We report the case of a 35-year-old woman who presented with pruritic lesions on the dorsum of the hands that had appeared 6 months earlier. After she started working as a baker and received small burns, the patient experienced more intense symptoms and the lesions worsened. She reported a lifelong history of anomalous scarring from minor injuries, taking the form of papular and erosive lesions that regressed after 6 weeks. The patient has 2 brothers who have similar symptoms.
Physical ExaminationLesions at various stages of development were observed on the dorsum of the hands and the arms (Fig. 1). These round, skin-colored, and in some cases umbilicated papules measured from 2 to 5 mm in diameter and contained a small central keratotic plug (Fig. 2). The older lesions were macular, light brown, and infiltrated.
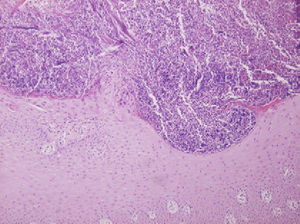
HistopathologyThickened collagen bundles were observed in the superficial dermis. These bundles were surrounded by areas of epidermal proliferation where transepidermal elimination of collagen took place through a small central crater containing keratotic material, mixed inflammatory infiltrate, and cellular detritus (Fig. 3).
Additional TestsThe results of a complete blood biochemistry ruled out abnormalities in glucose metabolism and renal insufficiency.
What Is Your Diagnosis?
DiagnosisFamilial reactive perforating collagenosis.
Clinical Course and TreatmentTopical treatment was started with tretinoin 0.1%, in combination with emollients, on the more recent lesions. The patient was strongly advised to avoid injury and scratching. Improvement was seen in 4 weeks, with a reduction in the number of lesions and symptom intensity.
CommentFamilial reactive perforating collagenosis is one of the primary perforating diseases, a group of disorders characterized by keratotic plugs through which dermal connective tissue is eliminated through the epidermis.1
These diseases fall into 3 main categories: elastosis perforans serpiginosa involving the elimination of elastic fibers, acquired perforating dermatosis with adult onset often related to diabetes, renal insufficiency, or toxicoderma,2 and, least frequently, familial reactive perforating collagenosis.3
Mehregan, Schwartz, and Livingood first described this hereditary disorder in 1967; the etiology is still poorly understood and the pattern of transmission varies.4 The condition is rare and only 50 cases have been described.
From infancy, these patients develop skin-colored papules measuring less than 10mm in diameter in response to superficial trauma. These lesions become umbilicated and eventually form a crater with a small central keratotic plug. They are typically found on the extensor aspects of the arms, the dorsum of the hands, and, less frequently, the elbows, knees, and feet. The palms of the hands and the soles of the feet are not affected. The lesions disappear within 2 months, leaving atrophy and hypopigmentation. The isomorphic response is more typical in this disease than in other perforating disorders.
The basic defect is thought to be due to a genetic abnormality that affects the collagen, leading to greater lability after injury. The same abnormality is also associated with an increase in serum and tissue concentrations of fibronectin and favors epithelial migration and proliferation, resulting in the transepidermal elimination of damaged collagen.5
Histologic examination reveals deposits of basophilic dermal collagen surrounded by inflammatory cells and areas of epidermal proliferation that eventually give rise to transepidermal elimination through a small central crater containing keratotic material and inflammatory cells. Elastic fibres are not affected.6
The differential diagnosis must include inflammatory pathologies (folliculitis, prurigo nodularis, arthropod bites), mucoid material deposits (acral persistent papular mucinosis), and tumors (multiple keratoacanthomas, syringomas, and benign fibrous histiocytomas), in addition to all other perforating diseases.
Several treatments have been described, including emollients, topical corticosteroids, topical retinoic acid, oral isotretinoin, and vitamin A supplements, but the results are varied.6 The hereditary forms of reactive perforating collagenosis are usually mild and localized, with no alarming symptoms except in rare circumstances.
Conflict of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Sánchez-Moya AI, et al. Pápulas umbilicadas en dorso de manos. Actas Dermosifiliogr.2012;103:435-6.