We have read with interest the article published recently by Fernández-Canga et al.1 on eyelid ectropion. Review articles, like that one, given their educational intent, bear an important responsibility, as many readers could take up certain diagnostic and treatment habits based on what they read, and this would have an impact on the care of our patients. For this reason, we would like to add some caveats based on our personal experience of more than 15 years dedicated to oculoplastic surgery and above all based on the scientific evidence.
The review deals with a syndrome of eyelid malposition, which apart from its esthetic impact, also has mainly ophthalmologic consequences. Of note in the article was the limited mention of the ocular surface and lacrimal duct. The eyelid and the eye are intimately related, and so any patient with a problem with the eyelid should undergo full ophthalmologic study. Ectropion can be caused by rubbing watery eyes in cases of obstructions in the lacrimal duct, problems with the ocular surface, or inflammatory processes, to mention some possibillities.2–4 To summarize study of ectropion merely with reference to eyelid laxity and its different components, without including full ophthalmologic study, would no doubt leave many patients without an appropriate diagnosis of the cause, resulting in a lower rate of therapeutic success.
Regarding the proposed algorithm for prevention of ectropion, it is important to differentiate between ectropion caused by medial or lateral laxity and/or by retractors when we examine our patients, as treatment, and ultimately prevention, would be different (Fig. 1).5 We will take a closer look at this concept later.
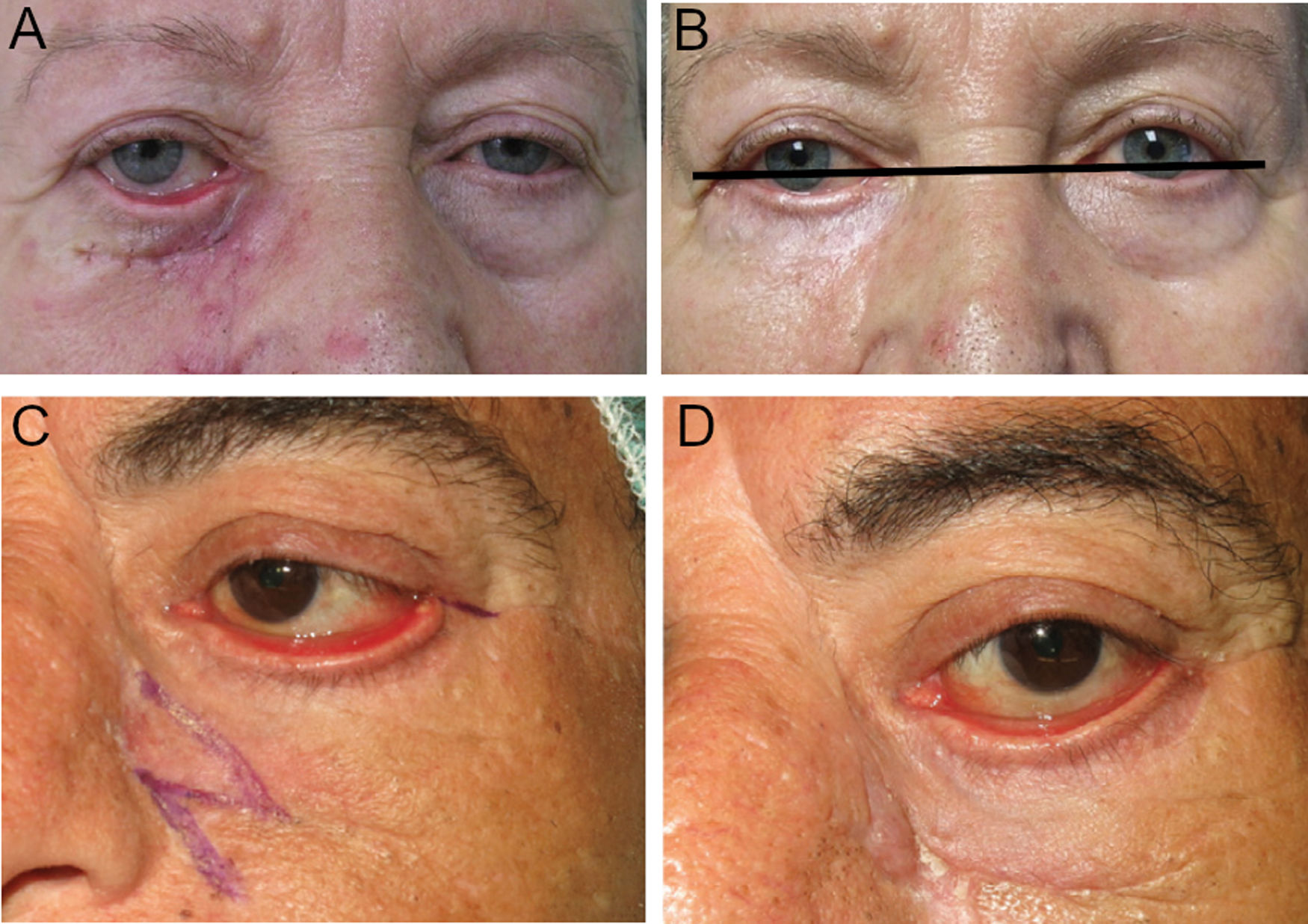
