Lymphangioma-like Kaposi sarcoma (LLKS) is a rare histologic variant of Kaposi sarcoma that can present as any of the 4known clinical variants. LLKS is a vascular neoplasm that develops secondary to infection by human herpesvirus type 8 (HHV-8), which is also known as the Kaposi sarcoma virus. Clinically, it can present with the usual manifestations, namely, patches, plaques, or nodules. However, in some cases, it presents as blisters that may be confused with bullous skin disease.
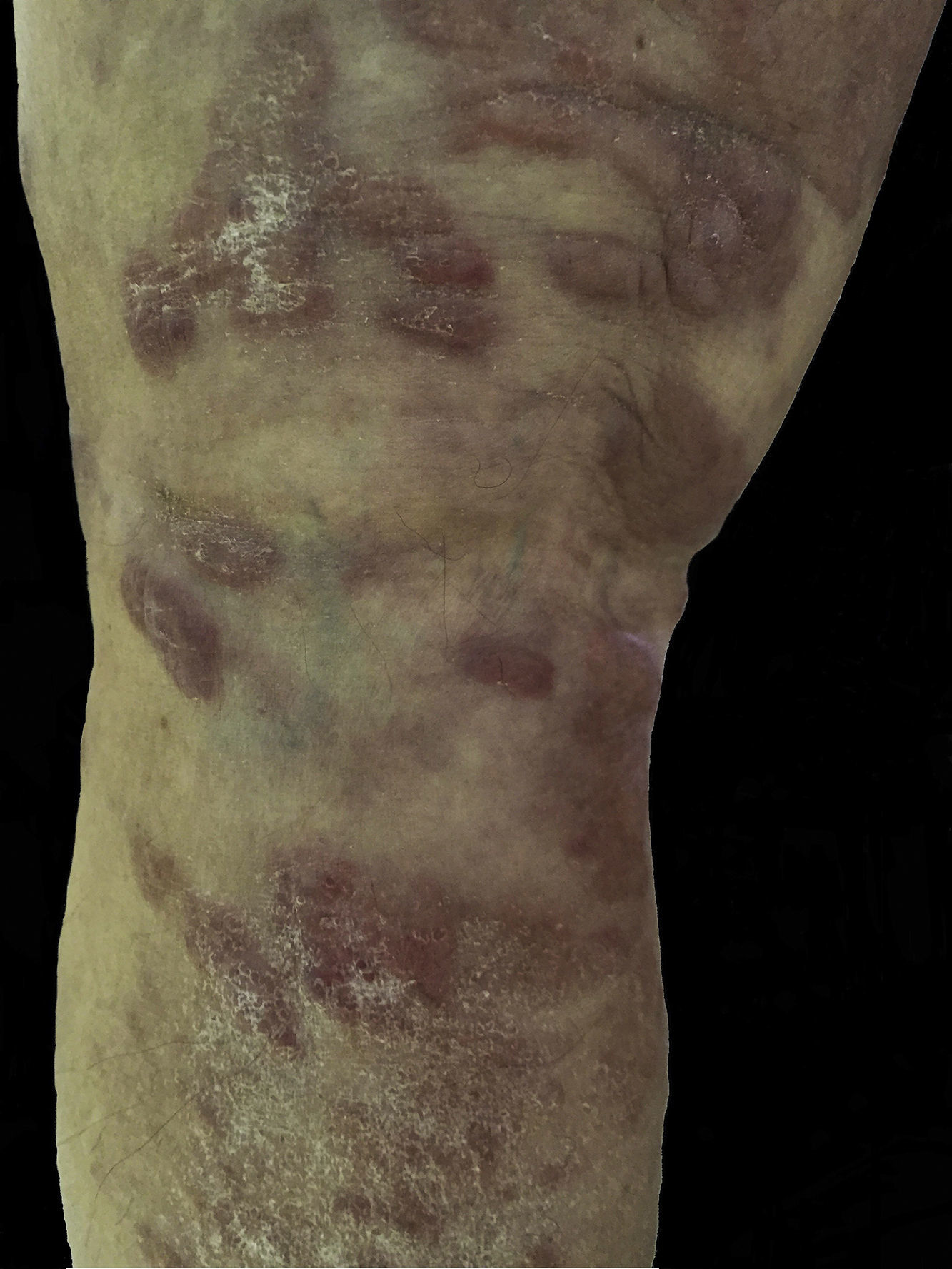
Case DescriptionThe patient was an 80-year-old man whose history was unremarkable. He presented with raised erythematous, oval plaques measuring 1-3cm in diameter that had first appeared 5 years previously. The plaques occasionally coalesced and were found on the upper and lower limbs and lower back. The lesions had gradually increased in number and size, although they were neither painful nor pruriginous. The physical examination revealed flaccid blisters (1cm) containing serum (Fig. 1). Treatment with various topical options had been unsuccessful.
