In 1909 the term lupus erythematosus tumidus was coined by Hoffmann,1 and in 1930 Gougerot and Burnier2 described the cases of 5 patients with similar clinical pictures consisting of nonscarring, erythematous, indurated facial lesions without surface changes. This condition, also known as tumid lupus erythematosus (TLE), has been largely overlooked in the literature, but has been recently characterized as a subtype of cutaneous lupus erythematosus (CLE) with peculiar clinical, photobiological, histological, and prognostic features.
A 70-year-old woman with a history of hypertension and Hashimoto thyroiditis was seen for asymptomatic skin lesions on the face that had appeared during the summer 5 months earlier and were not associated with any systemic clinical signs. The appearance of the facial lesions coincided with worsening of pre-existing lesions on the scalp and associated hair loss.
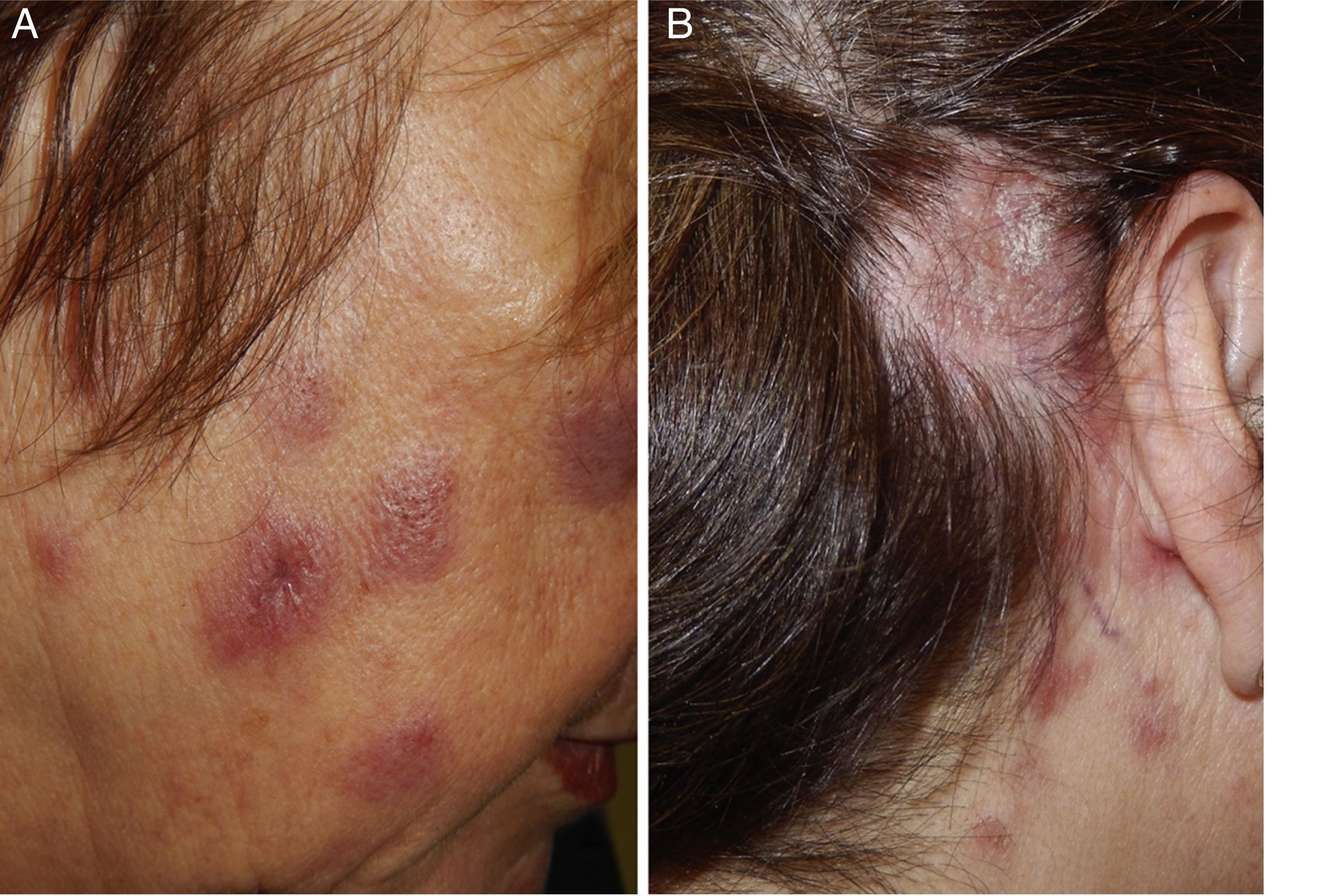
Physical examination revealed the presence of erythematous, edematous, infiltrated, nondesquamative plaques on the face, cervical region, and upper chest (Fig. 1A), as well as erythematous, desquamative, alopecic plaques on the parietal and right retroauricular areas of the scalp (Fig. 1B).