A, Ectropion with medial predominance, caused by scarring of the anterior lamella, probably associated with retractor laxity due to the age of the patient. B, Treatment by canthoplasty only, without involving either the retractors or anterior lamella, leading to an unsatisfactory outcome, with improvement in ectropion but persistence of an evident eyelid retraction. C, Complete tarsal ectropion. The outcome of an isolated Z-plasty is unsatisfactory, as can be observed comparing with the postoperative image (D) in which ectropion persists with evident inflammation of the ocular surface (taken from Fernández-Canga et al.1).
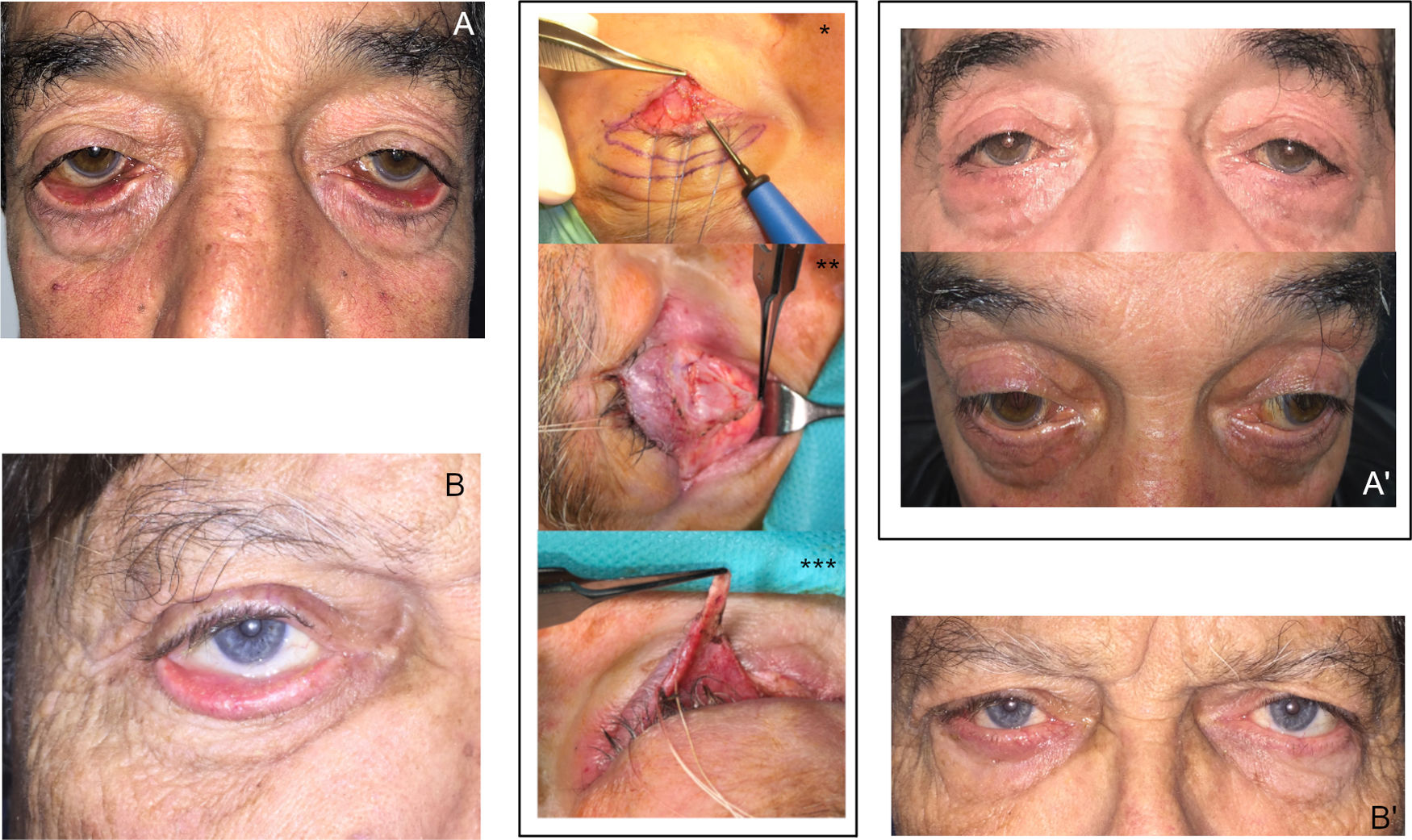
Regarding treatment, most patients have mixed ectropion; one of the main pathophysiological components underlying involutional ectropion is disinsertion of the lower eyelid retractors. From an educational point of view, the approach to ectropion should necessarily mention treatment of retractors; different techniques and approaches are available for these procedures.6–8 Z-plasty does not usually achieve satisfactory outcomes if it is not combined with other techniques in the treatment of cicatricial ectropion (Fig. 1). The use of synthetic materials in the treatment of cicatricial ectropion is not supported by the evidence; the authors cite a study in which acellular dermis is used as an alternative in the reconstruction of the posterior lamella; however, this approach is not appropriate in cases of ectropion in which we require the anterior but not the posterior lamella.9 Finally, as mentioned earlier, in cases of involutional ectropion, in which disinsertion of the retractors plays a key role, we cannot limit the approach to canthopexy or canthoplasty, but should also consider combining these techniques with others that address all pathophysiological causes of the process, particularly surgery of the retractors, and appropriate management of the skin (Fig. 2).
