We present the case of a 37-year-old man with no personal history of interest who came to our department with a lesion on the dorsum of the distal phalanx of the third finger of his right hand. The lesion had first appeared after an injury a few months earlier. It had deformed the nail and was painful on palpation.
Physical examination revealed a solid subungual tumor that deformed the nail in such a way that the curvature was increased both longitudinally and transversally (Fig. 1).
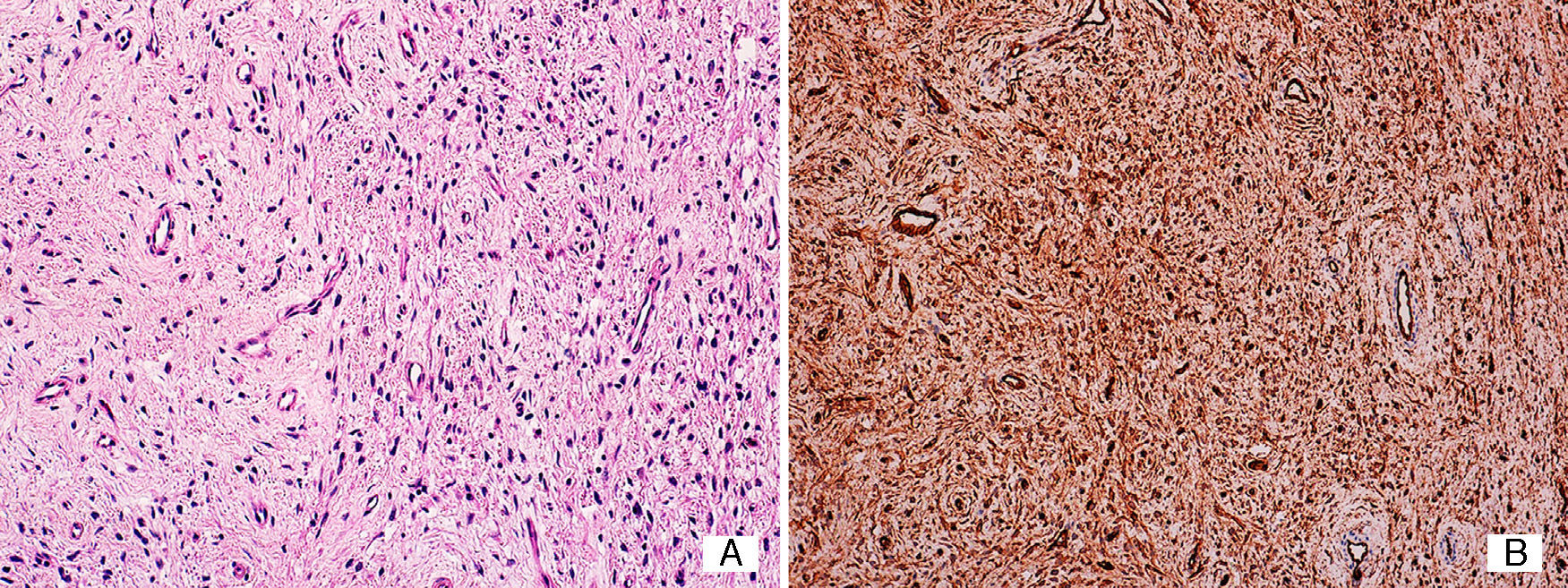
A punch biopsy of the lesion was performed after avulsion of the nail plate. Staining with hematoxylin-eosin revealed a well-defined nodular tumor in the dermis that spared the Grenz zone. Greater magnification revealed that the tumor was composed of a very dense population of spindle-shaped cells that were stellate in appearance with an eosinophilic cytoplasm and surrounded by a myxoid stroma with abundant vessels and isolated mastocytes. The vessels were small and had fine walls lined by endothelial cells with no atypia. Immunohistochemical staining for CD34, S100, and epithelial membrane antigen was only positive for CD34 (Fig. 2). The correlation between clinical and histology findings confirmed the diagnosis of superficial acral fibromyxoma.
A plain radiograph taken before surgery revealed a nodule attached to the soft tissue, with no bone involvement (Fig. 3).
Once the diagnosis was confirmed, the lesion was removed completely. First, the area was anesthetized using digital block with mepivacaine. Second, after application of local ischemia at the base of the finger, a small transverse incision was made in the eponychium in order to better visualize the extent of the lesion. Third, the lesion was dissected carefully and removed. Finally, curettage was performed on the nail bed and the eponychium was sutured. The patient continues to be followed in our department. No recurrence of the tumor has been observed, and the cosmetic outcome is good.
