The COVID-19 pandemic brought about social changes in 2020 and 2021. The aim of this study was to evaluate the epidemiologic profiles of the main sexually transmitted infections (STIs) of bacterial origin (chlamydia, gonorrhea, and syphilis) diagnosed during this period and compare them to findings from previous years.
Material and methodsDrawing on data from Hospital General Universitario in Valencia, Spain, we recorded the number of chlamydia, gonorrhea, and syphilis cases diagnosed monthly by multiplex polymerase chain reaction (PCR) in 2018–2021 and the number of PCR-confirmed SARS-CoV-2 cases diagnosed monthly in 2020–2021. We also collected clinical and demographic information on all patients diagnosed with STIs during the years studied.
ResultsThe total number of STIs diagnosed increased from 570 in 2018–2019 to 664 in 2020–2021. PCR positivity rates were similar in the 2 periods, but the incidence rates were higher during the pandemic. The chronologic correlation between SARS-CoV-2 and STI positivity was negative. Mean age at diagnosis was 29.64 years (95% CI, 19.33–41.14 years) for chlamydia, 30.86 years (95% CI, 20.24–42.45 years) for gonorrhea, and 37.04 years (95% CI, 26.01–51.00 years) for syphilis. The number of men diagnosed with chlamydia increased by 13.85% (95% CI, 6.39–21.08; p=.0003) during the pandemic.
ConclusionsWe observed a negative correlation between SARS-CoV2 infections and STIs during the pandemic and an increase in chlamydia cases among men. STI cases rose during 2020–2021, indicating that they remain a significant problem that needs to be addressed in young and adult populations.
Entre 2020-2021 hemos sufrido una pandemia por el virus SARS-CoV-2. Debido a los cambios sociales por la pandemia, nos hemos propuesto estudiar el comportamiento epidemiológico de las principales infecciones de transmisión sexual (ITS) bacterianas (clamidia, gonorrea y sífilis) durante este periodo y compararlo con periodos previos.
Material y métodosSe recogieron las muestras mensuales de clamidia, gonorrea y sífilis entre los años 2018-2021 y las muestras positivas mensuales de SARS-CoV-2 entre los años 2020-2021 del Hospital General Universitario de Valencia, analizadas por técnica PCR Multiplex. Se recogieron datos clínicos y demográficos de los pacientes con ITS.
ResultadosDurante los años 2020-2021 (pandemia) se diagnosticaron más casos de ITS total (664) que durante los años 2018-2019 (prepandemia) (570), con tasas de incidencia superiores y tasas de positividad similares. Se ha observado una correlación cronológica negativa entre las muestras positivas de SARS-CoV-2 y las muestras positivas de ITS. La edad media de los pacientes con diagnóstico de clamidia, gonorrea y sífilis fue de 29,64 (IC 95% 19,33-41,14), 30,86 (IC 95% 20,24-42,45) y 37,04 (IC 95% 26,01-51,00) años, respectivamente. El número de casos de clamidia en varones ha aumentado 13,85% (IC 95% 6,39-21,08; p=0,0003) en los años de pandemia.
ConclusionesDurante los años de pandemia ha existido una correlación negativa entre los casos de SARS-CoV-2 y los casos de ITS, con más casos de clamidia en varones. Las ITS han aumentado en los dos últimos años, por lo que son un importante problema de salud en la población joven y adulta que merece especial atención.
Sexually transmitted infections (STIs) comprise a heterogeneous group of infections that are transmitted from person to person through sexual contact (vaginal, anal, oral) and through nonsexual contact, for example, blood transfusions or contamination with body fluids. The most prevalent bacterial infections are chlamydia, gonorrhea, and syphilis, all of which are notifiable diseases.1–3
The latest epidemiological surveillance data on STIs in Spain, published in 2019, show that since the year 2001, the incidence of chlamydia, gonorrhea, and syphilis has continued to rise. In 2019, the incidence of these 3 diseases was 44.18, 28.88, and 13.29 per 100000 persons, respectively.4 The incidence rates of gonorrhea and syphilis are higher in men than in women. Those of chlamydia, on the other hand, are higher in women.5–7
The last few years have been characterized by the pandemic caused by the respiratory virus SARS-CoV-2,8 the incidence of which has varied from month to month. During those months when the incidence was high, the Spanish government was obliged to declare a state of alarm with social restriction measures to control the spread of the virus.9
Given that these measures were intended to reduce contact between persons who did not live together, with the subsequent reduction in activities associated with nightlife, we considered whether social restriction measures were also effective for reducing the frequency of the main bacterial venereal diseases and evaluated progress over the last 2 years.
