We read with interest the article “Molluscum Contagiosum on the Palms: An Uncommon Location”.1 The authors describe an adult male with 2 molluscum contagiosum (MC) lesions on the right hand and perform a review of the literature of reported cases of palmoplantar MC.
We report the clinical findings and dermoscopic characteristics of a new case of plantar MC seen recently in a 10-year-old girl, with no past history of interest, who visited our department with stable asymptomatic lesions on the right foot that had appeared 4 months earlier. The patient did not recall having suffered any local trauma and had not undergone prior treatment. She used a swimming pool twice a week and had a personal history of plantar hyperhidrosis and atopic diathesis, with several episodes of dyshidrotic eczema and juvenile plantar dermatitis in the past 3 years.
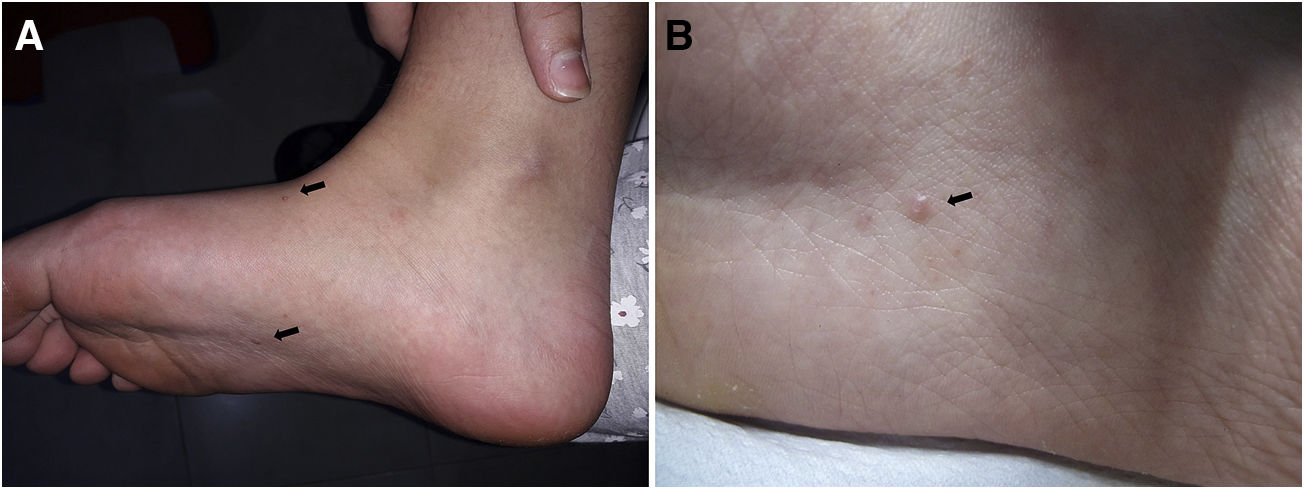
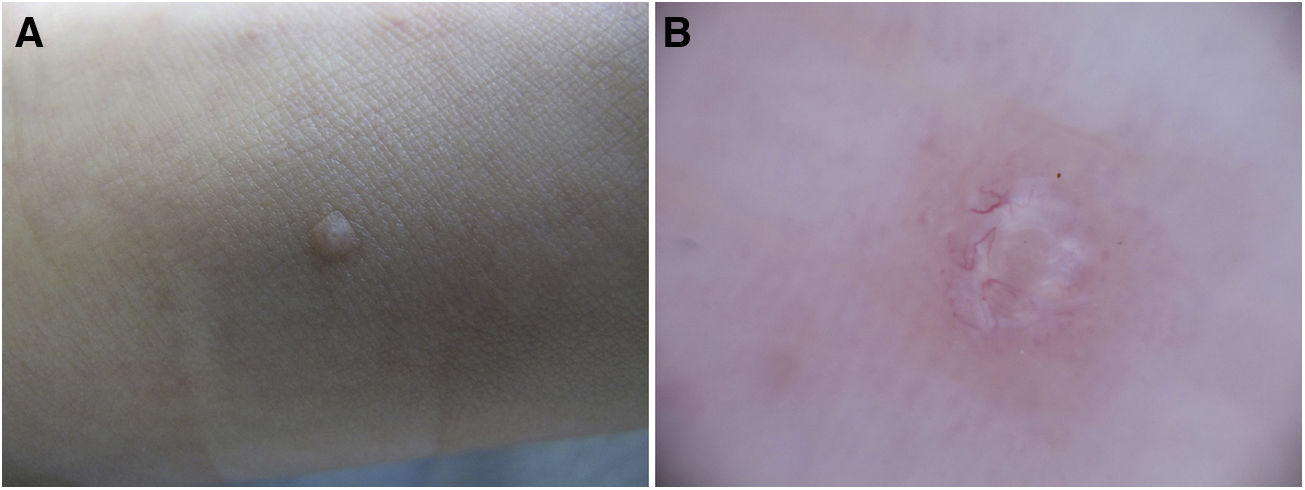
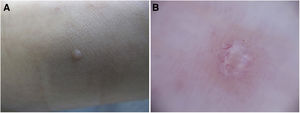
The dermatologic examination revealed 2 dome-shaped erythematous papules with an umbilicated center measuring 2 mm in diameter, located on the instep and sole of the right foot (Figs. 1 and 2A). Dermoscopy revealed a yellowish round central structure and branching vessels in a crown distribution on the periphery (Fig. 2B).
