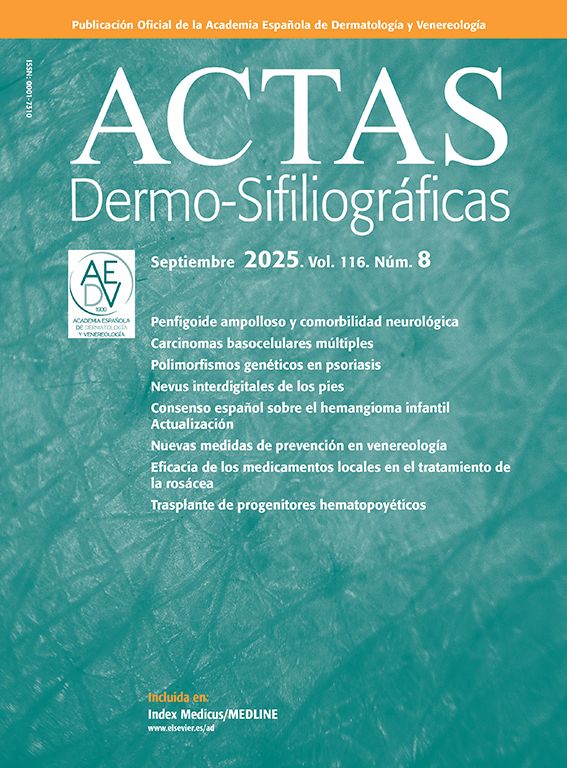
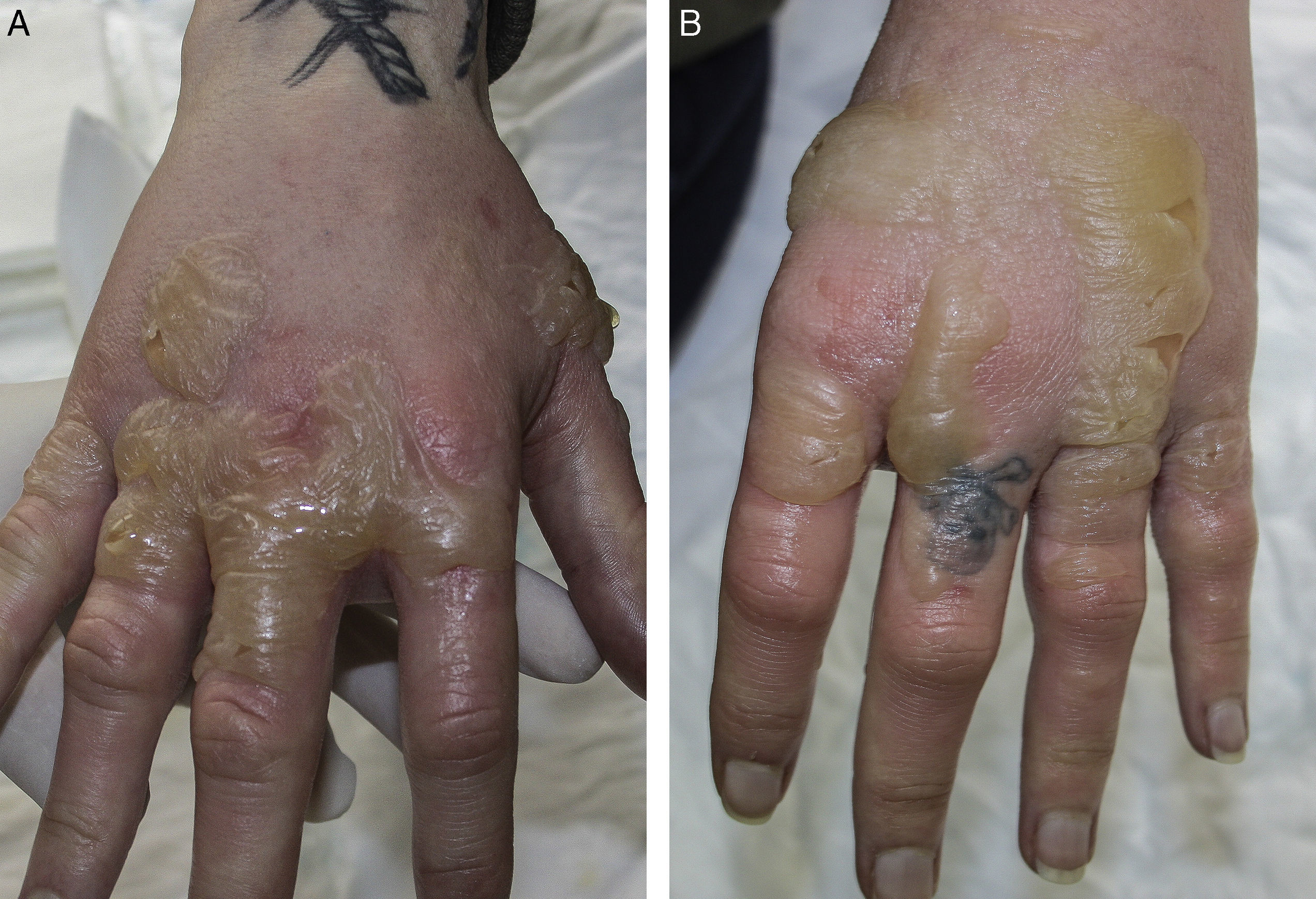
The patient was a 33-year-old woman with a past history of hypothyroidism, anorexia nervosa, and anxiety-depression with episodes of self-harm. She was on treatment with levothyroxine, fluoxetine, clonazepam, and clomethiazole, and there had been no recent changes in her medication. She attended the emergency department for a 3-day history of large, painful blisters on the dorsum of both hands and fingers (Fig. 1). The blisters contained a serous fluid and the surrounding skin was erythematous and pruritic. The patient denied having applied any substance to the area or contact with plants, and at that moment she was off work because of her psychiatric illness and dedicated her time to walking and reading outside, even though it was winter. The lesions were reminiscent of large burns and, suspecting that they may have been self-inflicted, it was decided to admit the patient to observe the clinical course. During her admission, she was prescribed topical therapy with fusidic acid and betamethasone, and oral therapy with prednisone and amoxicillin–clavulanic acid, leading to an improvement in the lesions within a few days. On resolution of the acute bullous condition, we observed very clearly defined, diffuse pigmentation of a residual appearance on the skin distal to the wrists (Fig. 2), but that did not affect the area covered by a ring; this suggested a possible diagnosis of phototoxicity. Additional tests performed, including extensive blood tests with autoimmune studies and 24-hour urinary porphyrin levels, determination of the minimal erythematous dose for UV-A and UV-B, and patch and photopatch testing with the standard series of the Spanish Contact Dermatitis and Skin Allergy Research Group and photoallergens of the Spanish Photobiology Group, were rigorously normal. Histology of the lesions showed a subepidermal blister with epidermal necrosis. Occasional apoptotic keratinocytes were observed in areas adjacent to the blister and a dermal infiltrate of lymphocytes, histiocytes, and eosinophils, with a number of extravasated red blood cells were observed in areas adjacent to the blister; these findings were compatible with a diagnosis of bullous phototoxic dermatitis. On further questioning, the patient finally remembered having applied a product prepared by a faith healer to combat an evil-eye curse 24 to 36hours prior to onset of the lesions. This remedy consisted of an infusion of a plant called rue, which the patient had to apply all over her body except on her head. The site of the lesions coincided with the only area that had not been covered by her winter clothing after applying the substance.