ObjectivesWe aimed to study the incidence of bacterial STIs (chlamydia, gonorrhea, and syphilis) and the characteristics of patients diagnosed with these venereal diseases between January 2020 and December 2021 (pandemic) and to compare our findings with those recorded between January 2018 and December 2019 (prepandemic).
We also studied the effect of the number of positive cases of SARS-CoV-2 infection on the number of positive cases of STI during the pandemic.
Material and MethodsUsing the database of the microbiology department, we collected samples of chlamydia, gonorrhea, and syphilis analyzed by means of multiplex polymerase chain reaction (PCR) between January 2018 and December 2021 from throughout our health department. We also collected SARS-CoV-2 samples from the microbiology department for patients from our health district, independently of the patient's clinical condition, between January 2020 and December 2021, again using the database of the microbiology department. The incidence of STI was calculated by counting the number of positive STI samples from patients in our health district and dividing the result by the catchment population. The rate of positive results was determined by dividing the number of positive samples by the number of samples analyzed. We recorded the age and sex of patients with positive STI samples from the different years of the study and analyzed the data using SPSS (IBM Corp).
ResultsWe found 692 cases of chlamydia, 441 cases of gonorrhea, and 101 cases of syphilis between January 2018 and December 2021.
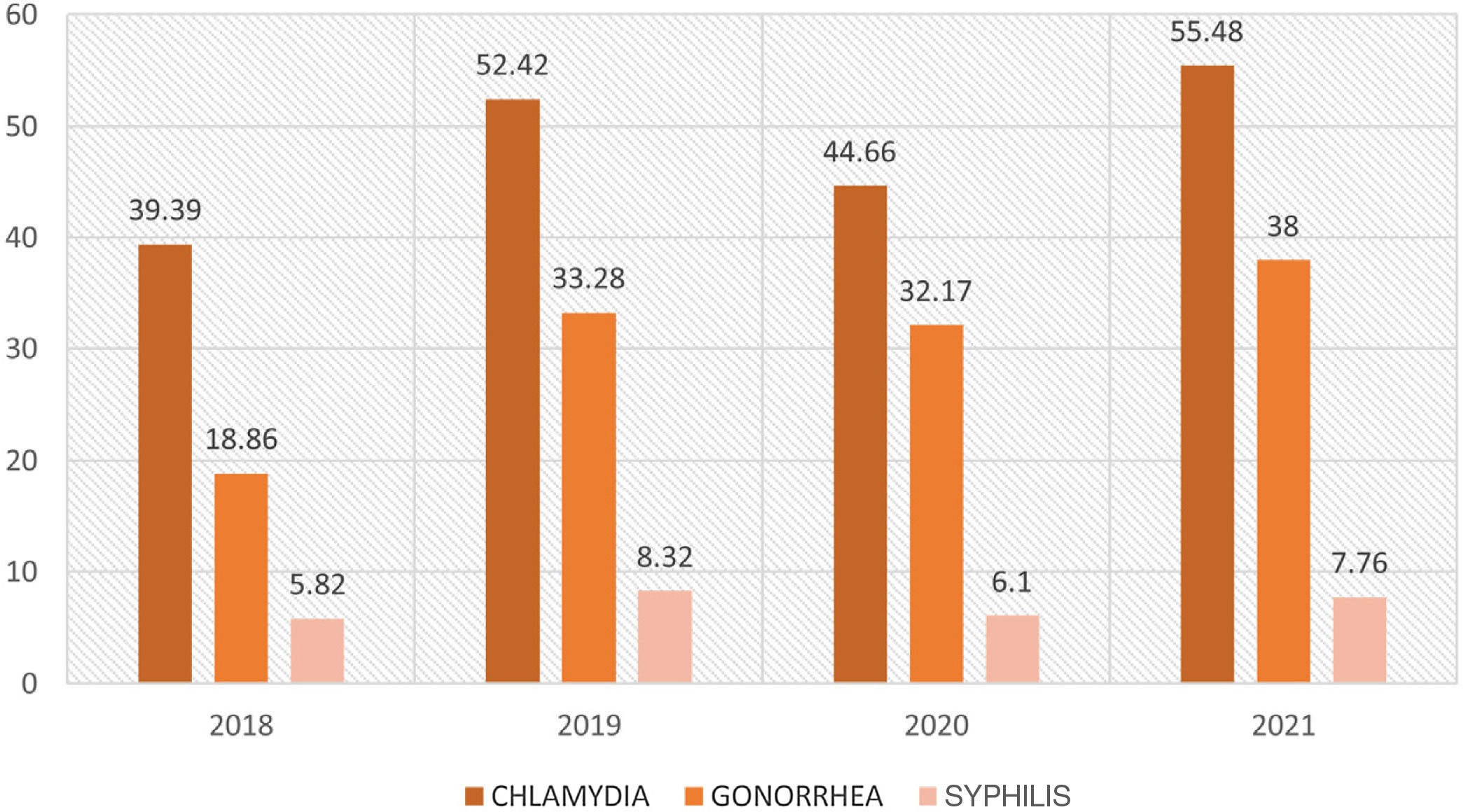
The incidence rates of the 3 STIs were calculated for the years assessed (Fig. 1). We observed a decrease in the incidence of chlamydia, gonorrhea, and syphilis in 2020 compared with 2019 (7.76 [95% CI, 2.9–14.93], 1.11 [95% CI, 0.02–5.57], and 2.29 [95% CI, 0.24–7.22] cases per 100000 persons, respectively). In contrast, in the year 2021, the incidence rates for chlamydia and gonorrhea were the highest reported in recent years.
The number of samples of chlamydia, gonorrhea, and syphilis analyzed during 2018–2019 (prepandemic) were 4050, 3406, and 245, with positive results detected for 331, 188, and 51, respectively. In comparison, the number of samples of chlamydia, gonorrhea, and syphilis analyzed in 2020–2021 (pandemic) was 4741, 4676, and 272, with positive results in 361, 253, and 50, respectively. These data were used to calculate the rate of positive results; the findings were similar for all 3 infections during the years of the pandemic and previous years, namely, 8.17%, 5.51%, and 20.81% in 2018–2019 and 7.61%, 5.41%, and 18.38% in 2020–2021, with no statistically significant differences. We obtained more positive samples of chlamydia and gonorrhea during the years of the pandemic than previously and found similar figures for syphilis in both periods (Table 1), with a total increase of 94 positive samples corresponding to an increase in the incidence rate of 26.03 cases per 100000 persons between 2018–2019 and 2020–2021.
