To the Editor:
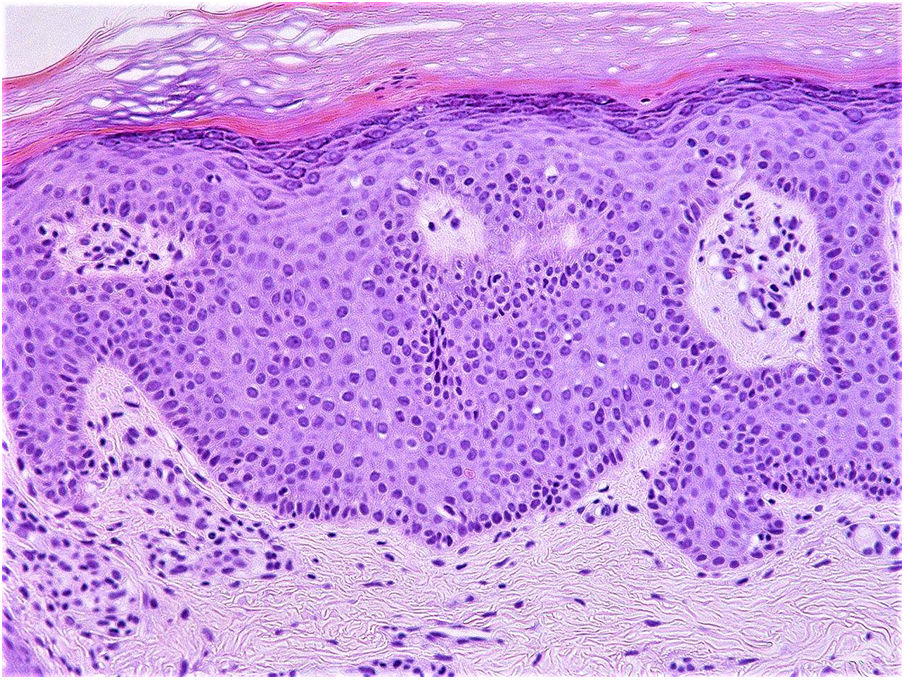
Papular epidermal nevus with “skyline” basal cell layer (PENS) is a variant of epidermal nevus that presents as isolated keratotic papules of variable number and morphology. Histology reveals the following characteristic features: hyperkeratosis; rectangular acanthosis; a palisade basal cell layer; and a wide supranuclear cytoplasmic region that resembles the characteristic “skyline sign” described in Bowen disease. The presence of a wide acellular region just above the nuclei of the basal cell layer is typical.
In 2004 Tadini reported 2 cases of patients with papular epithelial hamartomas with associated neurological abnormalities. These cases were subsequently included in the Atlas of Genodermatosis as new neurocutaneous syndromes.1 However, it was not until 2011 that the acronym PENS was proposed by Torrelo et al. in their series of 5 patients.2
Eight further articles have since have been published, bringing the total number of reported PENS cases to 21, 10 of which involve associated neurological abnormalities. This association of PENS with extracutaneous abnormalities is known as PENS syndrome.
We present 3 new cases of PENS, at least one of which corresponds to PENS syndrome.
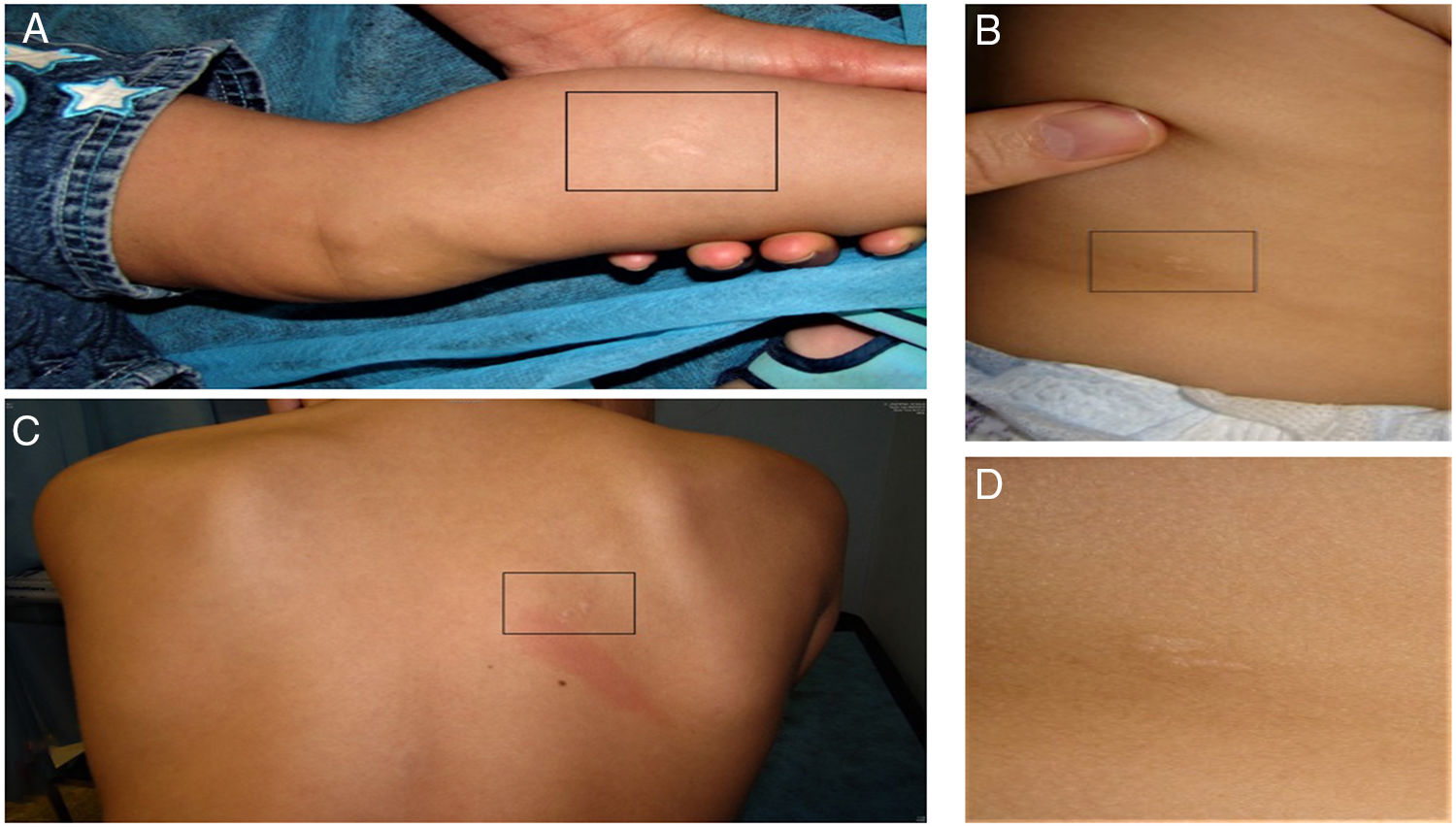
Case DescriptionsCase 1: The patient was a 1-year-old child, with no medical history of interest, who was seen for skin lesions on the limbs that had been present since birth and had remained stable. The lesions were flat, barely noticeable, minimally keratotic papules on the left leg and on both arms (Fig. 1). Magnetic resonance imaging (MRI) revealed expansion of the hydrophilic cavity at the level of the C5–T1 vertebrae. The patient had left torticollis and neurodevelopmental delay predominantly affecting motor, cognitive, and language function (Fig. 2).
Case 2: The patient was a 1-year-old girl with a history of right renal aplasia. She was seen for skin lesions on one arm, the right side, and both legs that her parents had noticed at 1 month of age. The lesions were skin-colored papules without evident associated hyperkeratosis (Fig. 1). Currently, the patient’s psychomotor development is normal.
