Primary cutaneous CD4+ small/medium-sized T-cell lymphoma (PCSM-TCL) is a rare provisional entity included in the 2005 cutaneous lymphoma classification of the World Health Organization/European Organisation for Research and Treatment of Cancer (WHO/EORTC) in the group of primary cutaneous T-cell lymphomas.1
Our patient was a 44-year-old man with no past history of interest. He was seen for a nodular lesion that had appeared on the left nasal ala 3 weeks earlier and had grown progressively. At the time of consultation, this well-defined, indurated nodular lesion measured 2.5cm in diameter and there were no changes in the overlying skin (Fig. 1). No other cutaneous lesions were observed and there were no palpable lymph nodes or organomegaly.
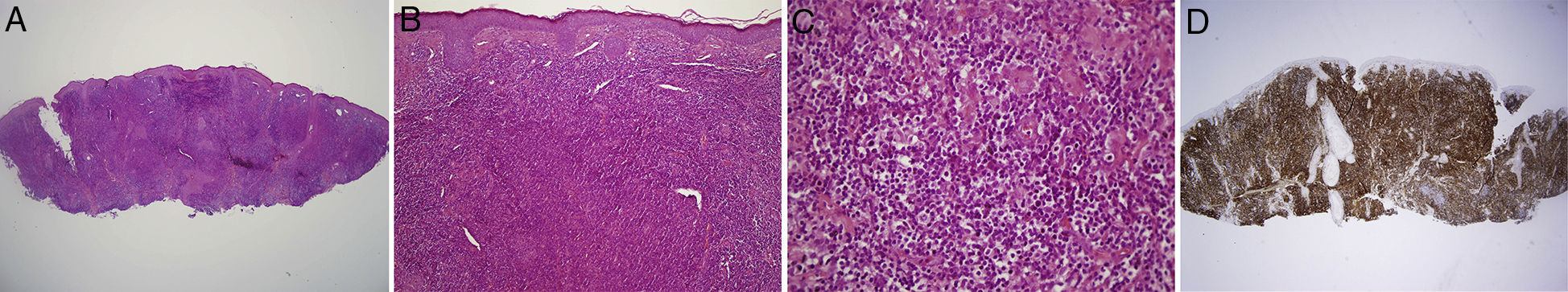
An incisional biopsy revealed a dense, diffuse lymphocytic infiltrate in the dermis. The lymphocyte population was formed of small-sized lymphocytes associated with another population of medium-sized lymphocytes, both populations showing pleomorphism. No discernible germinal centers were found. Epidermotropism was minimal and there was slight infiltration of the follicular epithelium. Immunohistochemistry revealed a lymphocyte population formed predominantly of T cells that expressed CD3 and CD5. The CD4/CD8 ratio was greater than 2 (Fig. 2). Analysis of T-cell receptor rearrangement revealed a monoclonal T-cell population.
A and B, Biopsy showing the dense lymphocytic infiltrate. Hematoxylin-eosin, original magnification ×2 (A) and ×10 (B). C, Detail of the composition of the infiltrate, showing cellular pleomorphism. Hematoxylin–eosin, original magnification ×40. D, Immunohistochemical stain for CD4, original magnification ×2.
Blood tests including complete blood count, routine biochemistry, and lactate dehydrogenase were normal, as was cervical-thoracic-abdominal computed tomography, excluding the involvement of other organs. Based on these findings we made a diagnosis of PCSM-TCL.
Since the first follow-up visit, 10 days after the biopsy, the lesion was seen to regress and it had completely disappeared after 3 months (Fig. 3). In view of the good clinical course, we decided to maintain a wait-and-see approach with frequent follow-up visits. After a year the patient remained asymptomatic and no new lesions had appeared.
PCSM-TCL is included as a provisional entity in the group of primary cutaneous T-cell lymphomas, both in the 2005 WHO/EORTC classification of cutaneous lymphomas and in the latest (2008) classification of tumors of hematopoietic and lymphoid tissue.1,2 It is a rare disease that accounts for approximately 2% to 3% of primary cutaneous lymphomas.1 It affects men and women equally, and the mean age at the time of diagnosis is 50-60 years, though it can arise at any age—published cases range from 3 to 90 years of age.3 Clinical presentation is usually as a solitary, asymptomatic, rapidly growing plaque or mass of up to 3cm diameter; lesions most commonly arise on the face or neck, or on the upper part of the trunk. The surface is typically smooth and may have an erythematous or violaceous appearance.3 There are 2 other forms of presentation with a poorer prognosis, one as an aggressive tumor and the other as multiple lesions with abundant eosinophils observed in the skin biopsy.4,5 The histology of the lesions contrasts with the benign course of PCSM-TCL. Dense, nodular or diffuse infiltrates of atypical, pleomorphic small- and medium-sized lymphocytes are found in the superficial and deep dermis and tend to infiltrate the subcutaneous cellular tissue. Although large pleomorphic cells may be observed, by definition these make up less than 30% of the infiltrate. An inflammatory infiltrate of reactive CD8+ T cells is usually present, as well as a variable number of B cells, plasma cells, macrophages, and eosinophils.6 It is not uncommon to find focal areas of epidermotropism and invasion of adnexal structures. The atypical cells show the following immunohistochemical profile: CD3+, CD4+, CD8–, and CD30–. The proliferation index is less than 30%, and molecular analysis reveals monoclonal rearrangement of the T-cell receptor gene, either of the gamma chain or of the beta chain, in 60% of cases.1–3 In the differential diagnosis, there are no clear criteria to differentiate PCSM-TCL from benign lymphoid diseases, and the nuclear pleomorphism, immunohistochemistry, and detection of clonality are therefore used to orient the diagnosis to PCSM-TCL.3 Five-year survival is over 90% when presentation is with a single lesion with typical characteristics. This prognosis worsens when presentation is multifocal, and overall 5-year survival is of 60% to 80%.1–3 Poor prognostic factors include CD2–, rapidly growing tumors over 5cm in diameter, the presence of a limited number of accompanying CD8+ Tcells and a high ki-67 index.3,7 To date, 3 other cases of spontaneous regression after biopsy have been reported.7–9 The therapeutic options described in the consensus statement on the treatment of cutaneous lymphomas10 suggest non-aggressive management for patients with primary or recurrent, single or multiple localized nodular forms, varying from follow-up of the patient to topical or intralesional corticosteroids or even surgery or radiation therapy. Treatment for aggressive forms must be individualized according to the characteristics of the patient.
Please cite this article as: González Fernández D, Valdés Pineda F, Gómez Díez S, Vivanco Allende B. Linfoma primario cutáneo T CD4 positivo de linfocitos de pequeño y mediano tamaño con regresión espontánea tras la biopsia. Actas Dermosifiliogr. 2015;106:767–768.