A 3-day-old newborn who was born at full term and had no past history of interest was evaluated for the presence of a congenital lesion on the vertex. Examination revealed a 9-mm, skin-colored pedunculated papule located on the midline (Fig. 1).
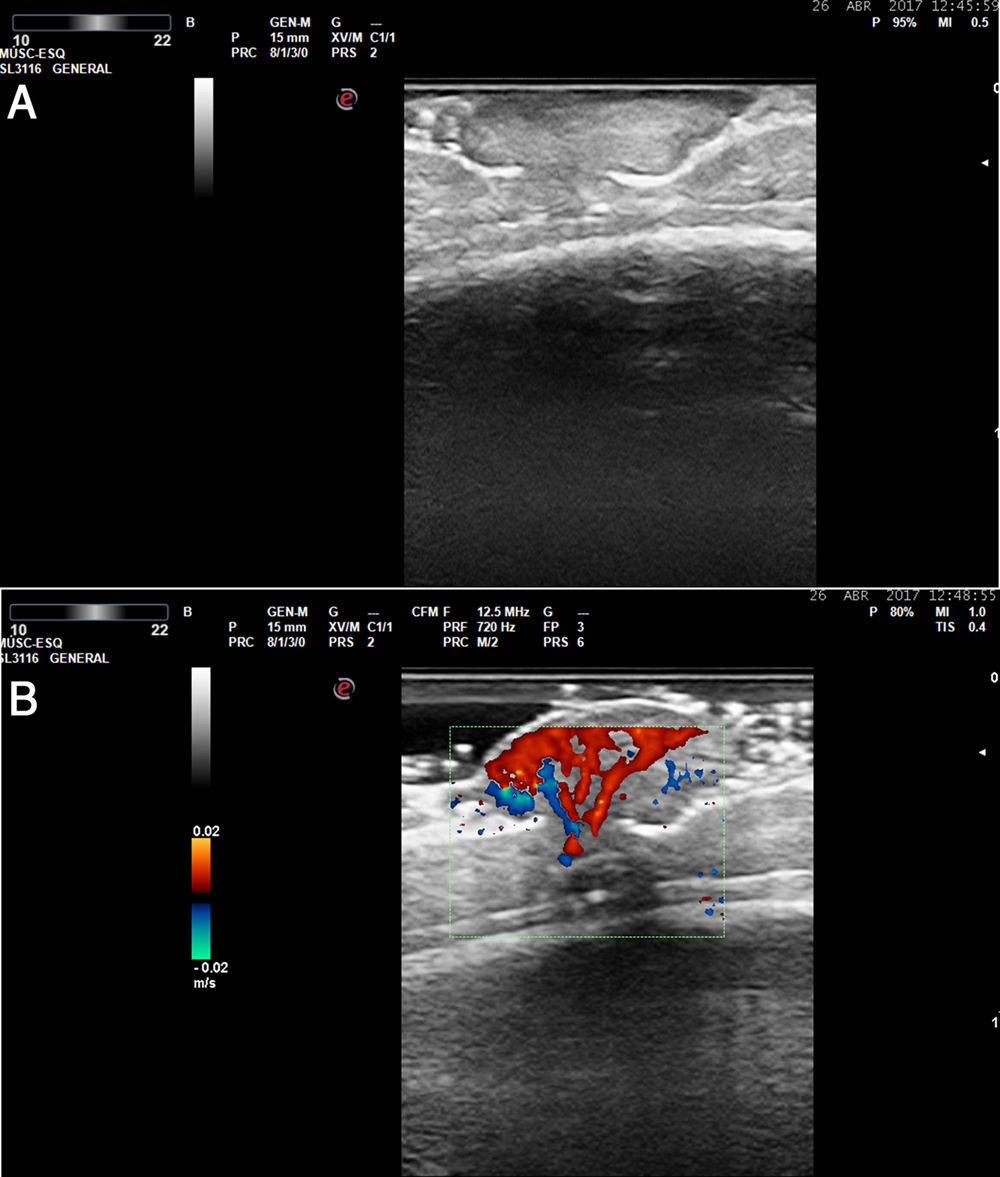
Skin ultrasound was performed with an Esaote Gamma MyLab system with a variable frequency (10–22 MHz) probe. B-mode ultrasound revealed a well-defined hyperechoic dermoepidermal lesion that had a lobulated lower contour and did not affect the calvaria (Fig. 2A). Abundant vascularization was observed in color Doppler mode (Fig. 2B). In the absence of calvarial involvement and intracranial invasion, tangential excision of the lesion and electrocoagulation of the bed was performed to rule out malignancy and the presence of a vascular lesion.
