Bone marrow involvement at the time of diagnosis is uncommon in patients with primary cutaneous marginal zone B-cell lymphoma (PCMZL). Moreover, in these patients such involvement is rarely found in isolation on diagnosis. Typically the few patients with PCMZL who have early bone marrow involvement also present secondary nodal or visceral involvement, which is detected by other staging studies (usually computed tomography). In recent years, this has given rise to some debate about whether a bone marrow biopsy should be routinely performed in patients diagnosed with PCMZL in view of the good prognosis and low incidence of bone marrow infiltration and/or extracutaneous involvement in this type of lymphoma.
En los pacientes con linfoma primario cutáneo de células B de la zona marginal (LPCBZM), la afectación de la médula ósea en el momento del diagnóstico es poco frecuente. Además, es raro en estos pacientes detectar afectación de la médula ósea al diagnóstico de forma aislada. Los pocos casos de LPCBZM y afectación inicial de la médula ósea habitualmente presentan también afectación secundaria nodal o visceral que son detectadas con otras pruebas de estadificación (normalmente con la TAC). Por dicho motivo, en los últimos años ha sido tema de controversia si debe realizarse la biopsia de médula ósea al diagnóstico de forma sistemática en todos los casos de LPCBZM dado el buen pronóstico y la baja incidencia de infiltración medular y/o afectación extracutánea por parte de este tipo de linfoma.
Primary cutaneous marginal zone B-cell lymphoma (MZL), or extranodal MZL of the mucosa-associated lymphoid tissue (MALT) type, is an indolent B-cell lymphoma that first manifests on the skin with no extracutaneous involvement at the time of diagnosis. It is one of the main subtypes of cutaneous B-cell lymphoma.1,2 Clinically, primary cutaneous MZL presents as isolated or multiple infiltrated plaques or nodules that are often found on the trunk or proximal part of the extremities (Fig. 1). These lymphomas affect middle-aged patients and tend to be somewhat more frequent in men. Although this tumor has an indolent course and is usually confined to the skin, relapses are common at the initial sites, distant sites, or both. In very rare cases, extracutaneous involvement is seen at diagnosis or during the course of the disease; other MALT sites (digestive tract, salivary glands, thyroid, breast, lung, and orbit), lymph nodes, or bone marrow may be affected. Nevertheless, prognosis is generally excellent, with a 5-year survival rate close to 100%.3–7
Staging of Primary Cutaneous MZLIn order to rule out potential systemic disease, the initial workup in suspected primary cutaneous MZL should include a clinical history and meticulous physical examination (detection of B symptoms, complete skin inspection, and palpation of lymph nodes and viscera). The staging study should include a laboratory workup with peripheral blood smear (formula and count), standard biochemical profile with levels of lactate dehydrogenase and β2-microglobulin, and serological tests for hepatitis C virus, human herpesvirus 8, cytomegalovirus, Epstein-Barr virus, and Borrelia burgdorferi. A computed tomography scan of the thorax, abdomen, and pelvis should be performed. Pioneering studies in this field also proposed systematic inclusion of bone marrow biopsy in the initial staging.6
Bone Marrow BiopsyBone marrow biopsy is an invasive diagnostic technique in which a small fragment of bone containing a small amount of bone marrow is extracted with a needle. The procedure is generally performed by hematologists, who usually take the sample from the iliac crest. Although local anesthesia is applied, the procedure is uncomfortable and may occasionally be painful. In some cases, the physician has to exert strong pressure when inserting the needle, and the patient may momentarily feel pain when the needle crosses the bone. The patient may also feel discomfort or pain in the general area, although this usually eases within a few hours with the help of ordinary analgesics. Other side effects include hematoma or bleeding at the puncture site and risk of local or bone infection, which is very unusual today given that the procedure is performed under aseptic conditions. Histologically, extranodal MZL does not have a specific pattern of infiltration, and nodular, interstitial, paratrabecular, diffuse, or sinusoidal patterns can be observed. The fact that a median of 5% of the medullary space is infiltrated by extranodal MZL sometimes creates a diagnostic challenge for the pathologist.8–10
