Kidney transplant is the treatment of choice for end-stage renal disease.1 Over the years, the number of transplants has grown to reach 3423 procedures performed in Spain in 2019.2 Due to the increased life expectancy, patients are exposed to chronic immunosuppression for more years, which triggers several different diseases, such as non-melanoma skin cancer (NMSC), which appears 15–20 years earlier compared to the overall population.3 While, in this patient population, skin cancer has been extensively studied, little is known about the other skin diseases these patients tend to develop. Some of the dermatoses most widely described in this group of patients include opportunistic infections, or immunosuppressive drug-related adverse events, such as stretch marks, acneiform reactions, or hirsutism.4
The main objective of this study was to describe the skin lesions developed by kidney transplant recipients that triggered medical consultations. This was a retrospective study of skin lesions conducted until August 2019 of all living kidney transplant recipients prior to December 31, 2017 in a tertiary referral center of the Canary Islands, Spain. Data were obtained from dermatology health records. The study was approved by Hospitalario Universitario de Canarias Research Ethics Committee, Tenerife, Spain.
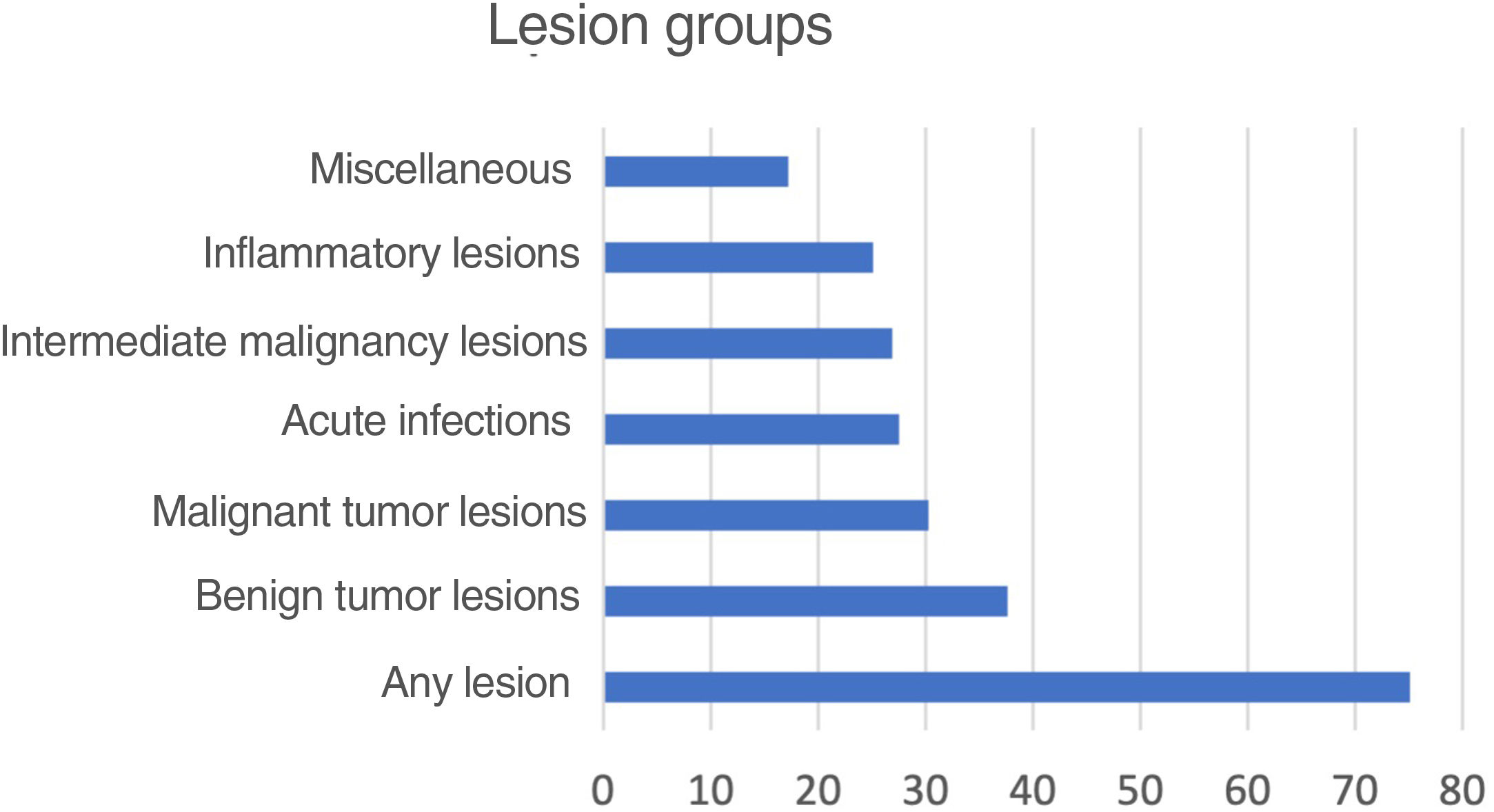
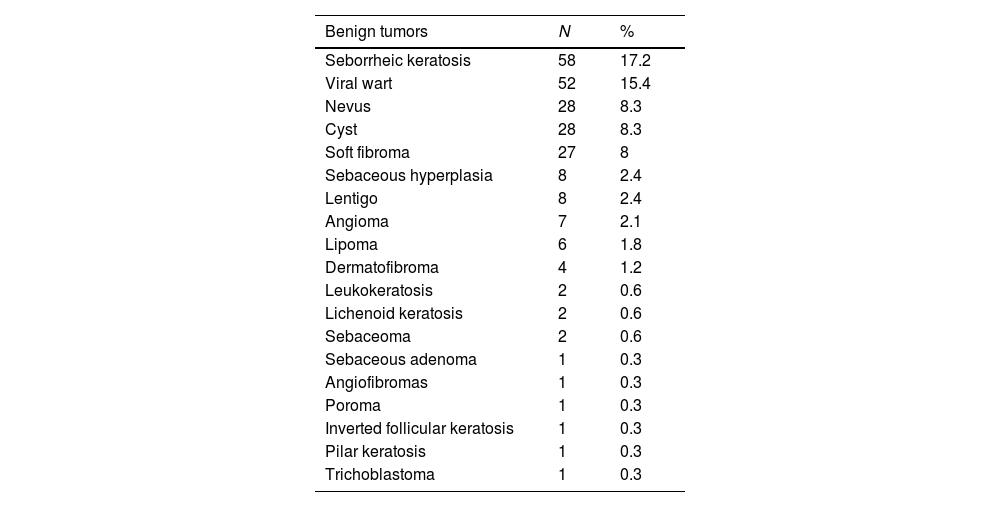
A total of 338 patients treated with kidney transplant from 1983 through 2017 were included in the study with a follow-up period of up to 36 years. A total of 254 patients (75.1%) developed some type of skin lesion. Benign tumors (37.6%) were the most common of all. When lesions were analyzed individually, actinic keratosis (28.7%) turned out to be the most common of all (Fig. 1).
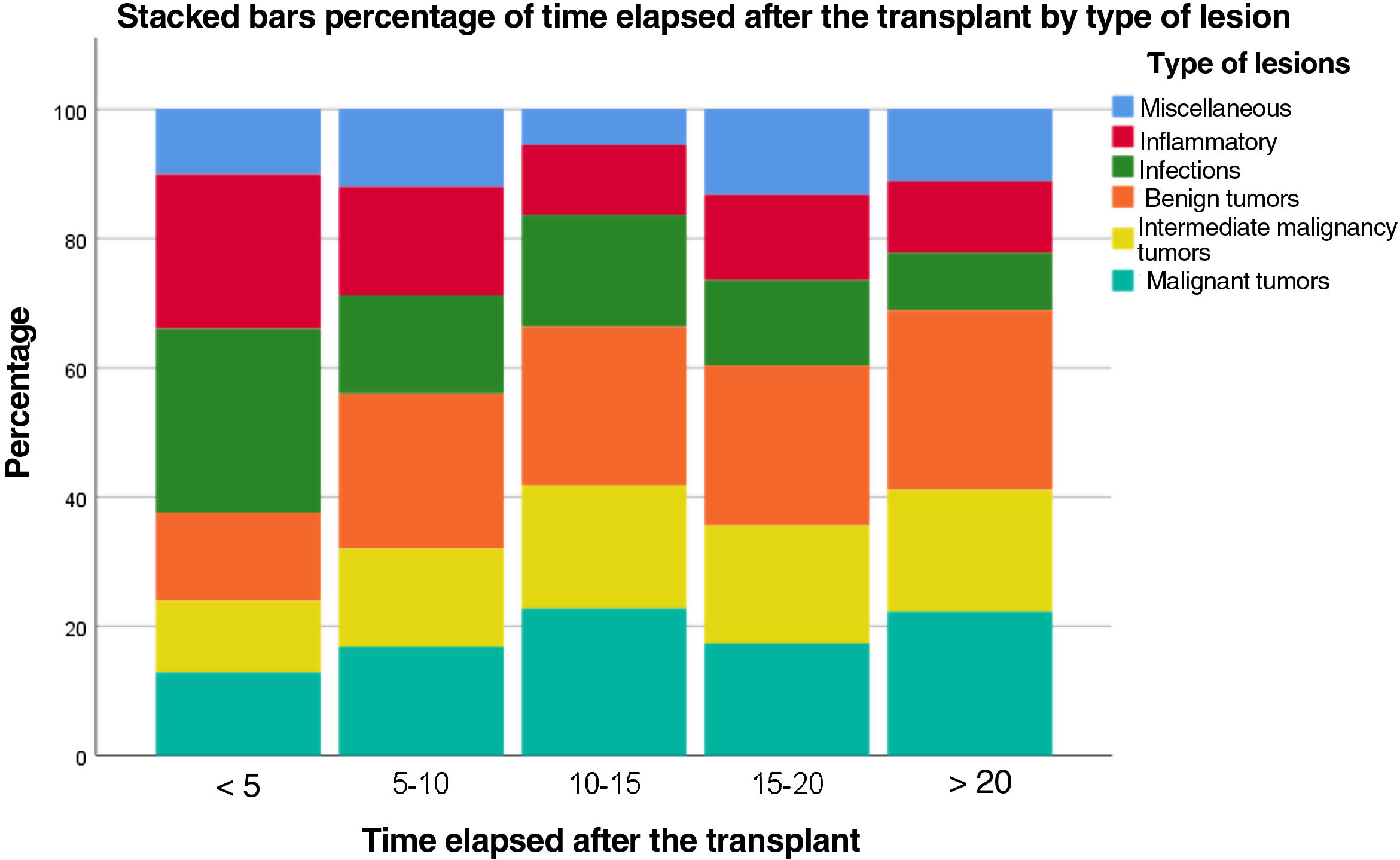
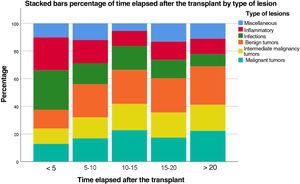