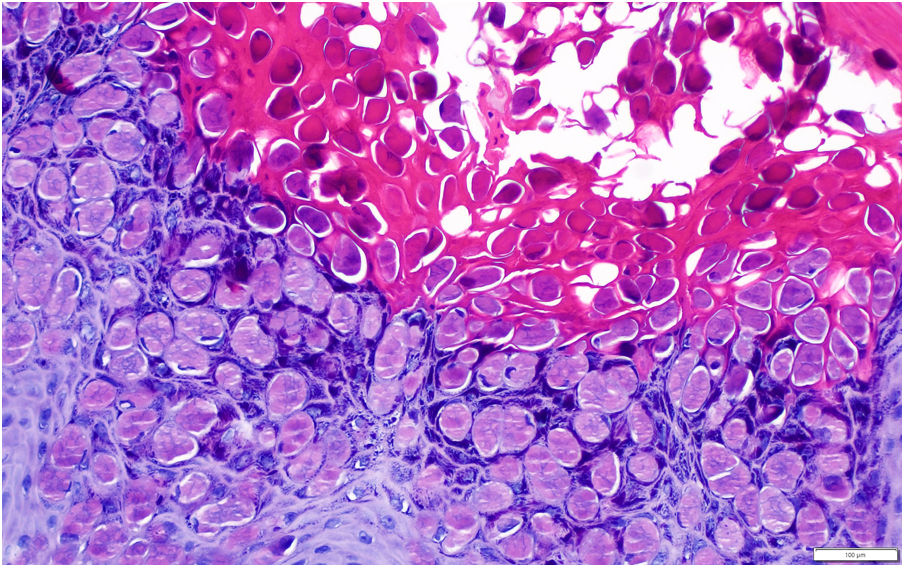
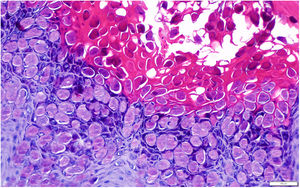
The lesions were treated with curettage and histopathology confirmed the suspected diagnosis of MC. The lesion was revealed to be nodular in the form of endophytic lobules with a squamous epithelium with molluscum bodies maturing toward the surface (Fig. 3).
MC is a very common skin infection caused by the poxvirus Molluscum contagiosum. Transmission is by direct contact, fomites, or autoinoculation. It usually manifests as dome-shaped umbilicated papules that are whiteish or the same color as normal skin, measuring between 3 and 5 mm in diameter, and generally asymptomatic.2
It mainly affects 3 population groups: children, sexually active adults, and immunosuppressed persons. In children, MC lesions tend to be found on the torso and extremities, whereas in adults, they usually present in the genital region, lower part of the abdomen, pubis, and proximal surface of the thighs.2,3 Regardless of age, subungual or interdigital involvement, or involvement of the conjunctival and oral mucosa and of the palmoplantar region is exceptional. Atypical clinical presentations (giant forms), extensive lesions, lesions on the face and neck, or other uncommon locations tend to occur particularly in the context of immunosuppression.4,5
The clinical diagnosis of plantar MC is more difficult, as the lesions tend to lack the usual clinical characteristics (they rarely present as umbilicate papules with a central keratin plug).6 They present as single or multiple papules or nodules with varying coloration (normal skin, erythematous, brownish, translucent, or yellowish) and with a hyperkeratotic, verrucous, or crusted surface. Most patients have only 1 giant lesion (≥ 1 cm in diameter), that is painful on walking.1,7
While infection with the MC virus is more frequent in childhood and in atypical locations in immunocompromised patients, most cases of palmoplantar involvement have been reported in immunocompetent adults. It may be that the thickness of the stratum corneum on the palms and soles makes entry of the poxvirus more difficult (it is much larger than the human papilloma virus). Moreover, local trauma and plantar hyperhidrosis may be predisposing factors.1
The differential diagnosis of plantar MC is broad and includes plantar warts, plantar corns, pyogenic granuloma, foreign body granuloma, epidermal cyst, Spitz nevus, and eccrine poroma. Treatment is the same as that used in other locations.5,7
The typical dermoscopic pattern of MC consists of a central round, amorphous structure (sometimes polylobar, in the form of a four-leaf clover, nonspecific, or even nonvisible) with a white or yellowish color, and blood vessels with a crown distribution (less frequently, radial, punctate, or mixed-pattern vessels), with a radial distribution in the periphery of the lesion. The whiteish central structure correlates histologically with the inverted lobules of the acanthotic epidermis (filled with Molluscum bodies), which expand as the infection advances, moving the dermis and, therefore, the vessels contained in it, to the periphery of the lesion.8,9 We have found only 1 article that describes the dermoscopic findings of plantar MC; those authors describe a yellowish destructured central area surrounded by thick branching vessels with bulbous terminations.10
In conclusion, we report MC with typical clinical signs on the sole of the foot of a girl who frequents a swimming pool. We believe that the history of plantar skin lesions in the context of the patient’s atopy (juvenile plantar dermatitis and dyshidrosis) and her hyperhidrosis may have contributed to the appearance of MC in that location.
FundingThis study has not received funding of any kind.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Monteagudo Sánchez B, León-Muiños E, Piñeyro-Molina F, Vázquez-Bueno JÁ. Dermatoscopia de un molusco contagioso plantar. Actas Dermosifiliogr. 2021;112:963–965.