Plants of the genus Ruta are small bushes originating from southern Europe that are cultured as ornamental plants in gardens and also for their medicinal properties and as a condiment. Among their many effects (abortifacient, antiparasitic, insect repellent, analgesic,…), they are widely known for their phototoxic capacity due to the furanocoumarins (5-methoxypsoralen and 8-methoxypsoralen) and alkaloids that they contains.1 Numerous cases have been published of phytophotodermatitis due to the topical application of distinct species of Ruta for various therapeutic uses, such as pediculicide2 or analgesic3 lotions, or direct use of the plant as an insect repellent.4 In most cases, the clinical diagnosis is simple because of the site of the lesions in sun-exposed areas, the tendency to form vesicles or blisters, and the residual pigmentation, together with a history of contact with the plant or the application of substances that the plant contains.
Blister formation in the phytophotodermatoses can be intense, simulating extensive burns.5 In children, contact with phototoxic plants can be accidental, when playing in gardens, and is often not remembered.6 The appearance of lesions similar to burns with no history of contact with plants can confound the diagnosis.
Apart from its therapeutic applications, Ruta is used widely in some countries of the Iberian peninsula and Latin America to protect against “evil spirits”.7,8 The recommendation to apply products containing this plant all over the body, typically followed by exposure to the sun, perhaps even on the beach, gives rise to widespread lesions that only spare the areas covered by the bathing suit. Severe episodes of extensive phytophotodermatitis require a multidisciplinary approach with supportive measures in burns units.
We have presented a case of bullous phytophotodermatitis due to the use of Ruta in an unusual esoteric remedy against an evil-eye curse. A diagnosis of phytophotodermatitis must be suspected in patients with bullous lesions only affecting sun-exposed skin. On resolution, the lesions tend to produce well-defined residual pigmentation. It is also important to consider this diagnosis in children, in whom contact with the plant may be accidental and pass unnoticed.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Córdoba S, González M, Martínez-Morán C, Borbujo JM. Fitofotodermatitis ampollosa producida por un remedio esotérico. Actas Dermosifiliogr. 2017;108:79–81.