Recent years have witnessed an increase in the use of ultrasound imaging of the skin in the field of dermatology, as the technique reveals details of vessels and other structures that cannot be detected on physical examination. Extradigital glomus tumors are rarely seen in clinical practice and can pose a diagnostic challenge for dermatologists. We report on 4 patients with a clinical suspicion of extradigital glomus tumor and on 1 patient with a clinical suspicion of subungual glomus tumor. All 5 patients underwent ultrasound examination in B mode and color and pulsed-wave Doppler prior to surgical excision of the tumor and histologic examination, which confirmed the diagnosis in each case. Ultrasound imaging of the skin, combined with clinical findings, provided a simple, noninvasive way of making a prompt diagnosis and identifying the exact location of the lesion for surgical removal.
En los últimos años se ha observado un aumento del uso de la ecografía cutánea en el campo de la dermatología, al proporcionar detalles estructurales y/o vasculares que con la simple exploración física no se pueden apreciar. Los tumores glómicos extradigitales son lesiones poco frecuentes en la práctica clínica y pueden suponer un reto diagnóstico para el dermatólogo. Presentamos 4 pacientes con sospecha clínica de tumor glómico extradigital y un paciente con sospecha de tumor glómico subungueal. A cada paciente se le realizó exploración ecográfica en modo B, doppler color y doppler pulsado, exéresis quirúrgica y análisis histológico que confirmó el diagnóstico sospechado. El uso de la ecografía cutánea añadida a los datos clínicos permitió de una manera sencilla e inocua evitar retrasos diagnósticos y determinar la localización exacta para una adecuada exéresis quirúrgica.
Glomus tumors are an uncommon type of benign neoplasm derived from a structure known as the neuromyoarterial glomus, which contributes to regulation of body temperature.1–5 These structures are most often found in the skin, in particular in the subungual region.1 Subungual glomus tumors are suspected when a lesion is found at this typical site,6 accompanied by a clinical presentation of sensitivity to cold and severe pain that can be spontaneous or arise after minimal contact. In contrast, diagnosis of extradigital glomus tumors is often mistaken or delayed given the low incidence of such lesions.3,5 In this study, we aimed to assess the correlation between clinical, histopathologic, and ultrasound findings for extradigital glomus tumors, and compare these findings with the characteristics of digital glomus tumors. We also aimed to describe the usefulness of ultrasound and color Doppler imaging in the diagnosis, surgical treatment, and follow-up of these tumors.
Care ReportWe present a total of 5 patients (Table 1), attended in our dermatology department. Three were men and 2 were women, and ages ranged from 42 to 65 years. All patients were seen for longstanding lesions present for several years on the limbs; all were painful with local sensitivity. With clinical suspicion of glomus tumor, each patient underwent a preoperative ultrasound study with a device equipped with a high frequency probe. Images were taken in B mode and color Doppler mode. Pulsed Doppler techniques were also used to characterize blood flow in intratumoral and peritumoral vessels. All patients had similar ultrasound findings, consistent with a vascularized tumor embedded in soft tissue. Once the extent of the lesion had been defined with the help of ultrasound, it was excised and the surgical defect was directly closed. In the case of the subungual lesion, the tumor was fully excised with access achieved by raising the proximal nail bed. After excision, the surgical defect was closed (Figures 1 and 2).
