The Tinea Hospital in Granada, Spain, was a charitable health facility founded in the 17th century and still treating patients well into the 20th century. The hospital accepted patients from anywhere, not only those residing in the surrounding area. We describe the hospital's founding and the characteristics of the patients and caregivers. We also discuss how tinea was considered at the time, including the typology and treatment protocols applied as well as diet and hygiene measures used. It is striking that a hospital so focused on treating a single disease did not produce studies on the condition or on the application of contemporary knowledge to guide treatment.
El Hospital de la Tina, fundado con fines benéfico-sanitarios en el siglo xvii, ha fun-cionado desde entonces hasta bien entrado el siglo xx realizando el tratamiento de las ti¿nas apacientes de todas procedencias acogidos en la institución. En el presente estudio describimosla fundación del hospital, las características de los pacientes y sus cuidadores, así como lo quese consideraba ti¿na, sus tipos, la pauta de tratamiento y los cuidados alimenticios e higiénicos. Nos llama la atención que la presencia tan temprana de un hospital «monográfico» no se tradujoen estudios sobre la enfermedad y la aplicación de los conocimientos de la época.
Seventeenth-century Granada was served by nearly 20 institutions sheltering the poor or the infirm. One of them specifically addressed the needs of persons with tinea infections well into the early 20th century. Its full name was Hospital de Nuestra Señora del Pilar de Zaragoza but it was generally known simply as the Tinea Hospital. This facility was probably the first hospital dedicated to treating a single disease in the Spanish territory, and it attended a considerable number of cases until most of its assets were lost after 1795, during the expropriations of ecclesiastical properties under the administration of Manuel Godoy. From that time forward, the hospital languished until it disappeared as a health care facility during the 1920s. Today the building houses an orphanage run by a charitable order of nuns (Hermanas Mercedarias de la Caridad), who very kindly gave us permission to consult their archives documenting the hospital's work.
This paper describes the founding of the hospital, the caregivers who worked there, the types of tinea they were familiar with, and the treatments they applied.
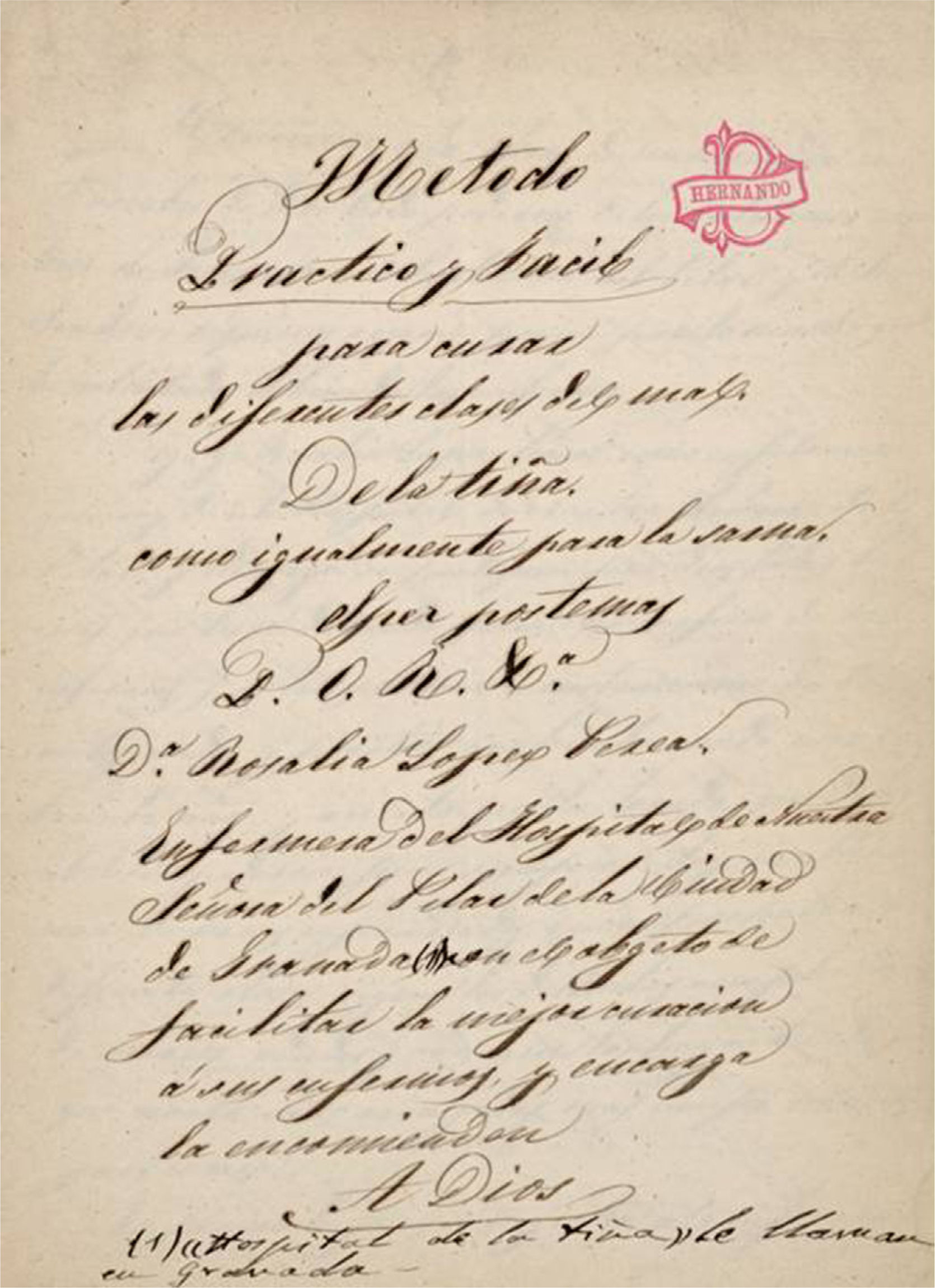
