Becker nevus (BN) is a hamartoma lesion characterized by a hyperpigmented macule with irregular, though well defined, borders, with hypertrichosis on the surface. It tends to present peripheral satellite lesions and is most frequently located on the anterior surface of the chest and on the shoulder girdle.1–3
Although it generally involves only the skin, it may occasionally be associated with muscle and bone abnormalities, constituting Becker nevus syndrome (BNS). This syndrome was defined by Happle and Koopman4–6 20 years ago and few cases have since been published in the literature.
Case SeriesCase 1A 12-year-old boy with no past personal or family history of interest presented a mildly hyperpigmented macule on the left side of the face and neck, and left arm. The lesion had been present since birth. Physical examination revealed a hyperpigmented macule with well-defined borders, with islands of healthy skin on the periphery and mild hypertrichosis with respect to the rest of the skin; the lesion involved the left cheek, neck, and left arm. The clinical picture was interpreted as BNS. The patient also presented hypoplasia of some teeth homolateral to the nevus, and facial asymmetry and scoliosis.
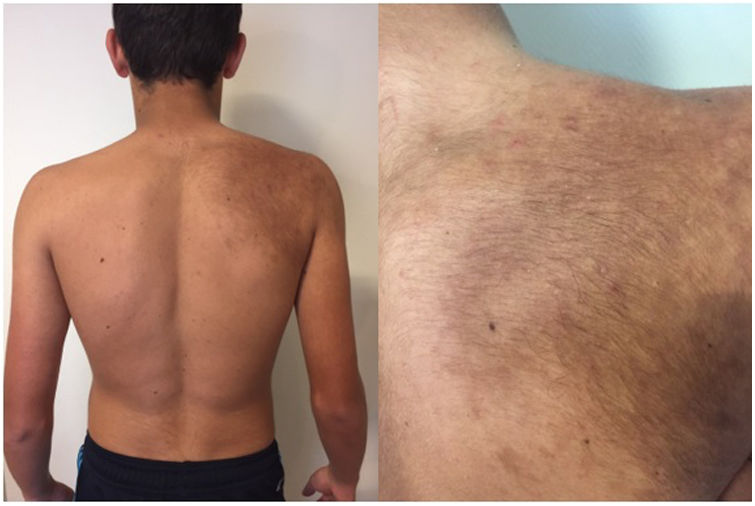
Case 2An 18-year-old boy with a past history of severe scoliosis that had been treated surgically visited our department with a hyperpigmented macule on the left scapular region; the lesion had been present since birth (Fig. 1). The patient reported that the lesion had become more pigmented and hairier over time.
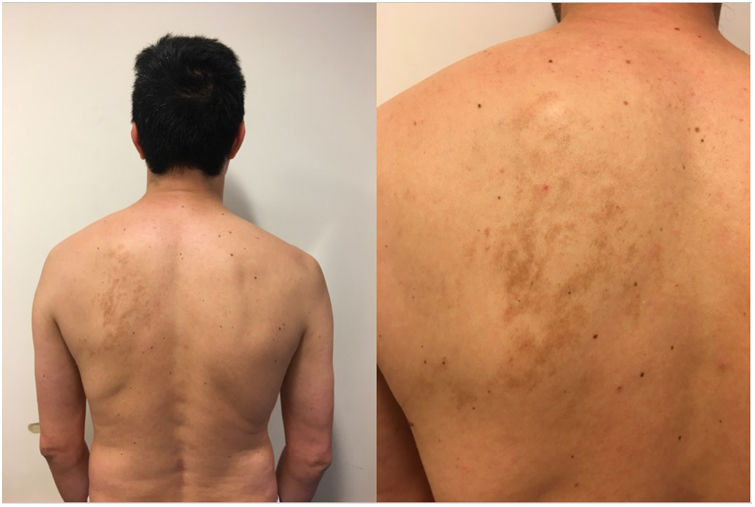
Case 3A 15-year-old boy visited our department with a hyperpigmented macule that involved the area of the right shoulder and scapula; the lesion had been present since birth. The nevus showed a higher density of closed comedones and moderate hypertrichosis compared with the resto of the skin (Fig. 2). The patient also presented moderate scoliosis, leading to a diagnosis of BNS.
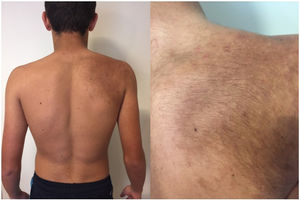
Case 4A 44-year-old man visited our department with a large hyperpigmented macule on the left scapular region; the lesion was the result of the coalescing of smaller macules (Fig. 3). Clear asymmetry in the trophism of the underlying soft tissue was also observed. A chest x-ray revealed marked scoliosis and the clinical picture was interpreted as BNS.
CommentBN was first described by SW Becker in 1949. It is an androgen-sensitive hamartoma. It usually presents from birth, although it occasionally only becomes visible over time, typically at puberty, when it may become more pigmented and hairier, due to hormone stimulation.1 This change is more evident in males. In their series of 118 cases, Patrizi et al7 also found a certain link between evidence of BN and exposure to sunlight.
BNS is the association of BN with underlying musculoskeletal malformations. It is a rare entity that affects both sexes equally, although this varies in different studies.5 Because BN is more frequently found on the thoracic region, especially the pectoral and scapular regions, it is associated with different abnormalities in this location, including as scoliosis, mammary hypoplasia, and muscular hypotrophy. In general, these disorders are ipsilateral to the nevus.6–10 The entity should be distinguished from Poland syndrome, which is characterized by hypoplasia or unilateral absence of pectoral muscles, ribs, breast, or nipple, together with homolateral syndactyly. It is occasionally associated with compromised internal organs.11,12
The clinical spectrum of involvement ranges from subtle manifestations that are difficult to detect clinically, to clear abnormalities, which are generally the reason for a medical consultation. In this regard, women consult more frequently when the BNS involves the breast, due to the resulting asymmetry in the anterior thorax.6,10
BNS forms part of what are known as epidermal nevus syndromes, together with Schimmelpenning syndrome, nevus comedonicus syndrome, Proteus syndrome, and CHILD syndrome. These syndromes are caused by a hamartomatous proliferation derived from the embryonic ectoderm as the result of anomalous growth of different epidermal structures, depending on the case in question.1
They tend to occur due to sporadic mutations. Heterozygotic individuals are phenotypically normal but may transmit the mutation over several generations, whereas the disease manifests in the presence of 2 somatic mutations during embryogenesis, with a paradominant inheritance pattern.1,6 Its genetic basis is not fully understood, although it is thought to be caused by a lethal postzygotic mutation of an autosomal gene that survives in mosaic form.8 Indeed, this entity manifests with characteristics of mosaic phenotype, presenting as a solitary lesion with serrated edges or, less commonly, as a segmented or flag-like lesion. Thus, in members of the same family, it is possible to find individuals with BNS and others with only BN.9
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Tirelli LL, Label A, Luna PC, Larralde M. Síndrome del nevo de Becker. Cuatro casos de una rara entidad. Actas Dermosifiliogr. 2021;112:282–283.