Necrobiosis lipoidica (NL) is a granulomatous disease of unknown etiology that typically occurs in diabetic patients. It is characterized by sclerotic plaques that most often appear on the legs.
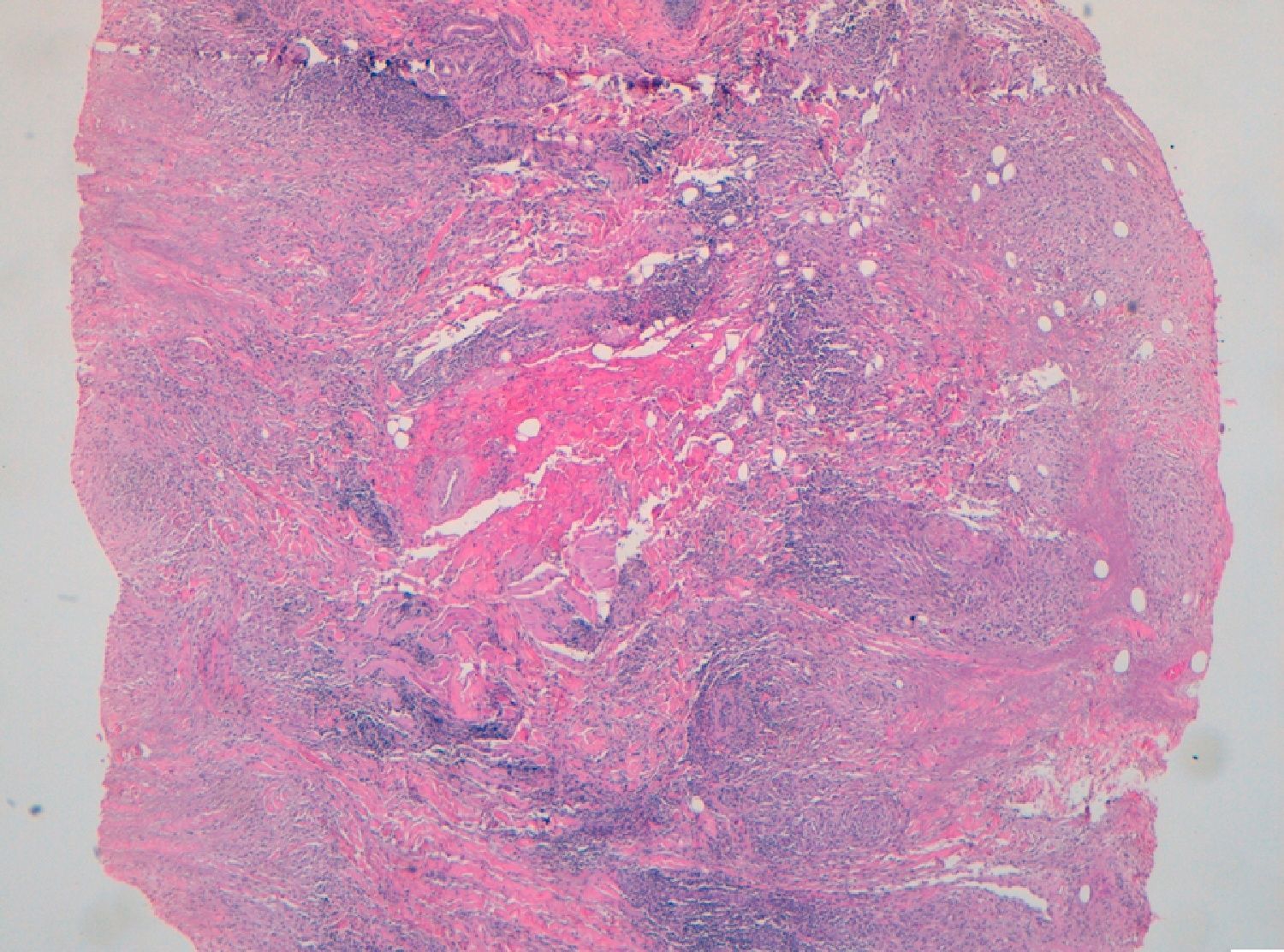
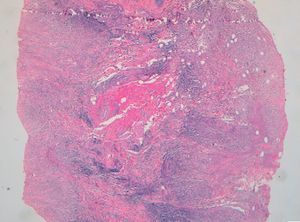
A 15-year-old girl was admitted to our hospital with facial lesions that had appeared 5 months earlier. She had previously consulted with a surgeon who had suggested surgical excision of the lesions. Physical examination revealed yellowish nodules and plaques with superficial telangiectasias on the upper and lower eyelids of the left eye (Fig. 1). The patient had been diagnosed with type 1 diabetes mellitus at age 6 years and had a history of marked insulin resistance and chronic poor blood glucose control (hemoglobin A1c, 13%). Skin biopsy revealed an inflammatory infiltrate in the reticular dermis and hypodermis, predominantly composed of histiocytes that had aggregated to form granulomas surrounded by degenerated collagen fibers. Other findings included extracellular lipid deposits and no increase in stromal mucin. Plasma cells and multinucleated giant cells were also observed (Fig. 2). A diagnosis of NL was established on the basis of clinical and histologic findings and the patient's past history. Because the site of the skin lesions made the use of topical or intralesional corticosteroids inadvisable, treatment was started with twice daily applications of 0.1% tacrolimus ointment. After 2 months of treatment with no improvement, oral pentoxifylline (600mg/12 h) was added but was subsequently discontinued owing to gastrointestinal intolerance. When the lesions had resolved only partially after 4 months of treatment, topical tacrolimus was replaced with acetylsalicylic acid (300mg/d). After a further 10 weeks of treatment, the periocular plaques had clearly improved, but other plaques of NL, including 1 with ulceration, appeared in the pretibial region. The pretibial plaques were treated with intralesional corticosteroids and hyperbaric oxygen therapy and resolved almost completely. After 2 years of treatment with acetylsalicylic acid, the periocular lesions had decreased in size until only a few small, infiltrated, slightly erythematous plaques remained. Ten months after withdrawal of the treatment, the plaques had not increased in size.