Within the first 5 years, acute infections and inflammatory lesions were the predominant ones, while benign and malignant tumors were more common after more than 20 years (Fig. 2).
The rate of transplant recipients who developed skin cancer was 30.2%, 28.7% of whom developed NMSC, including basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and intraepidermal carcinoma. The most common skin cancer in our kidney transplant recipients was BCC (21.9%) (Table 1). The mean time of appearance of any type of skin cancer was 7.6 years (range, 1–23 years). The SCC/BCC ratio for all patients was 0.69:1.
Skin lesions detailed by benign tumors.
| Benign tumors | N | % |
|---|---|---|
| Seborrheic keratosis | 58 | 17.2 |
| Viral wart | 52 | 15.4 |
| Nevus | 28 | 8.3 |
| Cyst | 28 | 8.3 |
| Soft fibroma | 27 | 8 |
| Sebaceous hyperplasia | 8 | 2.4 |
| Lentigo | 8 | 2.4 |
| Angioma | 7 | 2.1 |
| Lipoma | 6 | 1.8 |
| Dermatofibroma | 4 | 1.2 |
| Leukokeratosis | 2 | 0.6 |
| Lichenoid keratosis | 2 | 0.6 |
| Sebaceoma | 2 | 0.6 |
| Sebaceous adenoma | 1 | 0.3 |
| Angiofibromas | 1 | 0.3 |
| Poroma | 1 | 0.3 |
| Inverted follicular keratosis | 1 | 0.3 |
| Pilar keratosis | 1 | 0.3 |
| Trichoblastoma | 1 | 0.3 |
| Malignant tumor lesions | N | % |
|---|---|---|
| Skin cancer (all) | 102 | 30.2 |
| Basal cell carcinoma+squamous cell carcinoma (including intraepidermal carcinoma) | 97 | 28.7 |
| Basal cell carcinoma+squamous cell carcinoma | 89 | 26.3 |
| Basal cell carcinoma | 74 | 21.9 |
| Squamous cell carcinoma (including intraepidermal carcinoma) | 51 | 15.1 |
| Squamous cell carcinoma | 33 | 9.8 |
| Intraepidermal carcinoma | 32 | 9.5 |
| Keratoacanthoma | 5 | 1.5 |
| Porocarcinoma | 3 | 0.9 |
| Angiosarcoma | 1 | 0.3 |
| Trichilemmal carcinoma | 1 | 0.3 |
| Sebaceous carcinoma | 1 | 0.3 |
| Carcinosarcoma | 1 | 0.3 |
| Cutaneous lymphoma | 1 | 0.3 |
| Melanoma | 1 | 0.3 |
| Bowenoid papulosis | 1 | 0.3 |
| Kaposi's sarcoma | 1 | 0.3 |
