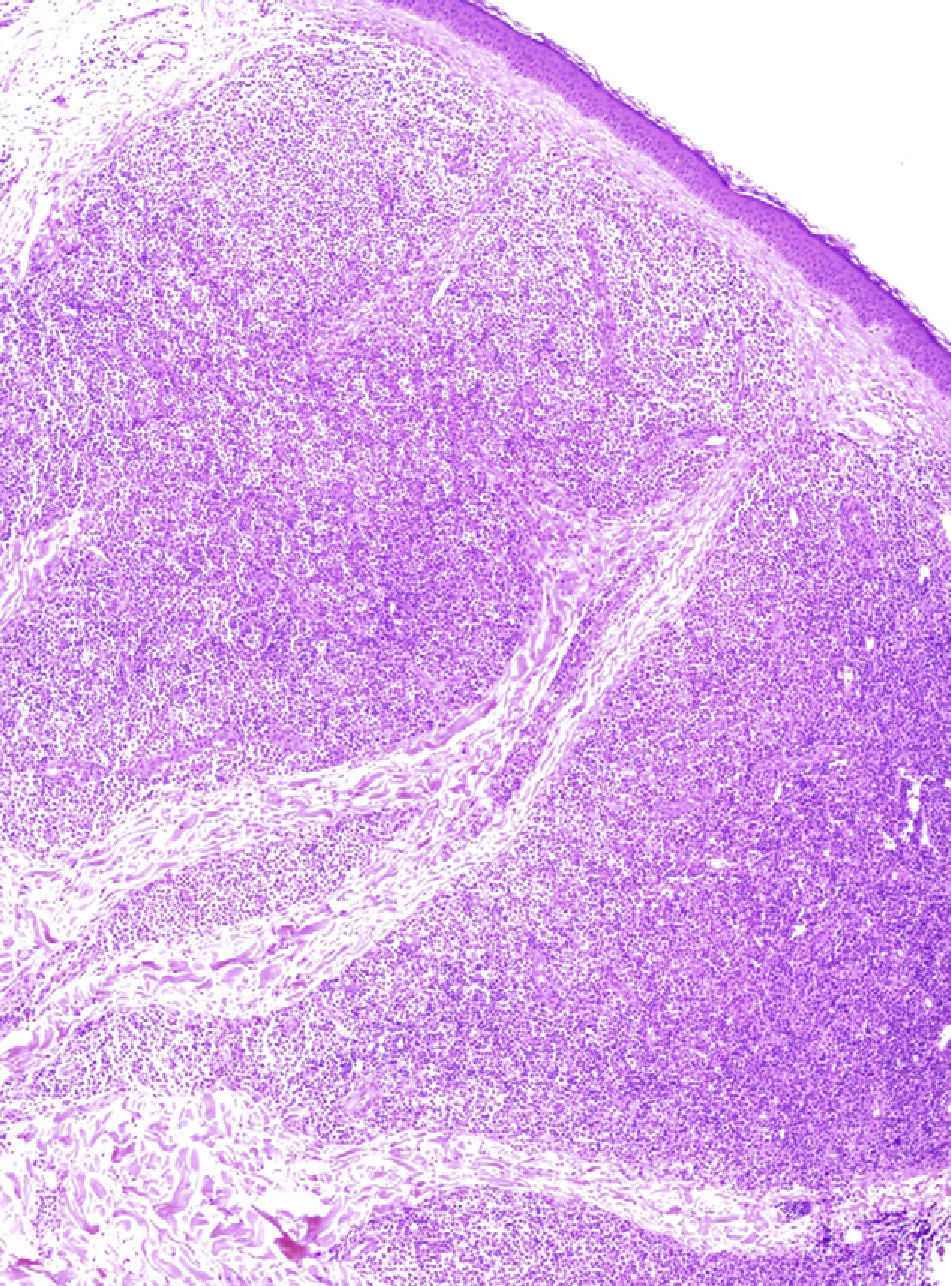
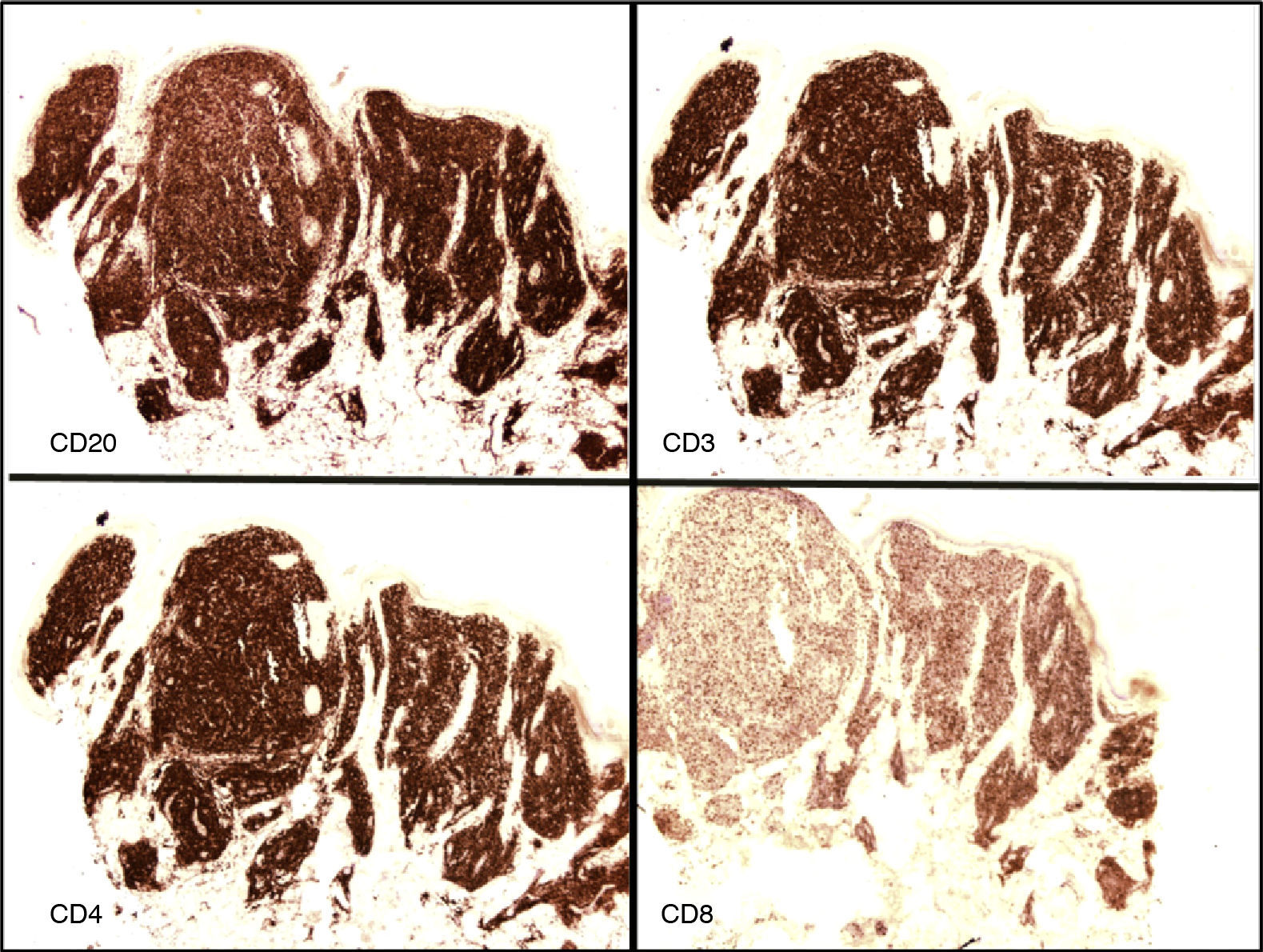
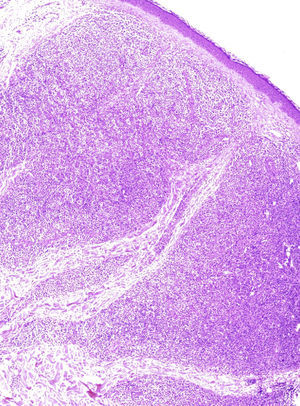
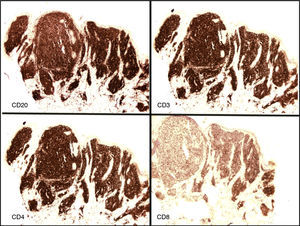
A biopsy performed at our center showed a nodular lymphoid proliferation with a tendency to coalesce extending throughout the dermis and into the hypodermis, with no evidence of epidermotropism (Fig. 2). The lesion was composed of medium and large B cells that were positive for CD20 and CD79 and negative for CD3, CD10, CD23, and CD43; there were also, however, abundant CD3+, CD5+, and CD7+ T cells (Fig. 3). Immunostaining was positive for bcl-6 in the large cells and in some of the smaller cells. There was also bcl-2 positivity, but this was difficult to interpret due to the presence of large number of T cells. The cells were negative for CD30, contrasting with the results from the previous biopsy. Approximately 15% of the cells were positive for Ki67. Immunogenotyping revealed clonal rearrangement of immunoglobulin heavy locus (IHG) genes and a lack of T-cell receptor gene (TCR) rearrangement.
On the basis of these findings, we ordered a staging study consisting of general blood tests (including analysis of lactic acid dehydrogenase and β-2 microglobulin levels), a chest and abdomen CT scan, and a bone marrow biopsy. The results were all normal.