A complete laboratory workup including complete blood count and biochemistry revealed iron-deficiency anemia. Serology testing for HIV was negative.
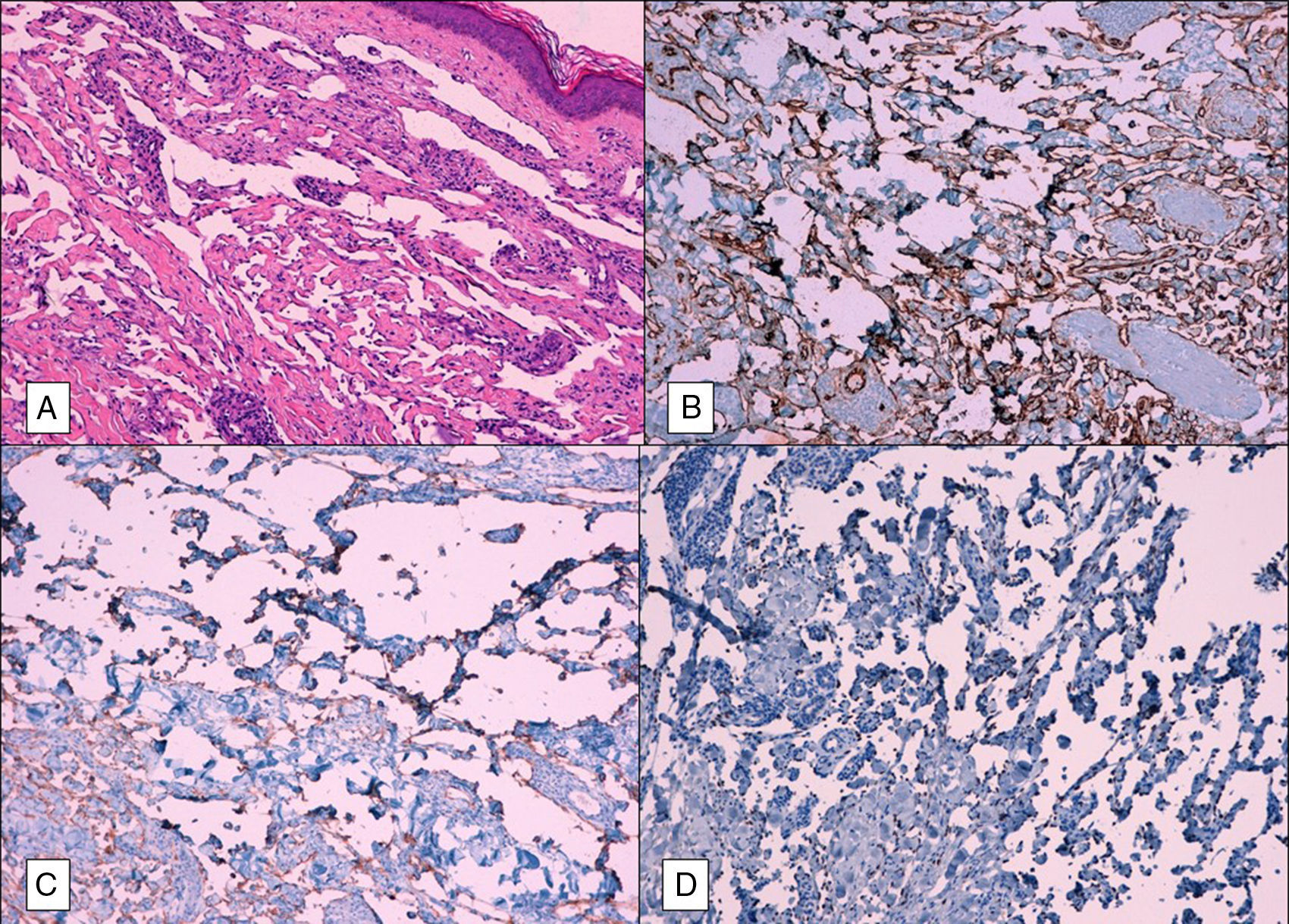
Histopathology revealed that the epidermis was conserved and highlighted a proliferation of anastomosed vascular spaces that occupied the complete thickness of the dermis, dissected the collagen bundles, and surrounded cutaneous muscles and adnexa. No blood was identified in these structures. Clusters of lymphocytes and plasma cells were common in the stroma. Closer examination revealed that the vascular channels were lined with a layer of flattened endothelial cells and that there was no atypia or mitosis. Immunohistochemistry showed that tumor proliferation was positive for the endothelial markers CD31 and CD34 and for the lymphatic marker D2-40. It also showed clear nuclear staining for latent nuclear antigen 1 of HHV-8 (Fig. 2).