| Sweat gland carcinoma | 1 | 0.3 |
| Merkel cell carcinoma | 0 | 0 |
| Verrucous carcinoma | 0 | 0 |
| Acute infections | N | % |
|---|---|---|
| Mycosis | 38 | 11.2 |
| Herpes zoster | 28 | 8.3 |
| Erysipelas/cellulitis | 11 | 3.3 |
| Abscess | 9 | 2.7 |
| Folliculitis | 9 | 2.7 |
| Herpes simplex | 6 | 1.8 |
| Furunculosis | 5 | 1.5 |
| Scabies | 2 | 0.6 |
| Chickenpox | 2 | 0.6 |
| Black hairy tongue | 1 | 0.3 |
| Molluscum | 1 | 0.3 |
| Pediculosis | 1 | 0.3 |
| Intermediate or premalignant tumor lesions | N | % |
|---|---|---|
| Actinic keratosis | 97 | 28.7 |
| Leukoplakia | 1 | 0.3 |
| Inflammatory lesions | N | % |
|---|---|---|
| Eczema | 41 | 12.1 |
| Acne | 26 | 7.7 |
| Aphthous ulcers | 10 | 3.0 |
| Psoriasis | 7 | 2.1 |
| Rosacea | 7 | 2.1 |
| Balanitis | 3 | 0.9 |
| Lichen simplex | 3 | 0.9 |
| Panniculitis | 2 | 0.6 |
| Chondrodermatitis | 1 | 0.3 |
| Erosive dermatosis | 1 | 0.3 |
| Hidradenitis suppurativa | 1 | 0.3 |
| Lipoid necrosis | 1 | 0.3 |
| Paronychia | 1 | 0.3 |
| Urticaria | 1 | 0.3 |
| Mucosal ulcer | 1 | 0.3 |
| Vasculitis | 1 | 0.3 |
| Miscellaneous | N | % |
|---|---|---|
| Xerosis | 12 | 3.6 |
| Alopecia | 10 | 3.0 |
| Pruritus | 7 | 2.1 |
| Purpura | 7 | 2.1 |
| Scar | 5 | 1.5 |
| Melasma | 4 | 1.2 |
| Hyperkeratosis | 3 | 0.9 |
| Prurigo | 2 | 0.6 |
| Depapillated tongue | 1 | 0.3 |
| Scrotal tongue | 1 | 0.3 |
| Onychodystrophy | 1 | 0.3 |
| Onychogryphosis | 1 | 0.3 |
| Hyperhidrosis | 1 | 0.3 |
| Bites | 1 | 0.3 |
| Radiodermatitis | 1 | 0.3 |
| ID reaction or dermatophytid | 1 | 0.3 |
| Phototoxic reaction | 1 | 0.3 |
| SAHA (seborrhea, acne, hirsutism, and alopecia) | 1 | 0.3 |
| Toxicoderma | 1 | 0.3 |
