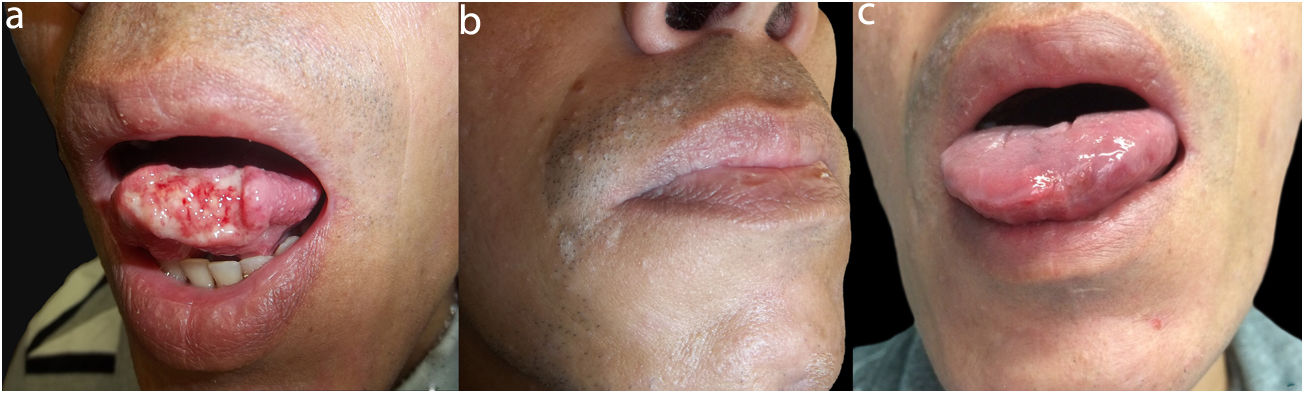
A 37-year-old man came to the clinic with a tongue ulcer that had first appeared 15 days earlier. The ulcer was painful, grew slowly, and caused difficulty eating and speaking. The patient, who was from Bogotá in Colombia, had a history of HIV infection, with a baseline viral load of 261647copies/mL and a CD4+ count of 28/mm3 (2.1%). He had started antiretroviral therapy with tenofovir, emtricitabine, and efavirenz 1 month before coming to the clinic. Physical examination revealed an ulcer on the tip of his tongue (2.2×1cm). The ulcer had irregular indurated borders and a base with fibrinoid tissue. The ulcer was painful on palpation and was associated with a right submaxillary adenopathy. The perioral region contained several pearly papules that were firm in consistency and molluscoid in appearance (Fig. 1A and B). We performed a biopsy, which revealed structures compatible with Cryptococcus species. Therefore, the patient was admitted to hospital. Computed tomography scan of the chest revealed several randomly distributed nodules and a dominant cavitary lesion in the apex of the right lung. We performed fiberoptic bronchoscopy and transbronchial biopsy, which revealed a nonnecrotizing granuloma comprising giant cells that phagocytosed round fungal structures, which were shown to be positive with Grocott stain. Culture was positive for Cryptococcus neoformans. In addition to the serum cryptococcal antigen latex agglutination test, which was positive, the results of other laboratory analysis (e.g., serial blood cultures and latex agglutination of cerebrospinal fluid, bacilloscopy, and culture of bronchial secretions) were negative. The patient was diagnosed with cryptococcal immune reconstitution inflammatory syndrome (C-IRIS), and induction treatment was started with amphotericin B deoxycholate and fluconazole for 2 weeks, followed by 8 weeks of consolidation therapy with fluconazole. The clinical picture had resolved by the end of treatment (Fig. 1C).