The patient was diagnosed with LLKS and referred to the medical oncology department. Given the poorly aggressive clinical course and the patient's age, it was decided—after evaluation and with the patient's agreement—to adopt a wait-and-see approach.
DiscussionLLKS is a malignant vascular neoplasm with evidence of lymph and blood vessel differentiation. It is a rare histologic variant of Kaposi sarcoma (5% of cases)1 and can present in any of the 4existing epidemiologic variants. Etiology and pathogenesis are controversial, as is the question of whether the disease should be classified as reactive or neoplastic.2 The discovery of HHV-8, which is present in 100% of cases of Kaposi sarcoma, irrespective of the subtype in question, is a major finding in our knowledge of the etiology and pathogenesis of the condition.3 Similarly, the question of cell differentiation is controversial, since cells express both specific blood and lymph markers.4,5
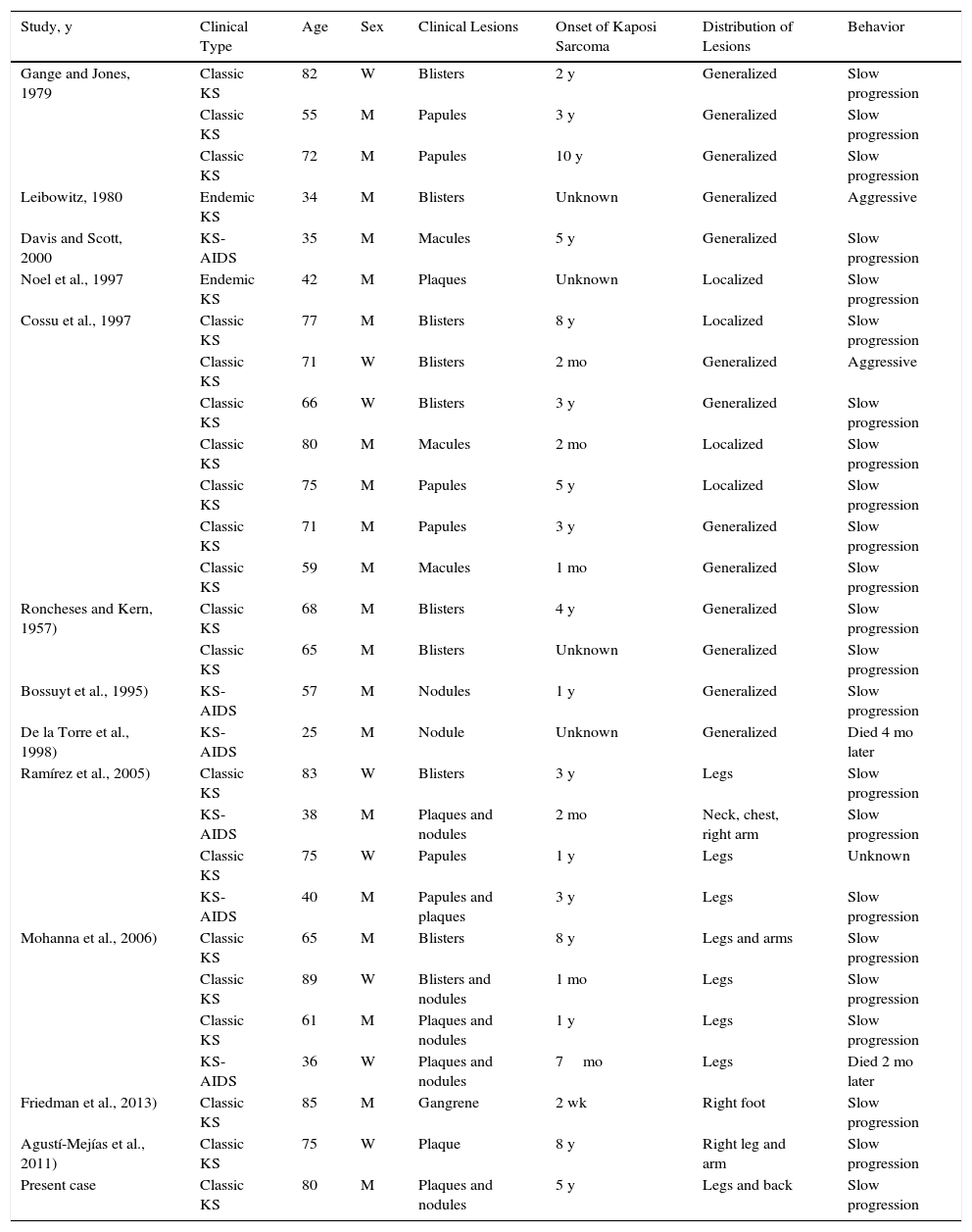
Clinical ManifestationsThe most common presentation of LLKS is blisters,6 although it can also appear in the more classic form of plaques or nodules. LLKS can also present as a mucocutaneous lesion, affecting mainly the legs and arms. The condition is more common in males, with a mean age at onset of 45.1 years (Table 1). Despite the low number of cases reported in the literature, data seem to indicate that LLKS is more indolent than the classic variety, although cases with an aggressive course have been reported.7,8
Lymphangioma-like Kaposi Sarcoma Affecting the Skin: Cases Published to Date.