Examples of complete treatment taking into account the underlying pathophysiology. Images of severe inferior ectropion, bilateral (A) and right side (B) with involutional components (laxity of the lateral canthal tendon and disinsertion of retractors) and cicatricial components (shortening of the anterior lamella due to chronic actinic damage). Correct treatment should combine different techniques aimed at correcting the cause of the process; in these cases we performed a heteropalpebral flap in association with anterior lamella (*), retractor surgery (**), and surgery of the lateral canthus (***). A’ and B’, Images at 4 months after surgery of the same patients: correct positioning of the lower eyelids can be observed, without ectropion or residual retraction, with anatomic and functional restitution of the ocular surface.
We found some conceptual errors that should be clarified so as not to confuse readers. Thus, in Fig. 1, the authors1 indicate lower eyelid orbital fat and denote it preaponeurotic fat; in the strict sense, preaponeurotic fat is found in the upper eyelid, which is where we find levator aponeurosis.7 Additionally, the flap that Tripier described in his original article in 1889 consisted of a bipedicled bridge-shaped musculoskeletal flap; after this first description, different modifications have been introduced. A skin or musculocutaneous flap of the upper eyelid to reconstruct defects of the lower eyelid, with lateral or medial base, as mentioned by Fernández-Canga et al.1 is without doubt a very versatile and widely used technique in oculoplastic reconstructive surgery. The flap, depending on its size and design, has recently been shown to behave partially as a graft in novel studies with lasers.10 Strictly speaking, it should not be called a Tripier flap but a modified Tripier flap.
