The most common causes of generalized interstitial edema are heart failure, chronic kidney disease, and diseases of the liver. Edema, mainly affecting the extremities, is also the initial presenting symptom of scleroderma and other sclerodermiform syndromes. This type of edema is caused by fibrosis of the dermis and in its early stages can be suggestive of other pathologies.1
We describe a patient with a history of mitral valve disease who, while awaiting valve surgery, was admitted for edema of the extremities of several months’ duration and was diagnosed with eosinophilic fasciitis (EF).
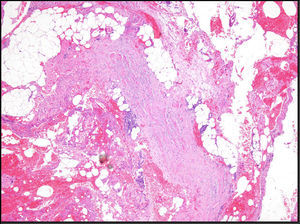
The patient was a 57-year-old man who presented with edema of 3 months’ duration that initially appeared on the lower limbs and subsequently developed on the hands and forearms. His past medical history included diabetes mellitus type 2 and hypercholesterolemia, and he had been diagnosed 6 years earlier with valvular heart disease (mitral valve prolapse) with severe mitral regurgitation. No abnormalities in left ventricular ejection fraction (LVEF) had been observed in cardiological examinations. The patient was admitted based on the suspicion that the edema had been triggered by a first episode of heart failure. He reported no dyspnea, orthopnea, or other related symptoms. Examination revealed a previously identified midsystolic murmur at the apex and hepatomegaly of 2cm. An increase in the diameter of the legs and forearms was also observed, with induration and dimpling of the skin in these areas (Fig. 1), as well as discrete erythema of the legs (Fig. 2). Blood tests showed eosinophilia, a slight elevation in the erythrocyte sedimentation rate (ESR), and hypergammaglobulinemia. All other parameters analyzed were normal. The previous diagnosis of mitral valve prolapse with severe mitral regurgitation was confirmed by transesophageal echocardiography. Left and right heart catheterization showed that both LVEF and pulmonary circuit pressure were normal. Given the contradictory clinical signs and the conflicting results of invasive cardiac tests, the patient was referred to the dermatology department. Given the suspicion of sclerodermiform syndrome a biopsy to the level of the muscular fascia was performed. The biopsy showed thickening and edema of the subcutaneous septa. The subcutaneous septa and superficial fascia contained a mild inflammatory infiltrate composed of lymphocytes, histiocytes, plasma cells, and eosinophils. The dermis and epidermis were intact (Fig. 3). Based on the diagnosis of EF the patient began prednisone treatment (60mg/d), to which methotrexate was later added, resulting in clinical improvement and normalization of blood parameters. The patient is currently being treated with hydroxychloroquine and has a good quality of life, with no impairment of mobility and no change in valvular heart disease status.
EF is a sclerodermiform syndrome that was first described by Shulman2 in 1974. It is characterized by an initial phase of edema, erythema, and thickening of the skin, with symmetrical involvement of the extremities, although it can also affect the trunk and neck. After this initial phase the skin and subcutaneous tissue becomes indurated and the skin acquires an orange-peel-like appearance. EF can also present as morphea-like skin lesions; these 2 entities have been linked in various studies.3,4 It can also be associated with extracutaneous manifestations such as arthritis, joint stiffness, carpal tunnel syndrome, and muscle weakness. There have been isolated reports of systemic or visceral involvement. EF has been linked to blood disorders such as aplastic anemia, autoimmune anemia and thrombocytopenia, and lymphoproliferative diseases (lymphoma and multiple myeloma). It is accompanied by peripheral blood eosinophilia (up to 80%-90% of cases, depending on the series), increased ESR, and hypergammaglobulinemia, although the absence of any of these symptoms does not rule out the presence of the disease. While the etiology of EF is unknown, it has been associated with a history of intense exercise, trauma,5Borrelia burgdorferi infection, and the use of drugs, such as simvastatin.6,7 Confirmatory diagnosis is established by histological analysis of the skin, including the superficial muscle fascia. The following signs are typical: thickening of the septa of the subcutaneous tissue and of the fascia, which contain an inflammatory infiltrate of variable intensity that consists of lymphocytes, plasma cells, and occasionally eosinophils (the presence of which is not required for diagnosis) and is associated with dermal fibrosis. Recent studies have described the usefulness of magnetic resonance imaging in diagnosing and monitoring the progression of EF.5,8,9 The differential diagnosis includes eosinophilia-myalgia syndrome, morphea, systemic scleroderma, and other sclerodermiform syndromes. As in the present case, the initial edema can be suggestive of other edema-causing conditions. Early treatment is essential to preserve mobility. The drugs of choice are oral corticosteroids, although hydroxychloroquine, methotrexate, and other immunosuppressive agents have also been used in isolated cases. Three predictors of treatment resistance have been identified: the presence of morphea-like skin lesions; early disease onset (patients under 12 years); and trunk involvement.4,10
We have reported a case of EF, a rare entity that presents diagnostic challenges and requires multidisciplinary management. Nondermatologist specialists should be familiar with the initial clinical features of this condition, including edema and erythema, in order to either rule out the disease or avoid delays in diagnosis, which can lead to further complications.
Please cite this article as: Utrera-Busquets M, Tardio J, Curcio-Ruigomez A, Borbujo-Martínez J. Fascitis eosinofílica: causa infrecuente de edemas. Actas Dermosifiliogr. 2014;105:626–628.