Superficial acral fibromyxoma is a benign tumor that was first described by Fetsch et al. in 2001.1 It is more common on the fingers and toes of middle-aged men. Clinically, it presents as a solid, well-defined, solitary nodule. The nail is involved in as many as 50% of cases.2–4 Diagnosis is usually delayed because of the slow growth of this type of lesion.
Histopathology reveals a well-defined, nonencapsulated tumor affecting the dermis and, sometimes, the subcutaneous cellular tissue. In most lesions, a Grenz zone is visible with no involvement of the epidermis. The tumor is composed of spindle-shaped cell bundles with pale eosinophilic cytoplasm and basophilic nuclei. These cells are immersed in areas of dense hyaline collagen and other areas of myxoid stroma. In most cases, we can see mastocytes and small vessels. Cellular necrosis and lymphovascular invasion are not usually present.1–8 Immunohistochemical staining is positive for CD34, CD99, and epithelial membrane antigen and negative for S-100, muscle-specific actin, and glial fibrillary acidic protein.2–7
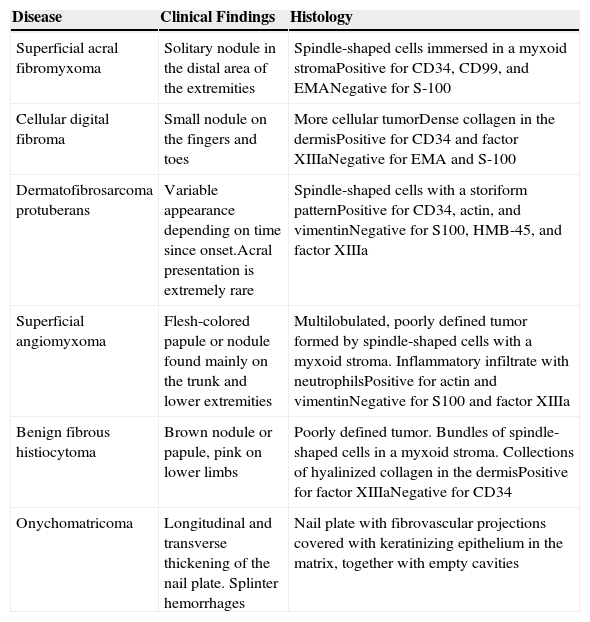
Histologically, it is important to differentiate this tumor from cellular digital fibroma, a CD34-positive tumor composed of spindle-shaped cells with a less myxoid stroma than in acral fibromyxoma that does not show immunoreactivity for epithelial membrane antigen or CD99. The differential diagnosis also includes myxoid neurofibroma, superficial angiomyxoma, fibrous histiocytoma, dermatofibrosarcoma protuberans, and onychomatricoma, owing to the histological characteristics shared by these tumors (Table 1).
Differential Diagnosis of Superficial Acral Fibromyxoma.
| Disease | Clinical Findings | Histology |
|---|---|---|
| Superficial acral fibromyxoma | Solitary nodule in the distal area of the extremities | Spindle-shaped cells immersed in a myxoid stromaPositive for CD34, CD99, and EMANegative for S-100 |
| Cellular digital fibroma | Small nodule on the fingers and toes | More cellular tumorDense collagen in the dermisPositive for CD34 and factor XIIIaNegative for EMA and S-100 |
| Dermatofibrosarcoma protuberans | Variable appearance depending on time since onset.Acral presentation is extremely rare | Spindle-shaped cells with a storiform patternPositive for CD34, actin, and vimentinNegative for S100, HMB-45, and factor XIIIa |
| Superficial angiomyxoma | Flesh-colored papule or nodule found mainly on the trunk and lower extremities | Multilobulated, poorly defined tumor formed by spindle-shaped cells with a myxoid stroma. Inflammatory infiltrate with neutrophilsPositive for actin and vimentinNegative for S100 and factor XIIIa |
| Benign fibrous histiocytoma | Brown nodule or papule, pink on lower limbs | Poorly defined tumor. Bundles of spindle-shaped cells in a myxoid stroma. Collections of hyalinized collagen in the dermisPositive for factor XIIIaNegative for CD34 |
| Onychomatricoma | Longitudinal and transverse thickening of the nail plate. Splinter hemorrhages | Nail plate with fibrovascular projections covered with keratinizing epithelium in the matrix, together with empty cavities |
Abbreviation: EMA, epithelial membrane antigen; HMB, human melanoma black.
Treatment is based on surgical removal, although the tumor can recur in as many as 20% of cases if the excision is not complete.2
Please cite this article as: Martínez-Leboráns L, Martínez-Aparicio A, Alegre de Miguel V. Lesión nodular acral tras traumatismo. Actas Dermosifiliogr. 2015;106:841–843.