C-IRIS is considered clinical deterioration of the disease caused by the encapsulated yeastCryptococcus in immunocompromised patients whose specific immune response improves.1 Pathogenesis is complex and not fully understood, although it seems that after severe immune deficiency, together with the inability to remove foreign antigens, the process is followed by immune restoration leading to a cytokine storm, a rapid increase in CD4 count, and reduced viral load 4 to 6 weeks after initiating antiretroviral therapy, thus leading to clinical expression of the symptoms.2,3
Cryptococcosis is the second most frequent opportunistic infection associated with IRIS and the first in terms of mortality (20.8%). The infection can remain latent for several years after the initial exposure and may remain subclinical for some time.1 Primary infection in the lungs may disseminate via the bloodstream to several organs, thus generating meningoencephalic, gastrointestinal, musculoskeletal, and mucocutaneous involvement.4
Cutaneous lesions are observed in 6% of cases of AIDS-associated disseminated cryptococcosis. The initial lesion is usually a painless papule that is soft in the center and ulcerated at the tip, which sometimes takes on an acneiform or molluscoid appearance (Fig. 1B). The ulcerated papules can become vegetating lesions or plaques covered by serosanguineous crusts, and in patients with severe immune deficiency, they can become complicated with vasculitis, thus generating palpable purpura. Compromise of other areas, particularly the oral cavity, is rare, with only a few cases of localized lesions on the tongue reported, most of which are associated with HIV infection.5–8 The lesion can present as nodules, granulomas, and indurated deep or superficial ulcers, which are similar to carcinoma.8,9 Pleomorphism in mucocutaneous lesions hampers the diagnosis of this infection; therefore, in the case of a tongue ulcer, we should initially suspect other causes of infection such as herpesvirus, cytomegalovirus, and histoplasmosis, as well as neoplastic processes such as squamous cell carcinoma and lymphoma.
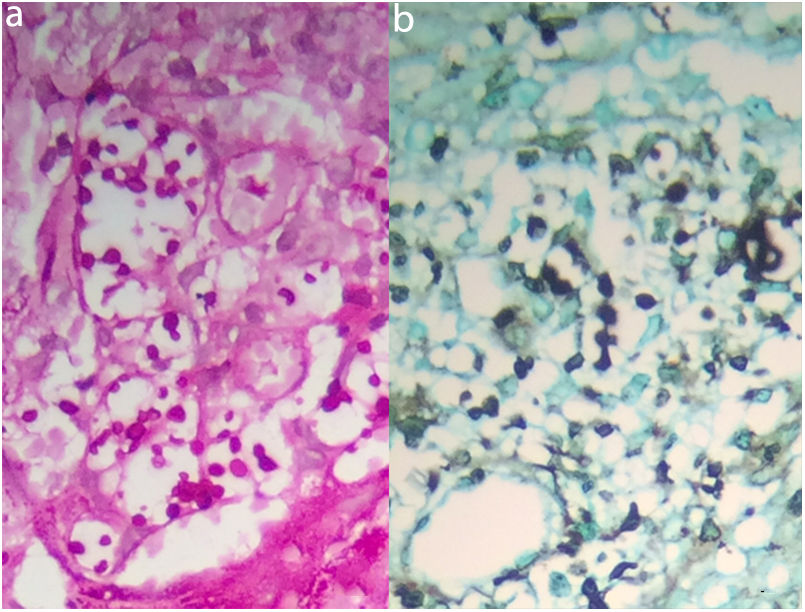
Diagnosis is based on observation of encapsulated yeasts in direct microscopy, isolation of C neoformans or Cryptococcus gattii in culture, and demonstration of capsular antigen in the supernatant of fluids, including serum and cerebrospinal fluid, by latex agglutination or enzyme-linked immunosorbent assay. Stains such as Periodic acid–Schiff, Grocott-Gomori's Methenamine Silver, Giemsa, Alcian blue, and mucicarmine, which were used in the histological sections in the present case (Fig. 2), are specific for cryptococcosis.4,9,10
A, Staining with –Periodic acid–Schiff (original magnification, × 400) reveals an ulcerated epithelium with hyperplasia. Note the mixed inflammatory infiltrate in a fibrous and mucoid stroma containing histiocytic granulomas with clear and abundant cytoplasm. These are full of yeasts of different shapes and sizes, some of which are encapsulated in appearance. B, Staining with Grocott-Gomori's Methenamine Silver (original magnification, × 400). Positivity in the capsule of the yeasts.
In the case we report, the patient received treatment with amphotericin B, which, together with its liposomal derivative and 2 older agents (5-fluorocytosine and fluconazole), forms part of the therapeutic arsenal. These medications can be used alone or in combination, although combination therapy has proven to be more successful.10
In conclusion we present a case of cryptococcosis with unusual manifestations on the tongue of a patient with AIDS in the context of IRIS. Cases of the type described here represent a diagnostic challenge for the multidisciplinary teams that manage this type of patient.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ballén J, Quiroga C, Palma F. Síndrome inflamatorio de reconstitución inmune criptocócico: presentación inusual en la lengua. Actas Dermosifiliogr. 2020;111:617–619.