Number of Positive Samples, Samples Analyzed, and Positive Result Rates for the 3 Sexually Transmitted Infection Before and During the Pandemic.
| Positive samples | Samples analyzed | Positive results, % | |
|---|---|---|---|
| 2018–2019 (prepandemic) | |||
| Chlamydia | 331 | 4050 | 8.17 |
| Gonorrhea | 188 | 3406 | 5.51 |
| Syphilis | 51 | 245 | 20.81 |
| Total | 570 | 7701 | 7.40 |
| 2020–2021 (pandemic) | |||
| Chlamydia | 361 | 4741 | 7.61 |
| Gonorrhea | 253 | 4676 | 5.41 |
| Syphilis | 50 | 272 | 18.38 |
| Total | 664 | 9689 | 6.80 |
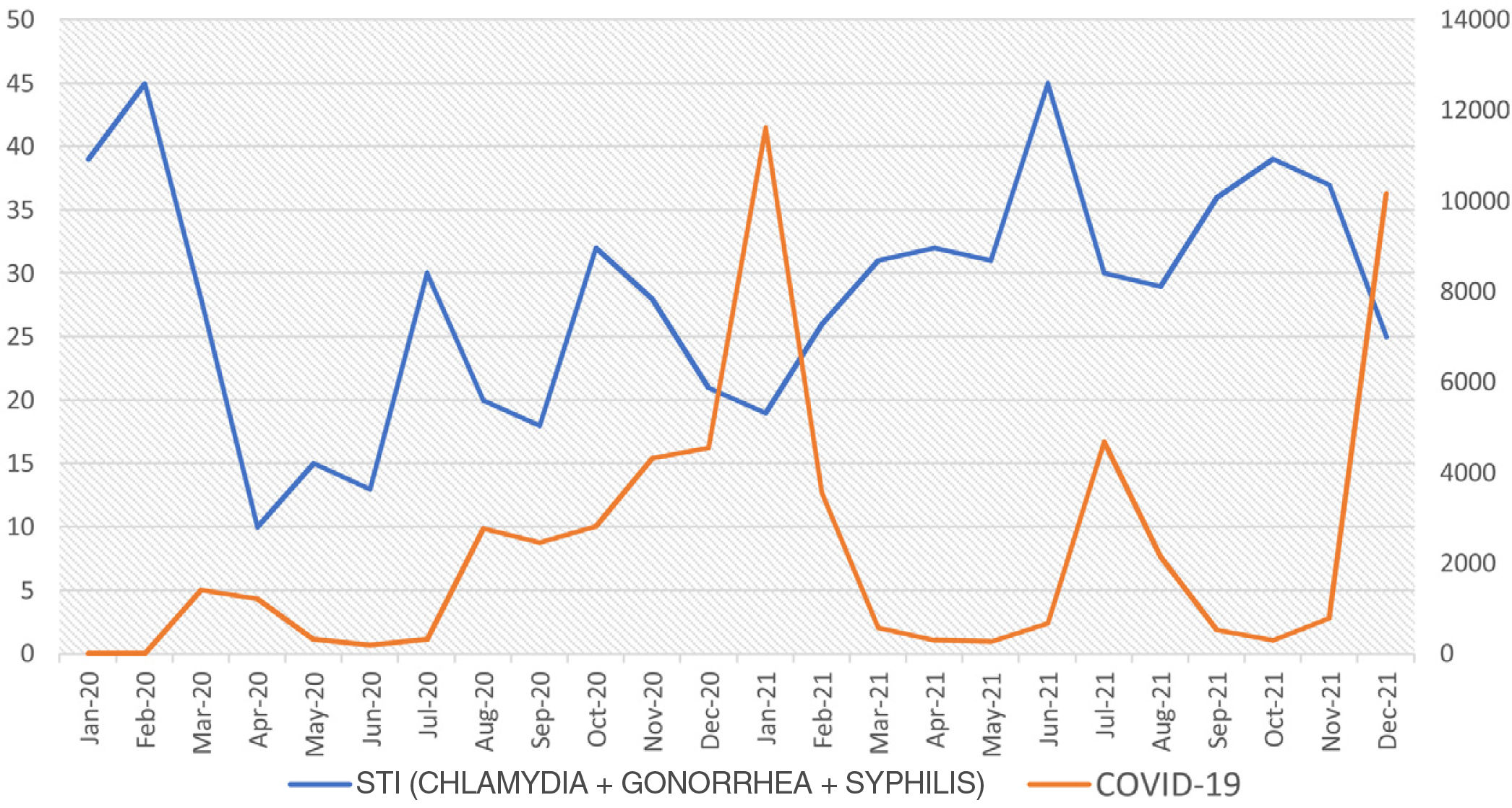
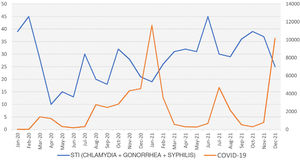
Cases of the 3 STIs from 2020–2021 were studied chronologically (month by month). The 3 diseases progressed in parallel during this period, with increases and decreases in chlamydia, gonorrhea, and syphilis at the same time points. We also analyzed PCR-positive SARS-CoV-2 samples from patients in our health district during January 2020 and December 2021. The chronological (monthly) data of the positive SARS-CoV-2 and STI samples were compared. The curves generated progressed in opposite directions, with increases in the number of positive SARS-CoV-2 samples occurring in parallel to marked decreases in the number of positive STI samples and, similarly, sharp decreases in the number of positive SARS-CoV-2 samples coinciding with rapid increases in the number of positive STI samples, with figures approaching those of the prepandemic period (Fig. 2).