The Founding of the Tinea HospitalHospital de Nuestra Señora del Pilar de Zaragoza, popularly called the Tinea Hospital, was founded by Joseph de la Calle y Heredía, one of the gentlemen who sat on the city of Granada's Council of Twenty-Four (Caballeros XXIV). The newly constituted hospital (Fig. 1), which was located in the Albaicin, the city's old Arab quarter, was built on the remains of an early 15th-century palace that had belonged to Boabdil el Chico, the last of the Nazrid kings of Granada.1
What we know about the hospital's founder comes from his own last will and testament.2 He was very probably a native of Granada, born around 1600; he died in the same city on April 16, 1676, and was buried in the convent chapel of Santa Isabel la Real. He was also a member of the Spanish legislature (the Cortes) and a captain in the cavalry during the Thirty Years’ War. Wounded in the Battle of Lerida in 1642, de la Calle y Heredía lost the use of his right arm and was held prisoner in France for a time. He never married and had no known offspring.
A plaque at the end of the hallway that gives access to the old hospital summarizes the founder's ideas about caring for the poor and infirm as a work of compassion. The views expressed were undoubtedly the sentiments that gave rise to the decision to establish the hospital: The duties of love: To welcome the poor, the beggar and the pilgrim, to feed the hungry and clothe the naked as acts of compassion incumbent on us all. When the poor ask, do not hesitate to give with an open hand. Reader, despise not the poor and never walk away when you see them. Help the scabrous, the leper, the mute, or those of pestilent breath, for the spirit of love demands it of you.
On his death Joseph de la Calle left his entire estate to support the founding and maintenance of a hospital to be placed under the protection of Our Lady of the Pillar, who had appeared miraculously in Zaragoza.2
Patients and CaregiversThe hospital's charter stated that its purpose was to care for patients “who have appalling diseases that distress the faithful and move them to pity,” very probably explaining the institution's decision to provide care for those with skin conditions. Moreover, the founder explicitly mentioned those suffering from tinea in his will, writing that these and similar unfortunates should be cared for “so that they do not wander the streets.”3
Although patients from Granada were given preference, anyone could apply for admission. Patient rosters list applicants from all over Spain and even some from abroad.4
Those from France were expressly mentioned in the benefactor's will: “I beg [the trustees] not to exclude the poor from France, because there is much charity in that Kingdom and it was extended to prisoners once detained there.”