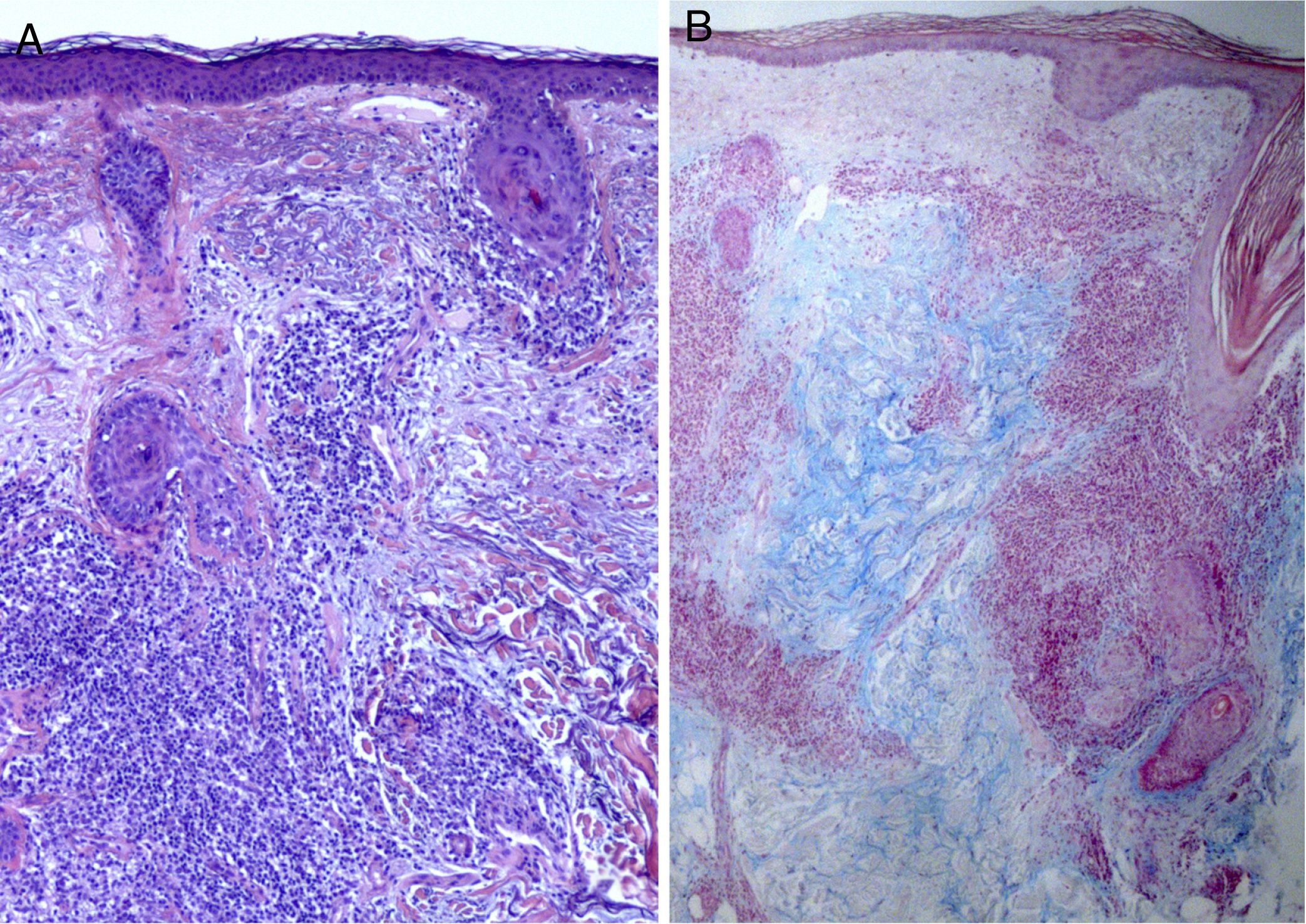
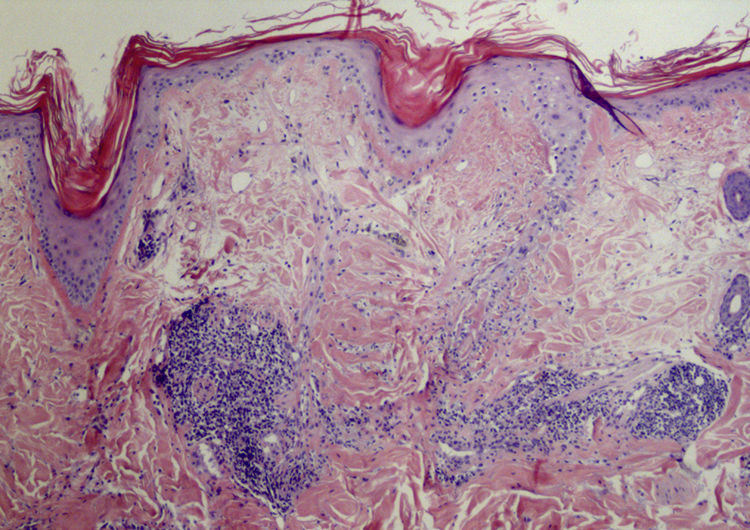
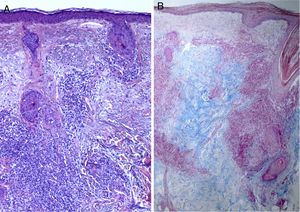
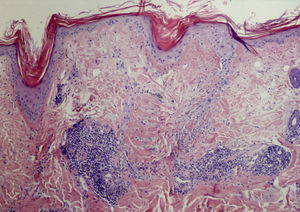
Results of previous laboratory tests performed in another center revealed that the patient was positive for antinuclear antibodies (ANA) (1:320) and negative for anti-Ro and anti-La antibodies. All other parameters were within the normal range. The results of a biopsy were consistent with lymphocytoma cutis. Given the suspicion of a lymphoproliferative process induced in response to CLE, new biopsies and laboratory tests were performed. The results revealed a decrease in ANA levels to 1:80. The pathological report of the facial lesion described discrete epidermal atrophy and a perivascular and periadnexal lymphocytic infiltrate, with no signs of interface dermatitis and abundant mucin deposition in the dermis (Fig. 2). The results of the scalp biopsy were compatible with discoid lupus erythematosus (DLE) (Fig. 3).
Based on these results the patient was diagnosed with CLE with concomitant DLE and TLE. The patient began treatment with photoprotection, 0.05% clobetasol propionate, and hydroxychloroquine at an initial dose of 400 mg/24 h followed by subsequent maintenance therapy at 200 mg/24 h, resulting in progressive clinical improvement.
The mean age of TLE patients is 36.4 to 38.5 years, and women and men appear to be affected equally.3,4 Clinically, TLE is characterized by the appearance in sun-exposed areas of erythematous, succulent, urticariform, nondesquamative plaques that heal without scarring or hypopigmentation. Other characteristic features are a higher frequency of photosensitivity, as determined by phototesting, and a lower percentage positivity for anti-double-stranded DNA (dsDNA), anti-Ro (Sjögren's-syndrome-related antigen A), and anti-La (Sjögren's-syndrome-related antigen B) antibodies than described