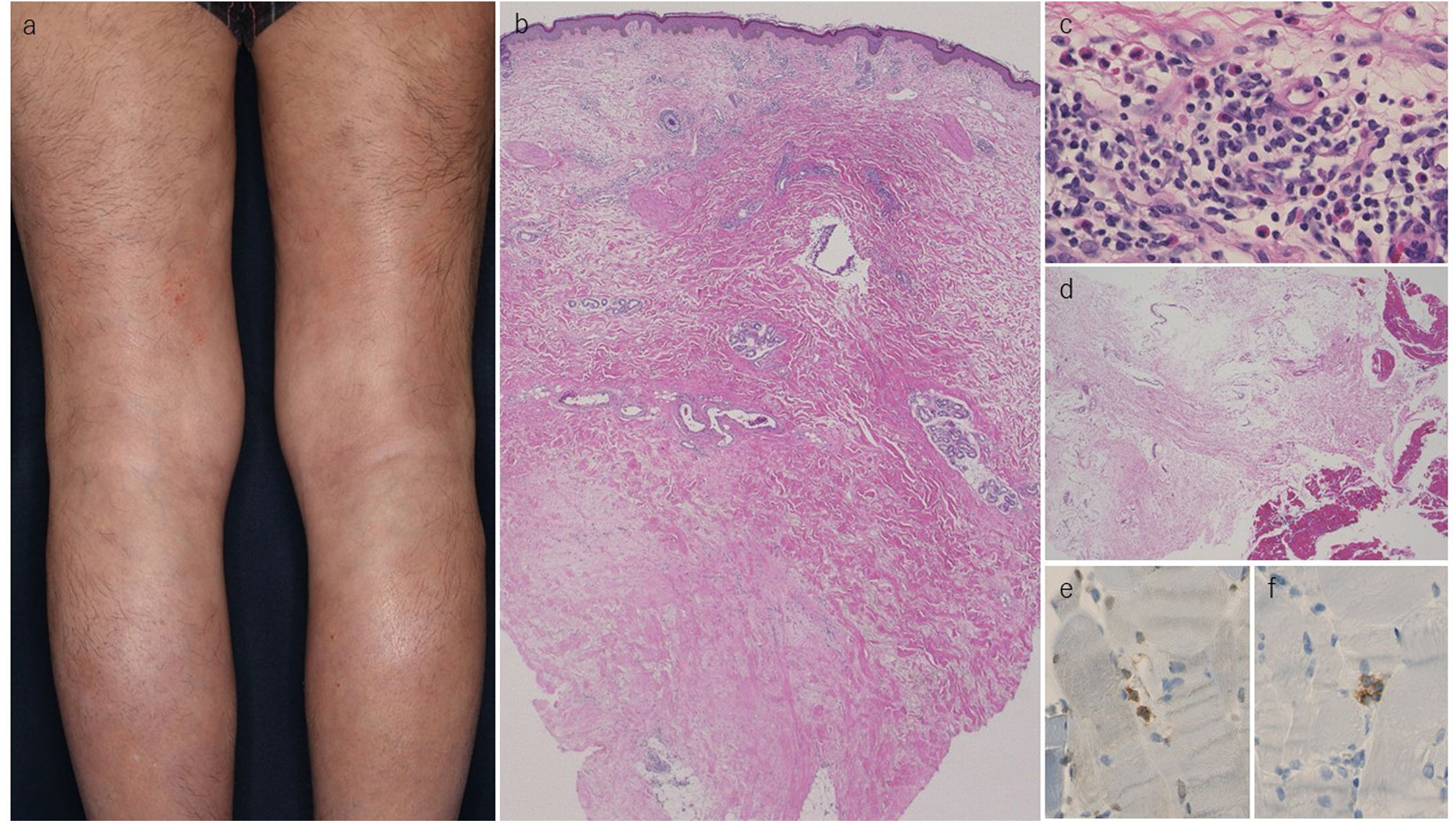
A 69-year-old male was admitted to the surgery department for cholangiocarcinoma (stage IIIB (pT2a, pN1, M0)). After surgery, chemotherapy with gemcitabine (600mg/body) was started with every two weeks’ administration for 13 months. Around the end of the chemotherapy schedule, he developed skin hardening of the lower extremities with pruritus, and was referred to the dermatology department. Gemcitabine administration was over one month before the initial visit to us. Physical examination showed severely hardened brownish skin on the bilateral lower extremities (Fig. 1a), although the upper extremities were not affected. Neither sclerodactyly nor Raynaud's phenomenon was recognized. Laboratory examination showed an elevated eosinophil (9.1%) and C-reactive protein (3.93mg/dl). A biopsy specimen revealed perivascular infiltration of mononuclear cells and eosinophils in the upper dermis, as well as thickened collagen bundles in the mid- to lower dermis (Fig. 1b, c). There was small number of inflammatory infiltrates of mononuclear cells and eosinophils in the thickened fascia (Fig. 1d), and few CD4- and CD8-positive T-cells were present in the muscle tissue (Fig. 1e, f). Topical corticosteroid ointment was administered for pruritus. Skin sclerosis was gradually improved over three months, and the sclerotic skin returned to normal within six months. Peripheral eosinophils also returned to normal. Thereafter, he has been followed for two years without recurrence of either cholangiocarcinoma or skin hardening of the lower extremities.
(a) Wood-like hardening of the bilateral lower extremities. (b) Histological features showing diffuse dermal sclerosis, thickened fibrous septal connective tissues with mononuclear cells infiltration in the subcutaneous tissues. (c) Higher magnification showed perivascular infiltration containing a number of eosinophils in the upper dermis. (d) Small number of cellular infiltrates of mononuclear cells in the thickened fascia. CD4- (e) and CD8- (f) positive T-cells in the muscle tissues. (Magnification, b: ×40, c: ×400, d: ×200, e: ×400, f: ×400).