NL is 3 times more common in women than in men, with the age of onset usually between 30 and 40 years. It is often associated with type 1 diabetes mellitus; between 75% and 90% of patients with NL have or will develop diabetes, although NL is present in only 0.3% to 3% of diabetic patients. NL has also been associated with autoimmune thyroid disease, rheumatoid arthritis, inflammatory bowel disease, and sarcoidosis.
Although NL lesions are typically located on the anterior and lateral aspects of the legs, cases affecting the trunk, upper limbs, face, and penis have also been described. NL lesions in the periocular region are extremely rare, but they have been found both in isolation1 and in association with NL lesions in other areas.2
The lesion begins as an erythematous papule or plaque, which extends peripherally, developing a yellowish atrophic center and a raised erythematous border. The main complication of NL is ulceration, which occurs in 25% to 33% of patients. Atypical lesions on the face and the edge of the scalp have been described3–5 in association with Miescher granuloma, actinic granuloma, granuloma multiforme, and necrobiotic xanthogranuloma.6
NL is histologically characterized by a normal or atrophic—and frequently ulcerated—epidermis and necrobiotic collagen with sclerosis. In the dermis, palisading granulomas arranged in layers parallel to the epidermis can be observed. The dermal inflammatory infiltrate is composed of histiocytes, multinucleated giant cells, lymphocytes, and plasma cells. The histopathological differential diagnosis must primarily rule out granuloma annulare, rheumatoid nodules, and necrobiotic xanthogranuloma.
In cases with periorbital involvement it is essential to rule out the possibility of necrobiotic xanthogranuloma, a form of histiocytosis associated with paraproteinemia that usually occurs in periorbital sites. This disorder manifests as yellowish-red indurated nodules or plaques, frequently with atrophy, ulceration, and telangiectasias. Histologically, necrobiotic xanthogranuloma is differentiated from NL by its denser infiltrate of histiocytes, more pronounced inflammation and more severe degeneration of the subcutaneous cell tissue, and the presence of foamy histiocytes, Touton giant cells, bizarre foreign-body giant cells, and cholesterol clefts.7
NL is treated for cosmetic reasons or to avoid ulceration and the risk of secondary infection and deep tissue destruction. Topical and intralesional corticosteroids are the drugs most widely used to treat NL. Other drugs that have been used include acetylsalicylic acid, ticlopidine, pentoxifylline, tretinoin, clofazimine, mycophenolate mofetil, tumor necrosis factor (TNF) inhibitors, ciclosporin, thalidomide, fumaric acid esters, hydroxychloroquine, niacinamide, photodynamic therapy,8 psoralen–UV-A,9 and topical tacrolimus.10 Blood glucose control and treatment for diabetes do not appear to have any beneficial effect on NL lesions. Surgical excision of the affected area can ensure resolution of the lesions but may also lead to considerable cosmetic and functional sequelae in the case of periorbital lesions.
In conclusion, when NL lesions occur in atypical sites, a high index of suspicion is required if we are to avoid misdiagnoses and inappropriate treatment decisions. Although it was only partially effective in the case of our patient, topical tacrolimus appears to be effective and particularly safe for the treatment of periocular NL lesions.
Please cite this article as: G. Pitarch, Giner F. Necrobiosis lipoidica periorbitaria. Actas Dermosifiliogr. 2013;104:636–8.