Senior nurses, both male and female, who lived at the hospital, took charge of care, cleaning and treating lesions with the help of several assistant nurses. They were also required to be familiar with exactly what the physician had prescribed: “At another table a senior nurse should assist the physician [in providing] what each patient has been ordered to take at the specified time.” Patients had to be closely supervised, and this task was assigned to assistant nurses: “And [the supervising nurses] should not leave the ward unattended, day or night, in case some sudden accident should happen.”3 The physician's constant attendance does not seem to have been crucial, as ward visits were required only twice a day and, understandably, whenever there was an emergency. This regimen of visits suggests that some patients might have had problems other than tinea, as that condition would not have necessitated morning and afternoon visits. The physician, in the presence of the hospital's rector, was also charged with examining new applicants. Once a diagnosis had been made, an order of admission was written up. Later it would have to be countersigned by the trustees. When a new charter was prepared for the hospital in 1805 to adapt the earlier provisions to a new era, it is likely that only patients with ringworm were being treated, as the new schedule stipulated that the physician would visit weekly, on the day treatments were applied.5
The 1805 charter made reference to other offices as well. There was a position for a chaplain, who was charged with hearing the confessions required of all patients on admission, as well as a barber-surgeon, an apothecary, an attendant in charge of the dispensary, a cook, a laundress, and a porter. A large number of persons ministered to the patients, and along with trustees and the rector—all with corresponding compensations and perquisites—they undoubtedly consumed most of the foundation's resources, to the detriment of the patients themselves.
No statistics were compiled to tell us the number of patients or the duration of treatments, although a complete set of patient rosters for the 18th century and lists of ordinary and extraordinary expenses have been preserved in the archives.6 From these sources we can deduce that the hospital's major outlay was for feeding the inpatients, as was the case for other similar institutions. As a result, it was not possible to admit all applicants, but rather only those who could be fed. According to our calculations, based on amounts listed in the expense ledgers, about 50 patients were housed on average.
In July of 1901, the hospital was visited by 3 professors from the Faculty of Medicine in Granada: Dr López-Peláez Villegas, an ear, nose and throat specialist; Dr Sánchez Aguilera, an ophthalmologist; and Dr Velázquez de Castro, a pharmacologist.7 The third published a report of their visit in the city's medical journal.8 None of them were specialists in dermatology, a problem that perhaps deprives us of precise information. The report might have been quite different if José Pareja Garrido, then professor of dermatology in the same faculty,9 had been present.
In 1892, the facility was taken over by the order of nuns who currently run the orphanage; in the hospital, they were helped by 2 nurses, who administered treatments, and a porter, who also carried out nursing tasks. If a physician was required, the sisters sent for Juan González Rodríguez, who lived in a small square nearby (Placeta de los Porras) and who Velázquez de Castro described as “the old doctor of the Albaicin.”8,10 According to the last known published mention of the hospital, in the newspaper La Alhambra on October 31, 1923, patients with tinea were still being attended at that time. No later references have been found.
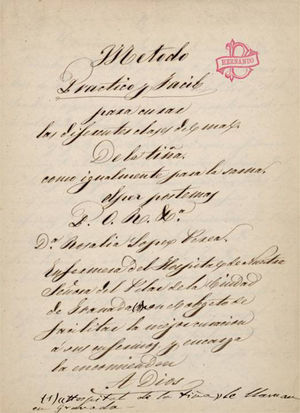
Types of TineaA manuscript from the end of the 18th century or beginning of the 19th describes cases of tinea treated at the hospital at that time, though we think the clinical features would not have been much different in the 17th century. The author was Doña Rosalía López Perea,11 a senior nurse at the hospital. The title for the manuscript (Fig. 2) promised details of an easy, practical approach to treating several types of tinea. Four were described. About Type 1, she wrote this: One type is known as the dry form and is the worst, as it takes a year or more for some patients to be cured. Pimples the size of the head of an ordinary pin are dispersed over the scalp and isolated from each other, in the midst of a white material like saltpeter.
This description seems to correspond to favus, variously called tinea lupinosa by Galen in the second century, corrosive tinea by Ambroise Paré in the 16th century, and then tinea vera by Anne Charles Lorry and porrigo lupinosa by English authors.12,13
This form has fairly characteristic features. It usually presents with dry scaling of the skin (the white material “like saltpeter” that is mentioned in the Granadan nurse's description), spreads over the scalp, and leads to inflammation that extends deep into the follicles. Pustules form (“pimples…the size of the head of an ordinary pin”) along with crusts that thicken to form masses of small cup-shaped yellowish scutula. As the senior nurse indicates, favus was difficult to manage and a cure must have come slowly in those times. Type 2 tinea was described as “a kind of rash.”
