Pachydermodactyly (PDD) is a benign, rare acquired digital fibromatosis around proximal interphalangeal (PIP) joints. Current therapies include local infiltration with triamcinolone acetonide or surgical excision. We report a patient treated successfully with surgical CO2 laser.
PDD was described by Bazex in 1973, although the term was coined by Verbov in 1975.1 It presents as symmetrical soft tissue swelling on the sides of PIP joints of second, third and fourth fingers. Lesions appear insidiously in puberty and they are four times more frequent in males.
Etiology is unknown, but it has been related to repetitive trauma, psychiatric disorders and systemic diseases as tuberous sclerosis or Ehlers-Danlos syndrome.2
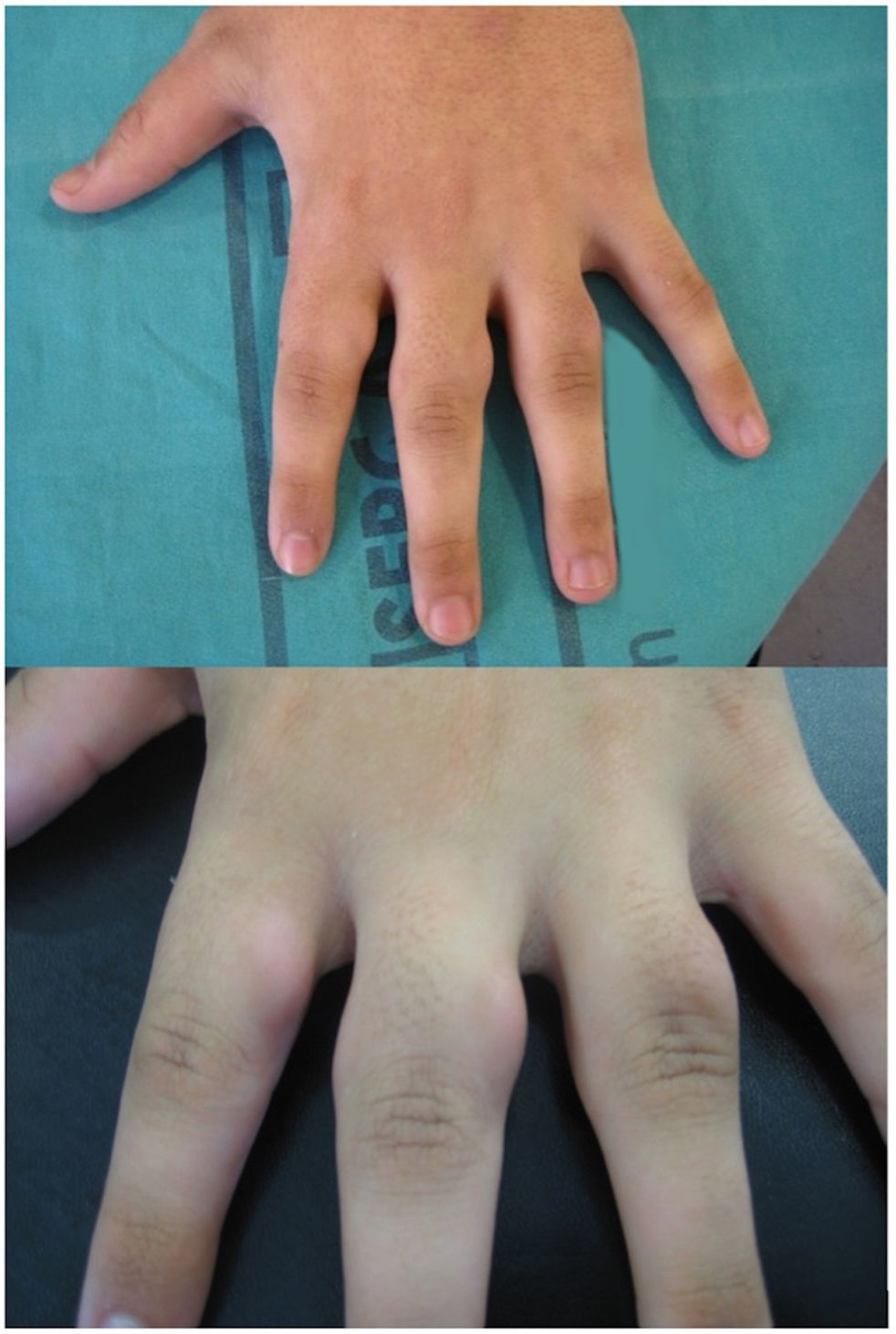
A 17-year-old male presented with a 6-year history of asymptomatic PIP joints thickening (Fig. 1). No morning stiffness, pain or other systemic manifestations were reported. He denied any mechanical trauma. Blood tests including rheumatoid factor, antinuclear antibody and C-reactive protein were negative. X-ray showed soft tissue swelling.