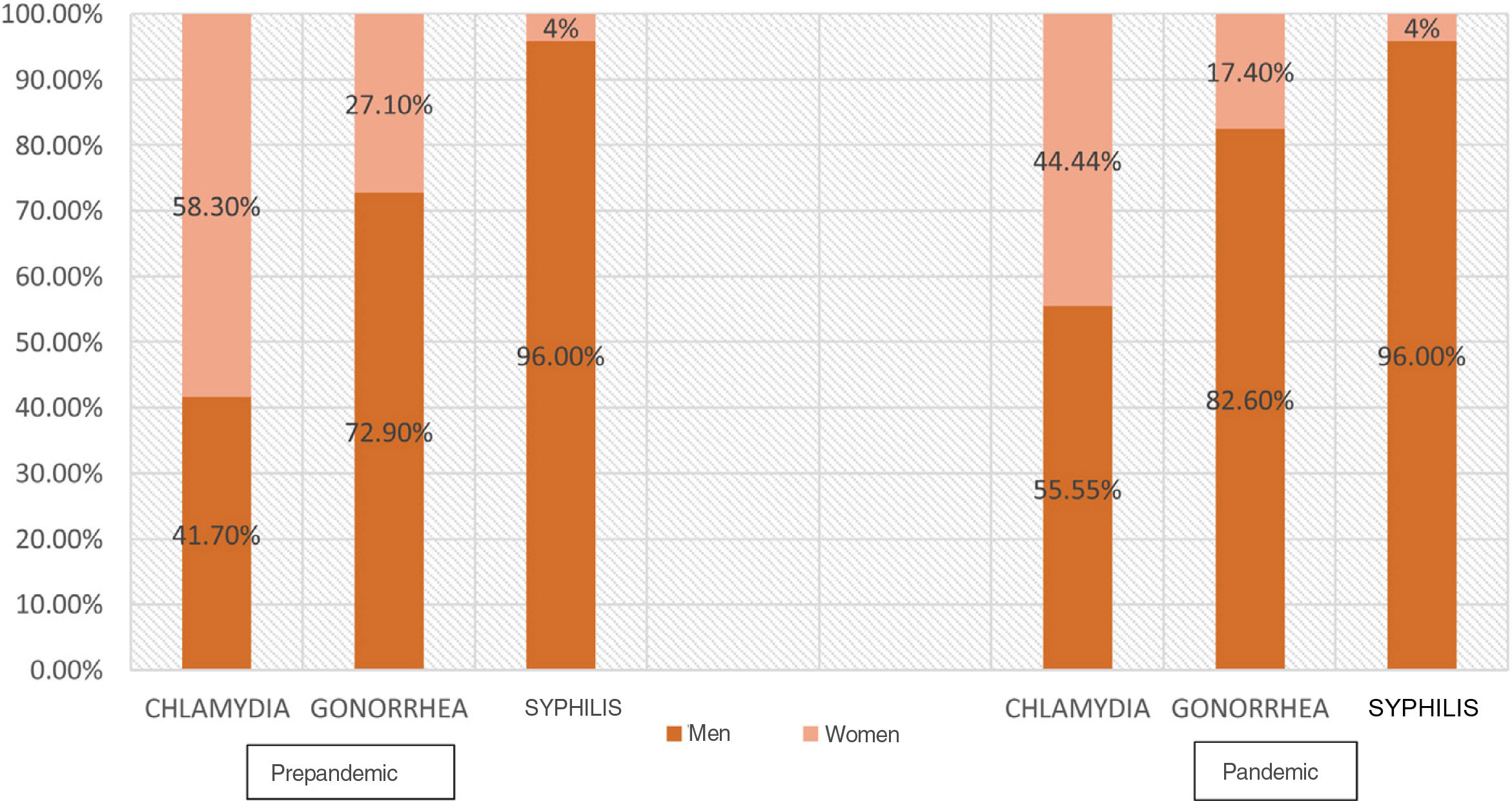
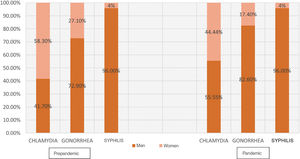
We observed no differences in the age of patients diagnosed with STIs during the pandemic compared with the previous years. The mean age at diagnosis of chlamydia, gonorrhea, and syphilis throughout the study period was 29.64 (95% CI, 19.33–41.14), 30.86 (95% CI, 20.24–42.45), and 37.04 (95% CI, 26.01–51.00) years, respectively. Significant differences were recorded in the percentage of males diagnosed with chlamydia during the pandemic compared to the prepandemic period (55.55% vs 41.7%), i.e., 13.83% (95% CI, 6.39–21.08; p=.0003) more diagnoses in males during the pandemic. No further significant differences by sex were recorded for the other STIs (Fig. 3).