Case 3: A 9-year-old girl was referred to our department with multiple stable and asymptomatic skin lesions on the trunk and limbs that had been present since birth. The lesions were skin-colored or brownish keratotic papules, many of which were linear, located on the right armpit, right interscapular area, left retroauricular area, left arm and forearm, the back of the left thigh, right pretibial area, and the back of the shoulder (Fig. 1). No other symptoms were reported, apart from tiptoeing in early childhood.
In all 3 cases, a skin biopsy revealed the aforementioned findings characteristic of PENS.
DiscussionWe report 3 new cases of PENS, a recently described entity. Familiarity with PENS is important given the possible association with other anomalies, particularly those affecting neurological function.
In the 3 cases presented here the patients had multiple, widely distributed skin lesions. In 2 of the patients the lesions had been present since birth, as reported in the majority of published cases. Although a likely familial association is described in 2 cases in the literature,3,4 none of the relatives of our 3 patients presented similar lesions.
The association of PENS with extracutaneous abnormalities is known as PENS syndrome, a term proposed at the 23rd meeting of the Spanish Pediatric Dermatology Group in 2012. Our first patient clearly fulfils the criteria for PENS syndrome. Psychomotor delay and mental retardation are features of most of the cases described,5 including those presented here. However, given the young age of our 3 patients, we cannot rule out the potential appearance later in life of other associated neurological conditions such as epilepsy, dyslexia, or attention deficit hyperactivity disorder. An association between PENS and nephrourological malformations (e.g. renal aplasia, as observed in Case 2) had not been previously reported, and it is therefore unclear whether a causal relationship exists. Rodríguez-Díaz et al.6 previously reported an association between PENS and shortening of the Achilles tendon. Although difficult to establish with certainty, this anomaly could account for the tiptoeing in early childhood observed in Case 3.
Because PENS is likely underdiagnosed, knowledge of its presentation and possible associated anomalies is important to ensure correct diagnosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Pardo Domínguez C, et al. Papular epidermal nevus with «skyline»: 3 nuevos casos. Actas Dermosifiliogr. 2020;111:185–187.