The main entity considered in the differential diagnosis was marginal zone B-cell lymphoma which, unlike cutaneous FCL, tends to be bcl-6-negative. We also considered diffuse large B-cell lymphoma, leg-type, but this is characterized by a diffuse monomorphous infiltrate with large numbers of large bcl-2+ and MUM-1+ cells. Because of the large number of T cells observed, we also initially considered mycosis fungoides and pseudolymphoma, but ruled these out on the basis of the clinical presentation, the type of infiltrate, the presence of IGH clonal rearrangement, and the lack of TCR clonal rearrangement2 (although it should be noted that TCR clonal rearrangement is not always detected in early mycosis fungoides3).
On correlating clinical and pathologic findings, Crosti lymphoma was considered the most likely diagnosis.4 This classic variant of cutaneous FCL is characterized by a B-cell infiltrate with follicle center cells and a variable number of centroblasts that may be accompanied by abundant reactive T cells.2 Pan B-cell markers and germinal center markers tend to be positive, but the latter may be negative in FCL with a diffuse growth pattern.5 Unlike in follicular lymphoma of nodal origin, cells in Crosti lymphoma are normally not immunoreactive for bcl-2.2,6 Up to 15% of primary cutaneous FCLs, however, express bcl-6 (as was the case with our patient), and this aids diagnosis.2
Following the recommendations of the European Organisation for Research and Treatment of Cancer,7 we initiated treatment with local radiation therapy. This led to resolution of the lesions and there were no signs of recurrence after 8 months of follow-up.
We have described a case diagnosed as Crosti lymphoma, which is a classic variant of primary cutaneous FCL generally characterized by a diffuse growth pattern and abundant immunoreactive T cells, although diagnosis can be complicated by an absence of germinal center markers.2,5 In our patient, the main confounding factor was the large T-cell population as this made it difficult to interpret immunohistochemical results and observe tumor cells. The diagnosis was established following a correlation of clinical and pathologic findings.
Please cite this article as: Morell L, Bassas-Vila J, Mate JL, Bielsa I. Linfoma de células B cutáneo: relevancia de la correlación clínico-patológica. Actas D Dermosifiliogr.2012;103:746-748.