Patients with cutaneous T-cell lymphoma frequently develop intense pruritus, which can often be refractory to anticancer and symptomatic treatments and can affect quality of life to a significant degree.1 Aprepitant, an antiemetic that is a substance P antagonist, has been used successfully to manage refractory pruritus.2,3
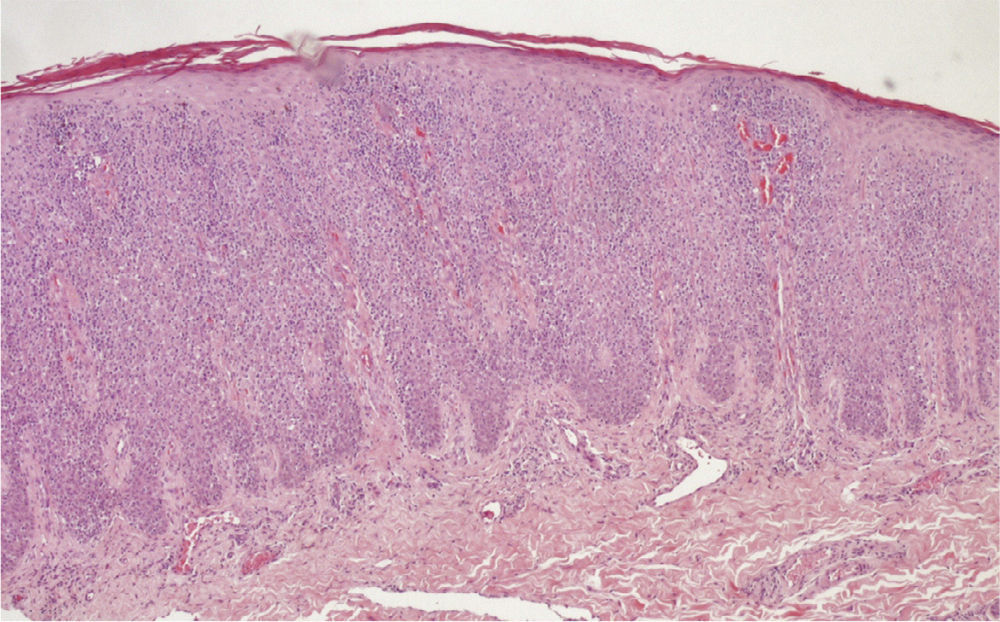
We present the case of a 61-year-old woman who was a smoker with a history of chronic obstructive pulmonary disease and who required home oxygen. In August 2011 she was seen for a 5-month history of skin lesions that she described as very itchy. The lesions, which were present on the head, trunk, and limbs, consisted of plaques and nodules with areas of necrosis (Fig. 1). Biopsy revealed acanthosis and partial necrosis of the epidermis, which was infiltrated by lymphocytes with an atypical morphology and marked epidermotropism (Fig. 2). Immunohistochemistry was positive for CD3, CD7, CD8, TIA1, and Ki67 (50%) and negative for CD4, CD5, CD56, T-cell receptor β-F1, CD79a, and CD20, and Epstein-Barr virus RNA was not detected. Serology for Human T-Lymphotrophic Virus I/II and Borrelia burgdorferi was negative. The study of tumor spread was negative. Based on the above data, a diagnosis of aggressive primary cutaneous cytotoxic T-cell lymphoma was made. The patient received treatment with various chemotherapy protocols—cyclophosphamide, adriamycin, vincristine, and prednisone (CHOP); bexarotene; gemcitabine plus oxaliplati; alemtuzumab; and cyclophosphamide, unpegylated liposomal adriamycin, vincristine, and prednisone (COMP)—without achieving control of disease progression or of the associated pruritus. She was administered symptomatic treatment for the pruritus with 0.1% triamcinolone acetonide cream once a day plus cetirizine 10mg in the morning and dexchlorpheniramine 2mg at night, with no improvement. This treatment was subsequently changed to 0.05% clobetasol cream once a day, plus bilastine 20mg in the morning and dexchlorpheniramine 4mg at night. Due to persistence of the pruritus (score of 10/10 on a verbal numerical scale), it was decided to prescribe aprepitant for off-label use. After using aprepitant for 3 consecutive days (125mg on the first day and 80mg on the second and third days)—there was a marked symptomatic improvement at each 2-weekly evaluation (score of 3/10 on the verbal numerical scale), and this led to a considerable improvement in the patient's quality of life until her death 13 months after diagnosis of the lymphoma.