Clinical Cases: Clinical and Ultrasound Characteristics of the Glomic Tumors.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | |
| Age | 65 | 60 | 46 | 67 | 46 |
| Sex | Male | Male | Female | Male | Female |
| Site | Lateral face of the elbow | Thigh | Thigh | Lateral face of the elbow | Nail |
| Clinical Characteristics | Pink macule of 0.5cm, with a punctiform, erythematous-violaceous papule with central elevationVery painful on palpation | Scar-like macule with poorly defined borders Nodule or underlying tumor not palpablePainful on application of pressure | Two violaceous papules of 0.5cm with a smooth surface on an erythematous-violaceous basePainful on application of pressure | Palpable nodule with overlying skin of erythematous-blue color, with irregular border, measuring 0.8cm approximatelyPainful to touch | Nail dystrophy on the medial face of the first finger of the right handVery painful to touch and sensitive to the cold at this site |
| Lesion duration | 5 years | 35 years | 1 year | 6 years | 4 years |
| Prior Treatment | No | Electrocoagulation | Electrocoagulation | No | No |
| Relapse after excision | No | No | No | No | No |
| Ultrasound study | |||||
| B Mode | |||||
| Site | Dermis | Dermis-hypodermis | Dermis | Dermis-hypodermis | Dermis |
| Echostructure | Solid lesion | Solid lesion | Solid lesion, form of use | Solid lesion | Ovaluated lesion |
| Borders or forms | Regular form | Regular border | Well-defined borders | Well-defined | Well-defined, regular border |
| Echogenicity | Hypoechoic, homogeneous | Hypoechoic, heterogeneous | Hypoechoic, heterogeneous | Hypoechoic, heterogeneous | Isoechoic |
| Stalk sign | + | + | – | + | – |
| Color Doppler | |||||
| Flow± | + | + | + | + | + |
| Site: intralesional/perilesional/both | Intralesional | Intralesional | Intralesional | Intralesional | Intralesional |
| Spectral Doppler | |||||
| Type of flow: arterial/venous/both | Arterial | Both | Arterial | Arterial | Arterial |
Source: Amitay-Laish et al.14
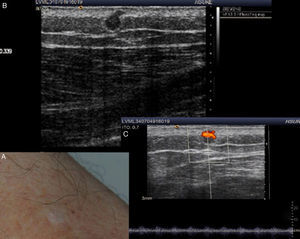
A, Clinical examination of the left thigh shows a scar-like macule with poorly defined borders. B, B mode Doppler ultrasound shows a solid, hypoechoic, spherical lesion with a regular border at the dermal-hypodermal interface. A hypoechoic prolongation in the form of a stalk is seen in the upper part of the lesion. C, Color Doppler mode shows increased vascularization.
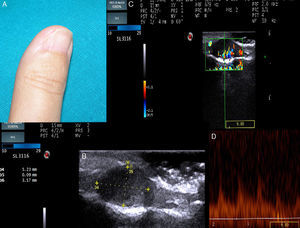
A, The examination shows nail dystrophy on the medial face of the first finger of the right hand. B, B mode Doppler image showing a well-defined, solid hypoechoic lesion with an oval form and regular borders. C, In Color Doppler mode, extensive vascularization can be seen in the nail bed. D, Spectral analysis shows low grade systolic arterial flow within the lesion.
The histologic findings were consistent with glomus tumor, with well-defined solid nodules surrounded by compact fibrotic tissue and no encapsulation. These nodules were comprised of monomorphous polygonal groups of glomus cells. Small vascular spaces could be discerned among these cell groups, surrounded by a fascicle of endothelial cells. In the immunohistochemical study, smooth muscle stained positive for actin and negative for desmin.
Subsequently, all patients underwent regular clinical and ultrasound follow-up and remained free of signs of recurrence. In the patient with a subungual glomus tumor, substantial nail dystrophy was present after surgery as a sequelae.
DiscussionIt is estimated that glomic tumors comprise 1.6% of all soft tissue tumors5,7 and 4.5% of all tumors on the hand. They are classified into 2 variants: solitary glomus tumors and multiple glomus tumors, with clinical and anatomopathologic differences.1
Solitary tumors are the most common and are the subject of the discussion in this article.1 They can manifest in the form of erythematous-violaceous nodule, red-pink or blue tipped macule, or increased curvature or deformity of the nail plate.8 Glomus tumors are classified according to their site as digital and extradigital. Extradigital tumors are less common. The typical clinical presentation is one of localized pain and sensitivity and hypersensitivity to cold (Table 2).1–8
Clinical Differences Between Subungual and Extradigital Glomus Tumors.