This type was undoubtedly the one we now call tinea capitis, and that was called tinea, or herpes, tonsurans by Pierre Louis Alphée Cazenave (1840) or herpes circinatus by Jean-Louis-Marc Alibert (1841), according to Arenas Guzman.14 Today this type encompasses 3 different clinical forms. In one of them, fungi of the genus Microsporum cause one or several small patches of hair loss, with papules surrounding the hair follicle, where broken hairs measuring 1 to 3mm can be observed. In the second, Trichophyton species cause a larger bald patch with scales and black dots derived from hairs broken off at the follicular opening. The third form, favus, is uncommon today. The response to treatment is considerably better in this second type than in the first, as López Perea mentions in her manuscript. Type 3 was described as “another form with small black lesions….”
It is difficult to find a correspondence between this description and any form of tinea in modern classifications. The nurse might have been referring to tinea capitis caused by Trichophyton species. Alternatively, she might have been seeing a scalp infection such as impetigo. Galen listed impetigo among the tinea afflictions grouped under the concept of favus, using it the term strictly in accordance with its Latin sense of honeycomb, evoking the sticky crusted masses typical of this disease. Type 4 was described thus: “another form is white, with large hut-shaped lesions that seep; it is the easiest one to cure.”
This type seems to correspond to inflammatory tinea or kerion, which William Tilbury Fox considered a trichophytic infection with inflammation secondary to bacterial contamination.15 Nevertheless, the fact that the nurse states that this form is easier to cure suggests to us that that she may simply be referring to impetigo, though to be sure of that there would have to be lesions in parts of the body other than the scalp.
TreatmentLopez Perez's11 account of practice at the hospital tells us that it was common to wait until patients were at least 4 years old before starting treatment, undoubtedly because the remedies available were extremely hard to tolerate. She also indicates, however, that treatment was occasionally started once an infant had passed the age of 1 year, but exercising extreme caution. The approach for such a young patient was much gentler. The nurse applied pitch plasters that were as small as possible and cooled them before placing them on the skin. Protect the integrity of the infant's scalp was critical.
Treatment began by first cropping the patient's hair close to the scalp, which was then coated with Flanders salve. This gentle, emollient salve was relatively free of water but had been kept in water at least 15 days to eliminate its salt content. The salve facilitated the removal of crusts, and applications were repeated daily until the scalp was clear of them and thus ready for the plasters. If the the patient's scalp was not then completely clear of lesions, the head was washed with mallow water.
The plasters were strips 4 fingers in width that had been soaked in a fairly diluted solution of hot tar. Several strips were applied to the scalp and the whole was then covered with brown paper. The nurse began applying the plasters at the front of the scalp and moved back, attempting to make sure they adhered. Pitch was used by itself in summer, but in winter or whenever the temperature dropped, it was necessary to mix the pitch with small pieces of tallow (12 pounds of pitch to a quarter pound of tallow).
The plasters were pulled off after a period not to exceed 8 days. Removal was accomplished by 2 caregivers: a senior nurse and an assistant nurse. The purpose of this procedure was to remove all hair from the scalp, and any isolated hairs left were carefully plucked out with tweezers. The scalp was then wiped with “an old rag,” which is to say, a cloth softened by use. Alternating this treatment with the application of Flanders salve, new plasters were soon applied, to be stripped off at the next session. These applications and removals went on for months in this way, until the tinea was thought to have been eradicated.
Complications were not infrequent, especially in cases of long-standing infections. Scalp lesions that bled were swabbed repeatedly with a mild vinegar solution (2 parts vinegar, 1 part water). If bleeding continued, the lesions were also swabbed with ardent spirits. Once bleeding had been brought under control, the usual treatment with plasters recommenced, although fewer at a time were applied to a fragile scalp. Blisters and pimples underwent the same treatment. “Dandruff” was removed with a black ointment made from a base of “well toasted oil in which mallow roots, animal fat, and tar (from the center) have been fried.”
An incipient tinea infection was treated less aggressively, without the use of plasters. The agents used were diluted vinegar, Flanders salve, and mallow water. When treatment with pitch plasters plus Flanders salve was ineffective, however, caregivers resorted to yet another treatment: If [a cure] is not accomplished by means of plasters, that approach must be abandoned, and warm poultices of mallow water should be applied, followed by a white salve and covered with brown paper. This should be done on all the treatment days.
The recipe to prepare the white salve was described as follows: Place a new vessel on the fire with a pound of oil. Add many mallow roots and when they are well cooked, remove them. Add 11 oz of wax and when it is melted, remove the vessel from the fire and stir it continuously with a branch of the mallow bush. When the mixture is warm, add half a pound of powdered white lead, mix well and stir until the salve thickens.