for other CLE subtypes.3,4 Associated systemic disease in these patients appears to be very rare, albeit possible.4,5 Histology reveals perivascular and periadnexal lymphocytic infiltrate and abundant deposition of interstitial mucin in the dermis. Compared with other CLE subtypes, the epidermis shows only mild alterations (or is intact), and basal vacuolization, hyperkeratosis, epidermal atrophy, and follicular plugging are less marked.6 Treatment with systemic antimalarials is effective in approximately 90% of patients, as compared with 50% of DLE patients.3 In addition to other CLE subtypes, the differential diagnosis should include polymorphic light eruption, Jessner lymphocytic infiltrate, reticular erythematous mucinosis, and pseudolymphoma,3 all of which have clinical and microscopic characteristics that resemble those of TLE. Consensus is lacking regarding several aspects of TLE, including its differential diagnosis, classification, and microscopic characteristics. Because several of its features are distinct from those of other forms of lupus, some authors question the origin of TLE, and consider it a photodermatosis outside the CLE spectrum.7,8 However, we believe that classification of TLE as a true lupus subtype is justified based on the evidence published to date, in particular the coexistence of TLE and DLE lesions in certain patients,3–5,9,10 as in the present case. Our description of a case of coexisting TLE and DLE adds to the small number of such cases reported in the literature, and should help resolve some of the controversy surrounding TLE, facilitating earlier diagnosis of this entity and better management of affected patients.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Abadías-Granado I, Sánchez-Bernal J, Felipo-Berlanga F, Ara-Martín M. Coexistencia de lupus eritematoso túmido y lupus eritematoso discoide. Actas Dermosifiliogr. 2019;110:253–255.