Unlike splenic and nodal MZL, which tend to infiltrate bone marrow in 67% to 100% and 30% to 40% of cases, respectively, extranodal MZL infiltrates bone marrow much less commonly (in around 10% of cases).8
Primary Cutaneous MZL and Bone Marrow Involvement at DiagnosisBone marrow involvement is uncommon at the time of diagnosis of primary cutaneous MZL. Moreover, in patients with this lymphoma, bone marrow is rarely the only tissue affected at diagnosis, and in the few cases in which early bone marrow involvement is found, patients usually also have secondary nodal or visceral disease, which is detected using other staging studies (usually computed tomography). Therefore, the need for bone marrow biopsy at diagnosis in all cases of suspected primary cutaneous MZL has lately come under debate. In a consensus proposal from the Cutaneous Lymphoma Task Force of the European Organization for Research and Treatment of Cancer (EORTC) and the International Society of Cutaneous Lymphomas, Kim et al.11 proposed a new TNM classification for primary cutaneous lymphomas other than mycosis fungoides and Sézary syndrome. The report also listed recommended tests for initial staging of these lymphomas (Table 1). Of note, the proposal considers bone marrow biopsy essential in cases of lymphoma with a risk of extracutaneous dissemination and intermediate or aggressive behavior according to the World Health Organization (WHO)-EORTC classification (Table 2) (natural killer lymphoma; CD8+ T-cell lymphoma; γ/δ T-cell lymphoma; and diffuse large B-cell lymphoma, leg type). In contrast, in slow-growing lymphomas, including primary cutaneous MZL, primary cutaneous follicle center lymphoma (FCL), and CD30+T-cell anaplastic lymphoma, bone marrow biopsy is considered an option, unless the results of other staging tests are positive. After an exhaustive review of the literature, we found that very few articles12–15 specifically address bone marrow involvement at diagnosis in primary cutaneous MZL and that even fewer address the issue of whether bone marrow biopsy should be performed routinely in cases of primary cutaneous MZL. We found confirmation of the low frequency of early bone marrow involvement in primary cutaneous MZL12–14 and suggest that routine bone marrow biopsy would not be justified in the initial workup for these lymphomas. The most relevant article in this respect is that of Senff et al.,12 who reviewed 275 bone marrow biopsy results (193 primary cutaneous FCL and 82 primary cutaneous MZL) and found that the marrow was affected at diagnosis in 22 cases of primary cutaneous FCL (11%) and that this was the only sign of extracutaneous dissemination in only 9 of them. A positive bone-marrow biopsy was found in only 2 cases of primary cutaneous MZL (2%), and in only 1 of these cases was bone marrow involvement the only extracutaneous sign. However, other guidelines, including those of the Dutch-Belgian Hemato-Oncology Group, maintain bone marrow biopsy as part of routine staging in all patients with non-Hodgkin lymphoma.16 The criteria for performing bone marrow biopsy vary among the different clinical guidelines of the working groups. The literature suggests that a bone marrow biopsy is ordered by most groups (as reported in papers from the Netherlands,3 Italy,5 and Austria17) although these studies were performed before the 2007 consensus paper.11 On the other hand, Gerami et al.,4 from Chicago in the United States, reviewed 30 cases of primary cutaneous MZL and found that bone marrow biopsy was only performed in half.
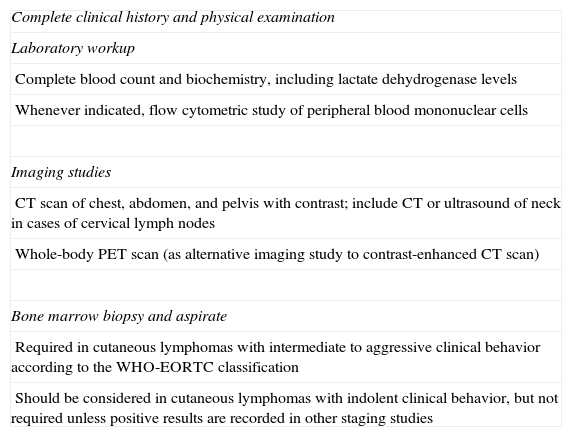
ISCL/EORTC Recommendations on Initial Staging in Cutaneous Lymphomas Other Than Mycosis Fungoides/Sézary Syndrome.
| Complete clinical history and physical examination |
| Laboratory workup |
| Complete blood count and biochemistry, including lactate dehydrogenase levels |
| Whenever indicated, flow cytometric study of peripheral blood mononuclear cells |
| Imaging studies |
| CT scan of chest, abdomen, and pelvis with contrast; include CT or ultrasound of neck in cases of cervical lymph nodes |
| Whole-body PET scan (as alternative imaging study to contrast-enhanced CT scan) |
| Bone marrow biopsy and aspirate |
| Required in cutaneous lymphomas with intermediate to aggressive clinical behavior according to the WHO-EORTC classification |
| Should be considered in cutaneous lymphomas with indolent clinical behavior, but not required unless positive results are recorded in other staging studies |
Abbreviations: CT, computed tomography; EORTC, European Organization for Research and Treatment of Cancer; ISCL, International Society of Cutaneous Lymphomas; PET, positron emission tomography; WHO, World Health Organization.