The condition the nurse called dry tinea, which she described as the most difficult to cure, required an additional treatment the author herself characterizes as empirical, or derived from her own experience. This technique relied on alternating the use of pitch, vinegar, and exposure to air. This regimen lasted a single month rather than an entire year.
If tinea corporis developed, only Flanders salve was applied and covered with brown paper. If maggots appeared on the scalp, they had to be removed with tweezers. The ulcers were then washed with water boiled with wormwood—an old remedy known to work as a vermifuge.16 Wormwood water would also be used to prepare poultices to apply afterwards. Once the scalp had been dried with a cloth, “course pine powder” was sprinkled on it and the skin was covered with a pitch plaster.
The patients were also purged at the time of each waning moon as a sort of adjuvant treatment reminiscent of Galenic medicine, which prescribed periodic purging or bleeding to eliminate the noxious humors that caused various diseases. It must be said that the treatments used at this hospital do not seem to have changed at all while the facility was in operation—a period spanning over 2 centuries. This can be inferred from the report of the 1901 visit8 made by the 3 professors from the Faculty of Medicine. Velázquez de Castro described the treatment of 13 children living at the hospital at that time in these words8: On Tuesdays, the heads of these small patients were given a helmet-like covering made of plasters of pitch and tallow, of which we have the formula. On Saturdays, the plasters were energetically stripped off. It was distressing to see the terrible pain this process caused…. Later the children were carefully treated with pure Flanders salve…. Any type of bathing hurts them.
Regarding the duration of treatment, the visiting physician reported that “we were told treatment took a long time, lasting at least 5 months. Normally it went on for a year or a year and a half before a cure was accomplished.”
A footnote in the cited article mentioned that Eugéne Guibout reported having abandoned this method of applying plasters at least 25 years earlier, because it was “barbarous, painful, and of scarce effect.”
Between 1871 and 1873 José Eugenio Olavide published a book that included illustrations of generalized favus17; the figures were numbered 1 and 2 in the book and attributed to the phytoparasitic group of dermatoses. Olavide proposed the following treatment for the condition: [Apply] an emollient poultice to the head and, after the crusts have fallen away, wash with soapy water in the morning. Remove hairs with a tweezer. Apply a solution of corrosive sublimate and, at night, a salve of the sublimate (6 g per ounce of salve).
Illustrations 6 and 7 in the same book show tinea, or herpes tonsurans, which Olavide treated thus: Several times daily apply a solution of corrosive sublimate, 6 g in an ounce of distilled water. Remove all hairs in the area of the tonsure, to a margin of 1cm around the infection. Then, instead of the solution of corrosive sublimate, use the salve (6 g of the sublimate per ounce [of salve]). If irritation and a reaction develop, treat with light applications of oil of juniper.
Returning to the manuscript of Nurse López Parea,11 we note that the patients’ daily meals consisted only of a bowl of thick soup made with chick peas, meat and bacon, a dish that was common everyday fare in 19th-century Spain. Certain foods were to be avoided once the patient's condition was cured and, in our opinion, were even more inadvisable while treatments lasted. The foods on this list were blue fish, “hut products” (which we understand to be dairy products such as milk and cheese, especially cured cheeses), furry-skinned fruits (most probably peaches and apricots), grapes, fresh and dried figs, anything spicy, broad beans, cabbages, radishes, and anything considered “choleric” (which we take to refer to any stimulant).
This diet corresponded to principles that had governed nutrition since the days of classical Galenic medicine, characterized by avoidance of dairy products in general and cured cheese in particular. Fruits and vegetables were avoided because they contained too much water, which was considered harmful to patients with tinea.
The manuscript also specifies certain precautionary measures for the first 3 months following clearance of the lesions, while the patient remained in quarantine: “Patients will keep their hair very short and wash their heads daily with diluted vinegar or mallow water.” If scabs formed on the scalp, they were to be cleaned off by rubbing “with brown paper and oil and then with paper only, until the scalp is dry.”
