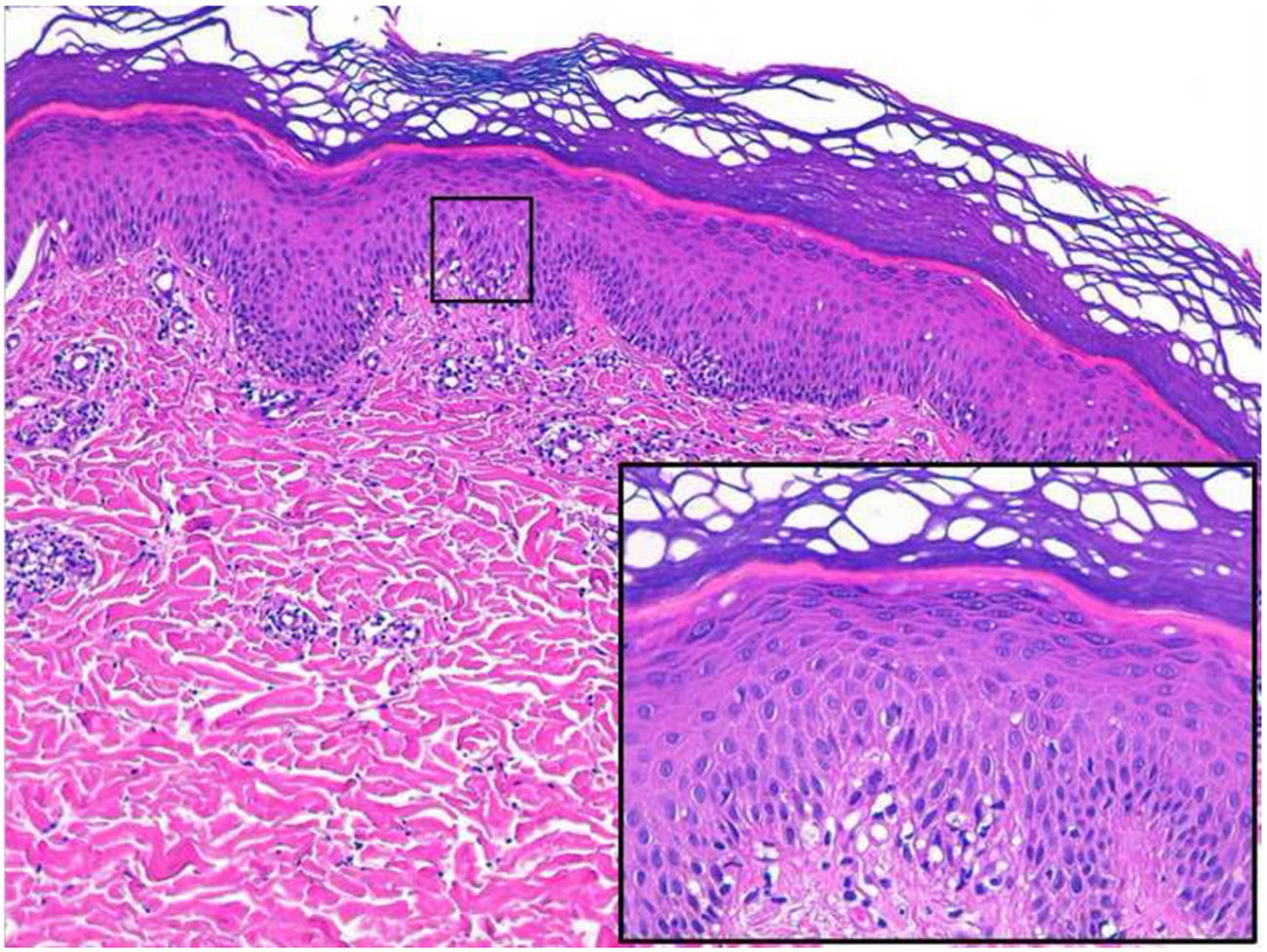
A 26-year-old man with no relevant history was seen at the emergency department for asymptomatic palmoplantar lesions that had appeared 3 weeks earlier and had not responded to topical prednicarbate treatment (twice daily for 20 days). The patient reported no fever or systemic symptoms. He had no history of oral or genital ulcers in the preceding weeks or months, and reported no risky sexual relations. Physical examination revealed erythematous oval plaques, some of which showed fine collarette scaling, located on the palms (Fig. 1), soles, and lateral aspects of the feet (Fig. 2). Histology showed superficial lymphocytic perivascular dermatitis with minimal epidermal exocytosis associated with mild spongiosis (Fig. 3). Immunohistochemistry for Treponema pallidum was negative. Serological screening using chemiluminescence immunoassay to detect total antibodies against T pallidum was initially negative. Screening was repeated 1 month later, together with visually interpreted treponemal and non-treponemal tests (T pallidum hemagglutination assay [TPHA] and rapid plasma reagin [RPR] tests), all of which were negative. The lesions resolved without treatment after 4 weeks, and the patient remained free of lesions during follow-up, which ended when he again tested negative in a T pallidum screening test 3 months after lesion resolution. Based on the clinical course and the clinical, histological, and laboratory data, a diagnosis of atypical palmoplantar pityriasis rosea (PR) was established.
PR is a common entity that mainly affects adolescents and young adults: 75% of cases are diagnosed between the ages of 10 and 35.1 Clinically, it presents as a papulosquamous eruption with a self-limiting course, distributed mainly on the trunk and the proximal aspect of the extremities, following the Langer lines. These lesions are usually preceded by a larger scaly lesion called a herald patch, and some patients may report prior flu-like symptoms.1 The literature includes infrequent reports of atypical forms, characterized by lesions that are morphologically distinct or appear in other locations. These atypical forms include vesicular, purpuric, inverse, unilateral, and palmoplantar PR. Palmoplantar involvement in PR is very rare, and very few cases are described in the literature. In some such cases the palms and soles are affected in the context of a more typical eruption on the trunk.2,3 Others consist of palmoplantar involvement in the form of vesicular lesions,4 or of more typical, exclusively palmoplantar lesions.5 We consider our case to correspond to the latter group, diagnosis of which can be difficult to establish. In all cases of PR with palmoplantar involvement the main differential diagnosis is secondary syphilis. For this reason, serological and histological approaches were used to rule out secondary syphilis in our patient and help establish diagnosis. Histology of PR is nonspecific. In our patient biopsy revealed findings that could be considered compatible with an eczematous process. However, given the clinical appearance of the lesions, the absence of pruritus, and the resolution without treatment, this entity was excluded from the differential diagnosis.
Treatment of PR is controversial. Some data support treatment with erythromycin.6 However, given the natural course of the disease alternative options include symptomatic treatment of pruritus with topical corticosteroids or oral antihistamines and therapeutic abstention, which was selected in the present case.
We present a case compatible with palmoplantar PR, a rare variant of PR of which very few cases are described in the literature. Despite their infrequent nature, atypical variants of PR can simulate other conditions, and therefore knowledge of these entities is of the utmost importance.
Please cite this article as: Martín-Alcalde J, Elosua-González M, Pinedo-Moraleda FJ, López-Estebaranz JL. Pitiriasis rosada atípica palmoplantar. Actas Dermosifiliogr. 2021;112:372–374.