A skin biopsy was performed, and it revealed hyperkeratosis, dermal collagen accumulation and decreased elastic fibers. Additionally, a small amount of mucin was evidenced in the dermis. The lack of symptoms and other signs of systemic diseases led to the diagnosis of PDD.
Given the psychological impact, therapeutic intervention was decided.
Under local anesthetic, using CO2 laser (SE-20–30w Franckline; Intermedic, Barcelona, Spain), a 5mm incision was made with superpulsed focused mode (beam diameter 1mm) and 5W power density. Once the plane of dissection between dermis and subcutaneous tissue was reached, we vaporized the thickened tissue with the same energy, but defocused mode. This was done while pulling the skin with an Adson tweezer and moving the laser in a circumferential manner, always staying parallel to the finger in order to avoid extending into deeper planes where the neurovascular bundle is located. This will guarantee that the treated area is mainly the dermo-hypodermal junction.
Treatment was split into 4 sessions 1 month apart treating 2–3 fingers each time to minimize postoperative morbidity.
Secondary intention wound healing does not need special follow up. Domiciliary daily wound-care was indicated for 2 weeks: cleaning with a mild soap and water, followed by the application of mupirocin ointment 2% and covering with a dressing.
An excellent cosmetic and functional outcome was achieved (Fig. 2). Post inflammatory hyperpigmentation (PIH) was the only adverse effect and it decreased in the following months without any treatment. No recurrence was detected.
PDD is a benign and usually asymptomatic entity. A recent systematic review concluded its typical presentation occurs in young men with no family history, affecting PIP joints bilaterally.2
Skin biopsy is not specific, and its utility resides in distinguishing from inflammatory diseases and other fibromatosis such as knuckle pads.
PDD may reverse with discontinuation of mechanical stimulation, and most cases do not require any treatment. Psychotherapy may be useful in patients with compulsive behavior.3
Therapy intervention is indicated when lesions are painful or cause functional or esthetic problem. Intralesional corticosteroid infiltration is the most used method.4 It is well-tolerated and inexpensive, but it also can produce lipoatrophy or vascular and tendon structures damage. In addition, this technique usually needs cessation of mechanical trauma to achieve long-term results.
When comparing surgery to laser, we find that both present the same theorical risks, since they are invasive procedures that could damage tendon, vascular and nervous structures. Surgery also requires suture and presents an increased cost and operative duration.5 Laser treatment induces more fibrosis than surgery, which is a beneficial side effect as it helps avoiding recurrence of lesions. PIH is a frequent, but minor side effect considering it improves over time even with no treatment.
Alternative methods such us occlusion of potent topical steroids show non-conclusive results. Oral tranilast was described to be effective in one case report.6
To our knowledge, this is the first report of the use of CO2 laser in PDD. Given the positive experience and the cost-effectiveness, we propose that vaporization with CO2 laser may be considered as an alternative therapeutic approach of PDD. Possible complications would be the damage to the neurovascular bundle, that is minimized by staying superficial and parallel to the finger when vaporizing the tissue. Ablation with CO2 laser offers some advantages that could make it also useful in similar entities such as knuckle pads and pseudo-knuckle pads, although more evidence is needed to support this statement.
Conflict of interestThe authors declare that they have no conflict of interest.