Compared to other populations described in the medical literature available, in an Indian cohort, the most common lesions were those of esthetic interest (62.3%), all those related to drug therapy, and infectious lesions (27.3%), being fungal (58.7%) and viral (29.3%) lesions the most common of all. Neoplasms were rare (2.1%), and all benign. We should mention, however, that the follow-up period only covered the first 6 months after the transplant.4 In another Italian series, the most frequent infections were fungal, followed by viral and bacterial. All precancerous lesions had late onsets, and most were actinic keratoses, 2 of which turned into SCC, and 2 patients died of Kaposi's sarcoma and melanoma.5 Regarding skin cancer, in an Irish patient cohort, one fourth of the patients developed malignant skin lesions.6 SCC is the most commonly reported NMSC in kidney transplant recipients, followed by BCC (3:1 ratio), while in the overall population, this ratio is inverted.7 In our series, BCC was the most common skin cancer of all (0.69:1 ratio). Similarly, in another Spanish cohort, a SCC/BCC ratio of 1:3.1 was described within the first 3 years compared to a 1:1.4 ratio at the completion of the study.8,9 Various factors, such as genetics, sun exposure habits, and phototype, may play a role in the development of different types of skin cancer. We should not forget that most data on skin cancer in transplant recipients come from populations from Northern Europe and Australia where patients have lower phototypes and different sun exposure habits. On the other hand, the fact that many BCC cases go unnoticed may also explain the differences reported.9
Infectious and inflammatory lesions become more important within the first few years after the transplant, while tumor lesions predominate over time. We should mention that BCC seems to be the most common malignant skin neoplasm in our population of kidney transplant recipients, unlike other studied populations. Given its undeniable association with UV radiation, we should improve knowledge and sun protection habits in these patients since the early stages of kidney transplant.
Conflicts of interestNone declared.