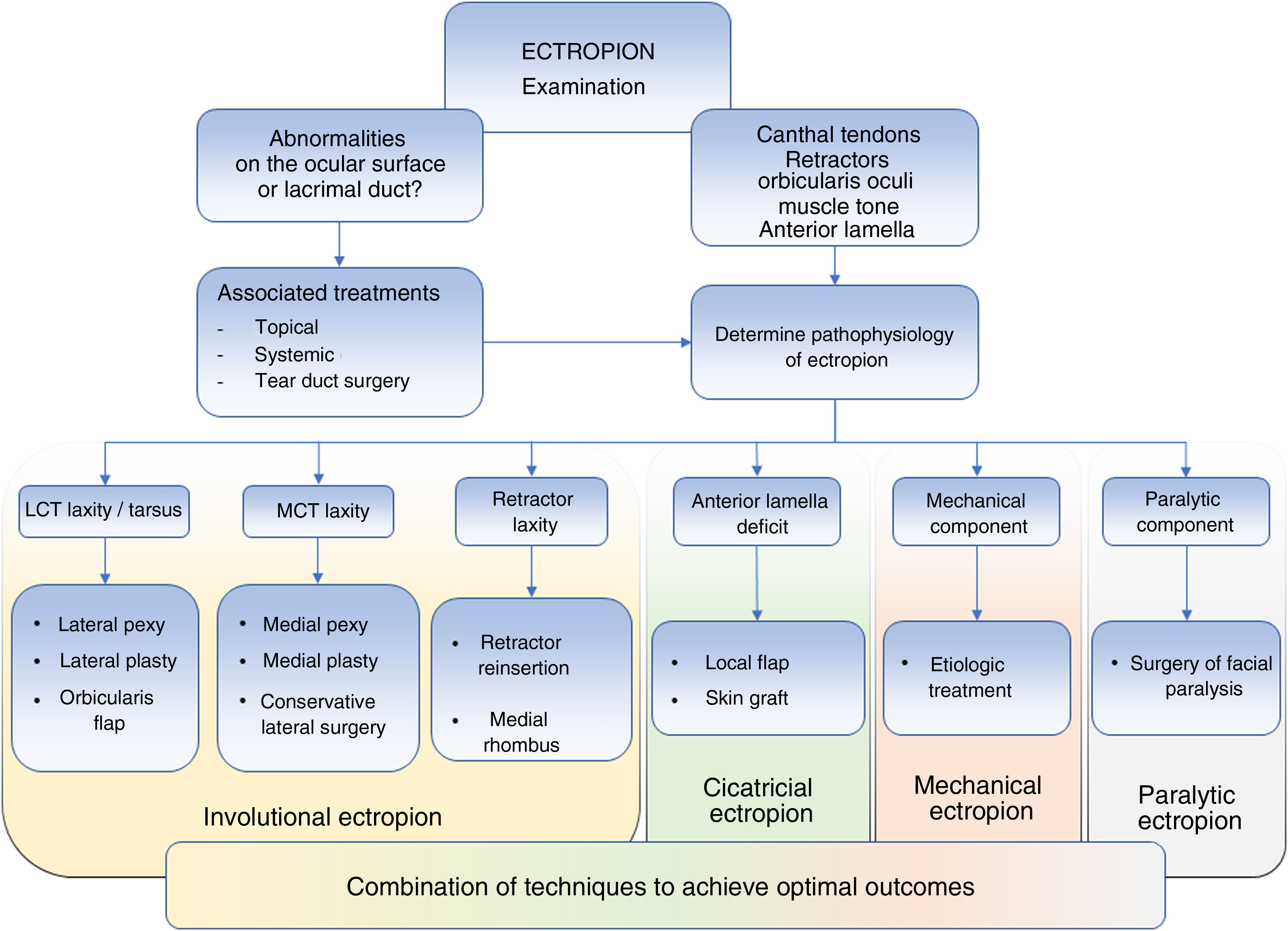
At times, partial improvements in this type of case, as those shown in the study by Fernández-Canga et al.,1 comfort the surgeon to a certain degree in view of the esthetic improvements achieved, but it is important to note that the ocular surface is still exposed and therefore homeostasis may be impacted. This is the difficulty that treatment of ectropion entails (particularly in cases with a cicatricial component). Unless a perfect positioning of the eyelid and the lower part of the conjunctival sacs is achieved, with appropriate contact of the eyelid margin and the lacrimal punctum with the eyeball, the ocular surface will continue to be distressed, with symptoms of epiphora, chronic conjunctivitis, or keratitis. Ultimately, these are the most important aspects requiring improvement. We propose a new algorithm for examination and treatment of ectropion taking into account all the points discussed above (Fig. 3).
Algorithm for examination and treatment of eyelid ectropion. It is important to perform a complete examination to determine which treatment is required; this ensures that the best outcomes are attained and reduces relapses. Abbreviations: LCT, lateral canthal tendon; MCT, medial canthal tendon.
Please cite this article as: Ortiz-Pérez S. Réplica a «Ectropión en cirugía dermatológica: exploración y técnicas reconstructivas». Actas Dermosifiliogr. 2021;112:385–388.