| Study, y | Clinical Type | Age | Sex | Clinical Lesions | Onset of Kaposi Sarcoma | Distribution of Lesions | Behavior |
|---|---|---|---|---|---|---|---|
| Gange and Jones, 1979 | Classic KS | 82 | W | Blisters | 2 y | Generalized | Slow progression |
| Classic KS | 55 | M | Papules | 3 y | Generalized | Slow progression | |
| Classic KS | 72 | M | Papules | 10 y | Generalized | Slow progression | |
| Leibowitz, 1980 | Endemic KS | 34 | M | Blisters | Unknown | Generalized | Aggressive |
| Davis and Scott, 2000 | KS-AIDS | 35 | M | Macules | 5 y | Generalized | Slow progression |
| Noel et al., 1997 | Endemic KS | 42 | M | Plaques | Unknown | Localized | Slow progression |
| Cossu et al., 1997 | Classic KS | 77 | M | Blisters | 8 y | Localized | Slow progression |
| Classic KS | 71 | W | Blisters | 2 mo | Generalized | Aggressive | |
| Classic KS | 66 | W | Blisters | 3 y | Generalized | Slow progression | |
| Classic KS | 80 | M | Macules | 2 mo | Localized | Slow progression | |
| Classic KS | 75 | M | Papules | 5 y | Localized | Slow progression | |
| Classic KS | 71 | M | Papules | 3 y | Generalized | Slow progression | |
| Classic KS | 59 | M | Macules | 1 mo | Generalized | Slow progression | |
| Roncheses and Kern, 1957) | Classic KS | 68 | M | Blisters | 4 y | Generalized | Slow progression |
| Classic KS | 65 | M | Blisters | Unknown | Generalized | Slow progression | |
| Bossuyt et al., 1995) | KS-AIDS | 57 | M | Nodules | 1 y | Generalized | Slow progression |
| De la Torre et al., 1998) | KS-AIDS | 25 | M | Nodule | Unknown | Generalized | Died 4 mo later |
| Ramírez et al., 2005) | Classic KS | 83 | W | Blisters | 3 y | Legs | Slow progression |
| KS-AIDS | 38 | M | Plaques and nodules | 2 mo | Neck, chest, right arm | Slow progression | |
| Classic KS | 75 | W | Papules | 1 y | Legs | Unknown | |
| KS-AIDS | 40 | M | Papules and plaques | 3 y | Legs | Slow progression | |
| Mohanna et al., 2006) | Classic KS | 65 | M | Blisters | 8 y | Legs and arms | Slow progression |
| Classic KS | 89 | W | Blisters and nodules | 1 mo | Legs | Slow progression | |
| Classic KS | 61 | M | Plaques and nodules | 1 y | Legs | Slow progression | |
| KS-AIDS | 36 | W | Plaques and nodules | 7mo | Legs | Died 2 mo later | |
| Friedman et al., 2013) | Classic KS | 85 | M | Gangrene | 2 wk | Right foot | Slow progression |
| Agustí-Mejías et al., 2011) | Classic KS | 75 | W | Plaque | 8 y | Right leg and arm | Slow progression |
| Present case | Classic KS | 80 | M | Plaques and nodules | 5 y | Legs and back | Slow progression |
Abbreviation: KS; Kaposi sarcoma.
Histologically, the disease is characterized by ectatic vascular spaces with a labyrinthine architecture that dissect collagen bundles and dermal adnexa and are accompanied by a nodular lymphoplasmacytic infiltrate. The vascular structures are lined with flattened endothelial cells with no mitosis and no—or very scant—atypia. The cells of Kaposi sarcoma express endothelial cell markers (CD31 and CD34) and lymphatic markers (D2-40), as well as HHV-8.9 The differential histologic diagnosis should be with other vascular tumors that show an infiltrative growth pattern between the collagen bundles or that comprises spindle cells, as is the case with low-grade angiosarcoma, kaposiform hemangioendothelioma, spindle cell hemangioma, hobnail angioma (targetoid hemosiderotic hemangioma), and benign lymphangioendothelioma.10 The condition can also present as lymphangiectasia, although it is easy to detect this form with histopathology, which reveals dilation of pre-existing lymph vessels and absence of new formations, as occurs in the lymphangiomatous type.
TreatmentLLKS can be systemic or local, depending on the epidemiologic type, the patient's immune status, and the number of lesions. Local treatment can be carried out with liquid nitrogen–based cryotherapy, radiotherapy, laser, or intralesional injections with chemotherapy agents or interferon. Systemic treatment can be administered with interferon or chemotherapy agents.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Martínez-Ortiz F, Avivar MG. Sarcoma de Kaposi de tipo linfangiomatoso. Actas Dermosifiliogr. 2017;108:268–271.