| Clinical Characteristics | Subungual Glomus Tumor | Extradigital Glomus Tumor |
| Sex | Female 2:1 | Male 4:1 |
| Age on diagnosis | Twenties and fifties | Forties and sixties |
| Clinical characteristics | Pain, localized sensitivity and hypersensitivity to cold | Pain |
| Correct initial diagnosis | Often | Less often |
Our patients were aged between 60 and 70 years in the case of extradigital sites and all were men, whereas the patient with the digital tumor was a woman in her forties. This is all consistent with what is reported in the literature, even though the sample was not particularly representative given the low number of patients. This difference between sites could be either because the tumor occurs in elderly patients or because often the atypical site of these tumors hinders diagnosis4 and they are confused with hemangiomas, neuromas, or neurofibromas,3,5 with subsequent delay in definitive diagnosis. According to some authors, the mean time to definitive diagnosis of extradigital glomus tumors can vary between 5 and 20 years.3 In fact, in 1 of the cases presented as an extradigital glomus tumor, correct diagnosis was delayed 35 years due to erroneous initial diagnosis and the fact that use of cryotherapy masked the clinical picture.
Ultrasound has only recently been used as an additional study for diagnosis and follow-up of cutaneous lesions. Applications include a range of inflammatory diseases, benign and malignant tumors, and even esthetics.9 In the ultrasound images captured in B mode, glomus tumors are seen as small solid, hypoechoic, well-defined nodules, more or less homogenous, with a regular border, most often located in the superficial dermis, with no involvement of the deep layers.2,4,6,10 In our patients, all tumors were in the dermis except 2 (patients 2 and 4) at the dermal-hypodermal interface. These did not however penetrate the hypodermis. The color Doppler study shows extensive vascularization inside the tumor, as would be expected with a vascular type tumor such as a glomus tumor.2,4,10,11 In addition, the pulsed Doppler study usually shows a low-grade systolic murmur. Both characteristics help us to differentiate such tumors, in the first instance, from other nonvascularized soft tissue tumors.4,12 However, an intense vascular signal in the Doppler study can also be seen in hemangiomas or arteriovenous malformations. Some B-mode ultrasound findings can assist in the differential diagnosis (Table 1). In hemangiomas, grey-scale images do not show such homogenous echogenicity and the margins are less well defined. In addition, vascular flow is diminished as blood pools are present. Malformations are usually more poorly defined lesions compared to surrounding tissue, with no mass effect, and they show the typical arteriovenous shunt.4 Three of our patients had the typical stalk sign. This sign corresponds to a hypoechoic prolongation of the lesion by the stalk, which in Doppler mode reveals an intense vascularization characteristic of vascular lesions such as glomus tumors.2 Nevertheless, images obtained by ultrasound are not specific to any particular lesion, and diagnosis of glomus tumor is clinical, with confirmation from histopathologic study. However, cutaneous ultrasound can guide diagnosis, providing significant information in a simple skin examination.9 Study of ultrasound images is also very useful for exactly, simply, quickly, and painlessly locating the lesion prior to excision. The technique can reveal the relationship with surrounding tissue to enable complete excision with minimal trauma and so avoid subsequent recurrence.2,6,13 Ultrasound has been able to detect tumors as small as 1mm,2 reflecting its usefulness in the early diagnosis of lesions. The limitations of ultrasound are seen with flat lesions less than 3mm across6 and with sites where artifacts may appear, such as subungual if the nail is very thick.13
The use of supplementary magnetic resonance imaging is a useful, noninvasive method, but it is more costly and so its use in everyday clinical practice does not appear to be justified.2,6,8 Radiography is inexpensive and quick, but it is only useful in large tumors and in subungual tumors to differentiate them from subungual exostosis.6
In conclusion, we highlight the usefulness of ultrasound for early diagnosis, detailed information on location, and guidance for complex excision of glomus tumors, as observed in our patients.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Gómez-Sánchez ME, Alfageme-Roldán F, Roustán-Gullón G, Segurado-Rodríguez MA. Tumores glómicos digitales y extradigitales. Utilidad de la ecografía cutánea. Actas Dermosifiliogr. 2014;105:e45–e49.