The presented patient developed severe hardening of the lower extremities during hospitalization for cholangiocarcinoma. Systemic prednisolone was not administered, because the patient suffered from nephritic syndrome and his doctor did not want to use oral corticosteroids due to the risk of infection. Initially, paraneoplastic eosinophilic fasciitis was suspected, but the patient's clinical course was atypical and the severe skin hardening gradually improved almost completely after the end of chemotherapy, without systemic prednisolone or any additional therapies. The medications were reviewed in detail, which confirmed that gemcitabine was administered as a postoperative chemotherapy, and that the skin hardening began to appear around the end of the chemotherapy schedule. Additionally, histopathological features showed sclerosis of the dermis, subcutaneous tissue, and fascia. Eosinophil infiltration was observed in the upper dermis, whereas scarcely detected in the thickened fascia. Those characteristics and the clinical course in the present case were inconsistent with typical eosinophilic fasciitis. Certain anti-cancer drugs such as taxane, paclitaxel, carboplatin, balicatib, and mitomycin C, evoke symptoms that resembles scleroderma, in which the lower limbs are predominantly affected. Gemcitabine is a chemotherapeutic agent used for various malignancies, and a few cases of gemcitabine-induced scleroderma-like changes or lipodermatosclerosis-like lesions have been reported.1–4 The intervals until the onset of scleroderma-like changes vary between 1 week and 1 year. It has been suggested that locoregional toxicity due to accumulation of gemcitabine or its metabolites in the subcutaneous tissues might be responsible for triggering sclerotic lesions. Alternatively, chemotherapeutic agents may promote DNA damage signals, which induces cutaneous fibrosis via increased production of type I interferon and interleukin-6.5 Although paraneoplastic eosinophilic fasciitis is sometimes reported, we should pay attention to the use of chemotherapy drugs as a triggering factor of skin hardening, if we see cancer-bearing patients.