DiscussionWe collected a total of 1068 positive STI samples between 2018 and 2021 with the aim of evaluating possible changes in the behavior of these infections during the SARS-CoV-2 pandemic. We observed a decrease in the number of positive STI samples during 2020 compared with 2019. This decrease runs against the continuous upward trend for cases of STI that has been observed since the start of the 21st century. The decrease in cases of STI in 2020 could be due to the effect of the social restriction measures implemented to control the spread of SARS-CoV-2, together with the fear of infection by the virus among the public. During the first stages of the pandemic, the normal functioning of our STI clinic was affected, with a decrease in the number of regular appointments and in the number of urgent appointments. The reduced frequency of face-to-face visits led to fewer analyses being performed for the diagnosis of venereal disease. These behaviors were reversed when the social restriction measures were relaxed, with an increase in the number of regular visits and urgent appointments for a suspected STI. These data agree with those reported in other studies, which show a decrease in cases of STI during the months when the incidence of SARS-CoV-2 infection was high.10,11
In order to analyze whether a greater or lesser number of tests for diagnosis of STI were performed and thus interpret our results, we recorded the rates of positive results during and before the pandemic. Positive results stabilized over the 4-year study period, with even lower values in 2020–2021, although no significant differences were recorded. This finding would contradict the possibility of having analyzed a lower number of STI samples owing to a reduction in the number of visits because of the SARS-CoV-2 pandemic, since in that case, the positive results rate would have been higher during the years of the pandemic. Similarly, by observing the absolute number of samples analyzed for the different venereal diseases during both periods, we can see that a greater number of STI samples were analyzed in 2020–2021 than in 2018–2019. These results enable us to compare the incidence rates for both periods, assuming the absence of bias owing to the epidemiological situation.
One notable finding of our study was that after analyzing the positive STI samples from before and during the pandemic, we observe higher figures both for the absolute number of positive samples and for incidence rates during the pandemic (2020–2021) than before the pandemic (2018–2019). Consequently, despite the decrease in venereal diseases in 2020, the year 2021 saw an increase in STIs, with higher figures than in previous years and a return to the upward trend we observed before the pandemic.
The analysis of STI data chronologically and comparison with data for positive SARS-CoV-2 samples during the pandemic in patients from our health district yielded 2 graphs illustrating contrasting behavior: STIs decreased considerably during the first wave of SARS-CoV-2 in March 2020 and, as the number of cases of SARS-CoV-2 decreased, the number of cases of STI increased sharply. This behavior was cyclic throughout 2020 and in 2021, albeit with gradually less marked decreases in the number of STIs. The number of positive STI samples at the end of 2021 returned to values similar to those recorded before the pandemic. Therefore, we observed a pronounced effect of the number of positive SARS-CoV-2 cases on the appearance of positive STI cases during the pandemic. This effect gradually diminished as the pandemic continued over time. Our data are very similar to those reported elsewhere, that is, sudden decreases in cases of venereal diseases during the months when the incidence of SARS-CoV-2 was highest, with sharp increases also during the months when incidence was lower and even, as we observed, exceeding figures recorded before the beginning of the pandemic.12–14
Chlamydia inflection is more prevalent in women throughout the world, as seen in our results from before the pandemic.15 In contrast, we found a significant 13.83% more cases of chlamydia infection among men during the pandemic than before. Values for the other STIs did not differ by sex. We have not seen this finding reported in other, similar studies. We are unable to account for this epidemiological change, although it could be due in part to a reduction in scheduled visits to the gynecologist and a decrease in STI screening tests in women owing to the pandemic, more frequent symptoms of chlamydial urethritis in men, and possible coinfection in men. However, the similarity in the rates of positive results for chlamydia infection before and during the pandemic would contradict part of this theory.
ConclusionsSocial restriction measures and fear of contracting SARS-CoV-2 infection led to an initial decrease in the frequency of STIs, with a clearly negative correlation between positive cases of SARS-CoV-2 infection and positive cases of STI. However, this change in the behavior of venereal diseases did not persist during subsequent months, and the year 2021 finished with the highest STI figures recorded to date. Similarly, we found an increase in cases of chlamydia infection among men during the pandemic compared with before the pandemic. However, we are unable to account for this difference.
Therefore, STIs are currently one of the main health problems in young persons and adults. Prevention and information campaigns should be implemented, as should measures to raise awareness, once the alarm generated by SARS-CoV-2 has subsided.
Conflicts of interestThe authors declare that they have no conflicts of interest.