As a precaution against moisture, for the reason mentioned above, patients were forbidden to use water on their feet or heads for a whole year after their skin had cleared. If dandruff developed during that year, they were instructed to apply a black ointment the hospital supplied on discharge. If the scalp broke out with pimples that were “colored and had white points, these lesions should be removed and the hair pulled out by the root against the direction of growth and the blood squeezed well out. Then wash the head with diluted vinegar and apply Alderete's unguent.” This unguent was prepared according to the following recipe: Take two 4-lb barrels of oil. To one of them, add small pieces of elderberry flowers until they take up half the volume of oil. To the other barrel, add the same proportion of roses. Cover both and leave them in the sun for at least a year. Place these oils in a vessel, add a quarter pound of soda, and heat. Remove the mixture from the fire and when it has cooled but is still warm, add 4 oz of powdered sulphur and 3 oz of verdigris. Stir with your hand until well blended.
Strict cleanliness—of body and clothing—was recommended as a complementary measure even though bathing was to be avoided. In fact, according to the treatment approach described in the nurse's manuscript,11 bathing was proscribed in all skin diseases, whether herpes, scabies, abscesses, ulcers or any other lesion.
Close to the time when the patient would be discharged (“sent out on the street” according to the vivid phrase that was used), certain evaluations had to be made, given that there was risk the patient would have to be readmitted if all was not well. Once cleared for discharge, the patient was usually provided with some type of clothing—above all a pair of hemp-soled espadrilles, given that many had traveled from distant places. We recall the case of a patient from Seville whose footwear was in shreds on admission.6
Comments- 1.
For over 2 and a half centuries, from roughly 1680 to 1920, Granada's Hospital de Nuestra Señora del Pilar de Zaragoza, widely known as the Tinea Hospital, offered what we could describe as specialized care for individuals with tinea infections. The patients came from many places, but above all from the territory corresponding to the old Kingdom of Granada.
- 2.
Four types of tinea were defined and each received some form of treatment based on depilation of the scalp and various adjuvant measures. Cures were accomplished with these means, although the duration of treatment was relatively long. In addition, there was agreement on certain dietary and hygienic measures, and patients were advised on what to do during convalescence, possibly making readmission less likely.
- 3.
On the other hand, this early specialized hospital produced no research on the disease that could have contributed to improve knowledge. Nor did it develop treatments that required less time or were less aggressive and more effective. This deficit is especially surprising since a good level of understanding of tinea had been attained by the end of the 19th century. We can conceive at least 2 possible explanations for the lack of research:
- a)
The hospital's mission always focused on providing charitable assistance to the sick in the community, and the founder had expressly stated that the way to do this was to remove the patients from society so that others would not be distressed by their condition. In complying with this mission, once the patients were fed and clothed, the hospital's trustees may have thought that other objectives, such as curing disease, were secondary.
- b)
As stated in this private hospital's charter, which remained practically the same throughout the institution's history, auxiliary personnel and senior and assistant nurses were always in charge of care. The role of physicians was limited to delivering a diagnosis—a requisite for admission—and treating concurrent general diseases the inpatients might have or complications that might develop while the tinea was being treated. Although we think these physicians could surely have done much more, the role assigned to them undoubtedly made it difficult for them to dedicate more attention to the health problem that is of interest to us.
- a)
In the translation of treatments, the term pitch plaster refers to either the strips (tiras) or the patches (parches) of pitch (pez) that are used for hair removal. Contemporary instructions in English sometimes referred specifically to combinations of black pitch, resin (in its form exuded from the tree), and spruce (or Burgundy) pitch (possibly also exuded). The senior nurse only specifies a type of pitch twice, however, mentioning black pitch (pez negra) in paragraphs 3 and 5 in the section on treatments. I have used the familiar term tar in both those cases. Paragraph 5 also specifies that the tar should be “from the center” (translated literally); her meaning is somewhat obscure, though we might speculate she means she takes the substance from the middle of a viscous suspension.
The nurse's description of Type 3 tinea includes the word pupulillas, which has never been recorded by dictionary compilers. It is rendered as small black lesions because I assume it is an idiosyncratic derivation from pupa, a word used with and by children to refer to any injury, especially one that leaves a crust.
Finally, in her description of Type 4 tinea, the nurse uses the word pagiza. Pagiza/o is listed by English and French linguists recording Spanish words; they report it being used to denote a thatched hut in the 16th- and early 17th-century (http://ntlle.rae.es/ntlle/SrvltGUILoginNtlle), or to refer to rusticity. I have rendered this as “hut-shaped lesions,” which seems to describe the rounded shape of a kerion. —Mary Ellen Kerans
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Girón F, Lozano C, Serrano-Ortega S. El «Hospital de la Tiña»: Una señera institución granadina (1679-1923). Actas Dermosifiliogr. 2013;106:632–637.