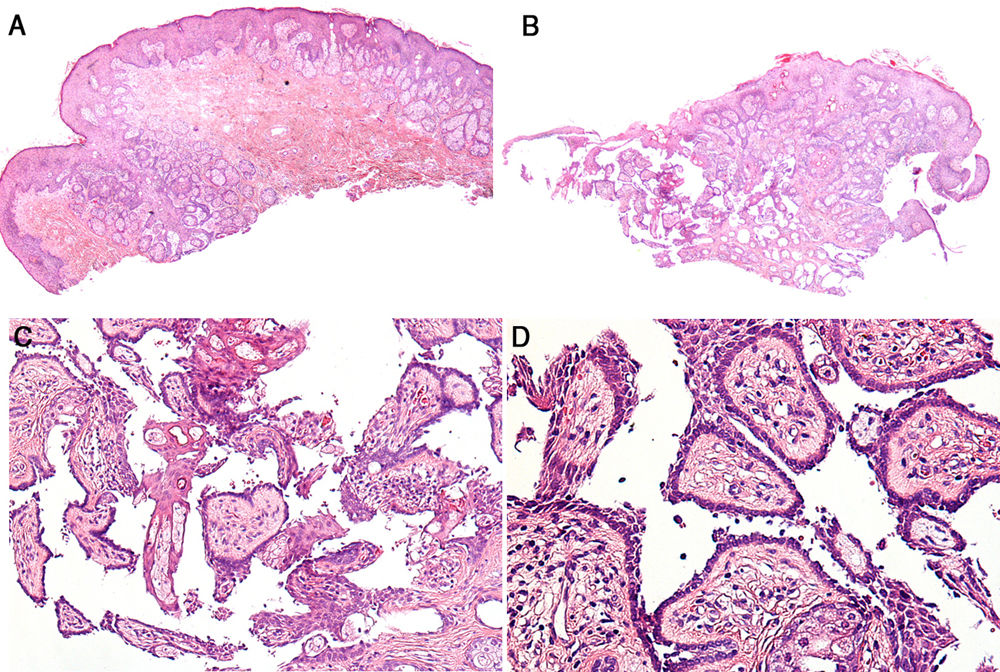
Histology showed multiple sebaceous glands in the papillary dermis beneath a preserved epidermis (Fig. 3A). Examination of successive sections revealed a lesion composed of papillary structures connected to the follicular infundibulum (Fig. 3B). These papillary structures were lined with a row of columnar epithelial cells that showed evidence of decapitation secretion at the luminal border, and the stroma of the papillae contained numerous plasma cells (Fig. 3C and D).
What Is Your Diagnosis?
DiagnosisSyringocystadenoma papilliferum.
CommentsA diagnosis of syringocystadenoma papilliferum was established. This is a benign adnexal hamartoma with follicular and apocrine differentiation.1 Up to 50% of these lesions are congenital and can go unnoticed until adolescence, at which point hormonal stimulation promotes their growth and they tend to become more evident. During this growth phase they can ulcerate and bleed in response to trauma. The differential diagnosis of the congenital ulcerated form should include traumatic birth injury.2 Between 70% and 90% of cases occur in the cervicocephalic region, although involvement of other areas has been described in pediatric patients.3 Three clinical forms can be distinguished: papular (single papule or plaque on the scalp, most frequently associated with sebaceous nevus); linear (multiple umbilicated papules of similar size, most often in the cervical region); and nodular (the most common extracephalic subtype).
Syringocystadenoma papilliferum is one of the lesions that most frequently develops from Jadassohn nevus; 75% of syringocystadenoma papilliferum cases arise from this nevus type. A review of the literature reveals that multiple benign and malignant neoplasms can develop from pre-existing Jadassohn nevus, including tricholemoma, trichoblastoma, sebaceoma, apocrine adenoma, basal cell carcinoma, squamous cell carcinoma, verrucous carcinoma, ductal carcinoma, and syringocystadenoma papilliferum.4
The main peculiarity of our patient’s lesion was the papillary epithelial lining, which consisted of a single row of cells and exhibited discrete signs of decapitation secretion, as opposed to the classic double-row arrangement of epithelial cells showing evidence of decapitation secretion at the luminal border. This may be because the patient was a newborn, and therefore the lesion was in the initial stages of development and not highly differentiated.
In such cases ultrasound plays an important role as it can help establish the size and depth of the lesion, as well as its relationship with adjacent structures. In this specific case ultrasound allowed us to rule out cranial involvement.
We have found no previous descriptions in the literature of the ultrasound pattern of syringocystadenoma papilliferum. A marked increase in vascularization is also observed in other benign adnexal proliferations. The correlation between this feature and the histopathological findings is unclear.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Torre Castro J, Mendoza Cembranos MD, Requena Caballero L. Una lesión congénita en el cuero cabelludo. Actas Dermosifiliogr. 2021;112:257–258.