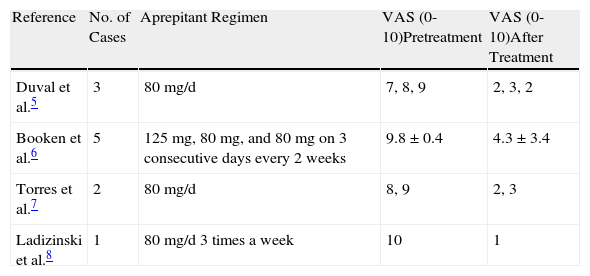
Substance P is a potent inducer of pruritus. It activates the neurokinin-1 receptors present on keratinocytes and mast cells and also on the neurons of the sensory dorsal root ganglion. Aprepitant inhibits the effect of substance P by blocking the neurokinin receptors.1,3 It acts by blocking signal conduction along peripheral nerve C fibers—inhibiting the release of nerve growth factor from keratinocytes—or by blocking signal transmission in the dorsal horn.4 In 2009, Duval et al.5 reported 3 patients with pruritus secondary to Sézary syndrome in whom aprepitant was used at a dose of 80mg/d continuously and led to successful control of the pruritus. Subsequently, Booken et al.6 published the cases of 5 patients with pruritus secondary to erythrodermic cutaneous T-cell lymphoma who were treated with aprepitant on a 3-day regimen (125mg on day 1 and 80mg on days 2 and3) every 2 weeks, with improvement of the pruritus in 4 cases. Later, Torres et al.7 described 2 patients with pruritus secondary to Sézary syndrome; both responded well to aprepitant at a dose of 80mg/d. Most recently, Ladizinski et al.8 were the first to report the efficacy of aprepitant in a patient with nonerythrodermic cutaneous T-cell lymphoma; they administered the drug at a dose of 80mg 3 times a week (Table 1). Aprepitant has also been effective in the control of chronic itching in patients with atopic dermatitis or nodular pruritus,2 in patients with solid tumors,9 and in those with erlotinib-induced pruritus.10 Aprepitant has a good pharmacological safety profile. It is important to remember that this drug is able to inhibit CYP3A4, and it must not therefore be administered to patients on treatment with pimozide, terfenadine, astemizole, or cisapride. It can also induce elevations of the aminotransferases and must be used with caution in patients with altered liver function. The common side effects of aprepitant include hiccup, fatigue, constipation, headache, and anorexia.
Published Cases of the Use of Aprepitant to Treat Pruritus Secondary to Cutaneous Lymphoma.
| Reference | No. of Cases | Aprepitant Regimen | VAS (0-10)Pretreatment | VAS (0-10)After Treatment |
| Duval et al.5 | 3 | 80mg/d | 7, 8, 9 | 2, 3, 2 |
| Booken et al.6 | 5 | 125mg, 80mg, and 80mg on 3 consecutive days every 2 weeks | 9.8±0.4 | 4.3±3.4 |
| Torres et al.7 | 2 | 80mg/d | 8, 9 | 2, 3 |
| Ladizinski et al.8 | 1 | 80mg/d 3 times a week | 10 | 1 |
Abbreviation: VAS, visual analogue scale.
In summary, we have presented the case of a patient in whom aprepitant was used successfully to treat refractory pruritus secondary to cutaneous T-cell lymphoma. This treatment produced a marked improvement in patient's quality of life.
Please cite this article as: Borja-Consigliere HA, López-Pestaña A, Vidal-Manceñido MJ, Tuneu-Valls A. Tratamiento con aprepitant del prurito refractario secundario a linfoma cutáneo de células T. Actas Dermosifiliogr. 2014;105:716–718.