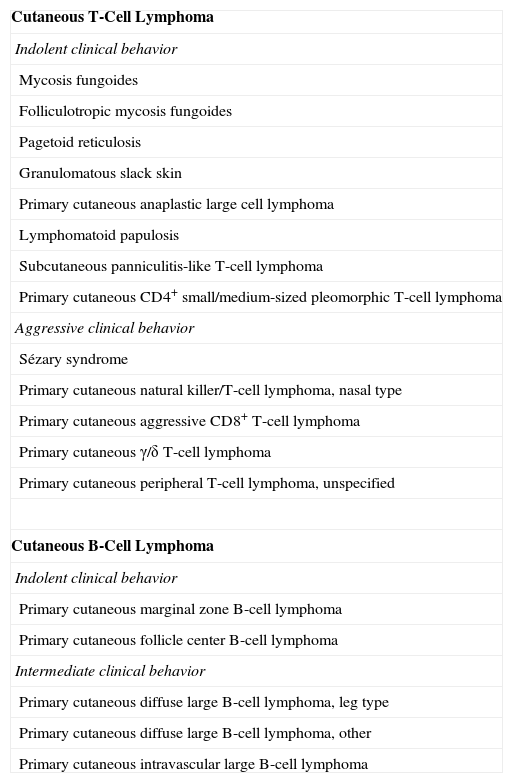
WHO-EORTC Classification of Primary Cutaneous Lymphomas.
| Cutaneous T-Cell Lymphoma |
| Indolent clinical behavior |
| Mycosis fungoides |
| Folliculotropic mycosis fungoides |
| Pagetoid reticulosis |
| Granulomatous slack skin |
| Primary cutaneous anaplastic large cell lymphoma |
| Lymphomatoid papulosis |
| Subcutaneous panniculitis-like T-cell lymphoma |
| Primary cutaneous CD4+ small/medium-sized pleomorphic T-cell lymphoma |
| Aggressive clinical behavior |
| Sézary syndrome |
| Primary cutaneous natural killer/T-cell lymphoma, nasal type |
| Primary cutaneous aggressive CD8+ T-cell lymphoma |
| Primary cutaneous γ/δ T-cell lymphoma |
| Primary cutaneous peripheral T-cell lymphoma, unspecified |
| Cutaneous B-Cell Lymphoma |
| Indolent clinical behavior |
| Primary cutaneous marginal zone B-cell lymphoma |
| Primary cutaneous follicle center B-cell lymphoma |
| Intermediate clinical behavior |
| Primary cutaneous diffuse large B-cell lymphoma, leg type |
| Primary cutaneous diffuse large B-cell lymphoma, other |
| Primary cutaneous intravascular large B-cell lymphoma |
Abbreviations: EORTC, European Organization for Research and Treatment of Cancer; WHO, World Health Organization.
In patients with primary cutaneous MZL, not performing a bone marrow biopsy has very limited clinical consequences. If a patient with MZL has skin lesions at the time of initial staging (including those who have had a negative bone marrow biopsy), then the disease would be classed as primary cutaneous MZL according to the WHO-EORTC classification. However, if a distant tumor can be identified in the bone marrow biopsy or at another phase of staging, the classification would change to extranodal MZL with initial presentation on the skin and the corresponding MALT lymphoma. Lastly, if we do not perform a bone marrow biopsy and the other staging study results are negative, then, from a terminological point of view, we cannot class the disease as primary cutaneous MZL, but rather as extranodal MZL with skin lesions. Although the classification changes, the disease would still be considered slow-growing lymphoma, and treatment and prognosis would not vary substantially. Treatment of extranodal MZL with skin lesions and isolated involvement of the marrow is no different from that of primary cutaneous MZL. The treatment of choice in both cases is local radiotherapy delivered to the skin, although patients with extranodal MZL are more closely followed.12
Furthermore, if, by definition, primary cutaneous MZL is limited to the skin at diagnosis, then diagnosis must be confirmed by staging study in order to rule out the presence of systemic lymphoma with secondary cutaneous manifestations. Consequently, if bone marrow biopsy is no longer to be routinely performed in these cases, then we cannot confirm a diagnosis of the primary cutaneous form, thus making it difficult to identify the pathogenetic differences between the different types of MALT lymphoma by localization, in terms of the translocations and antigenic stimuli involved in their development.
ConclusionIn our opinion, bone marrow biopsy is necessary for the diagnosis and classification of cutaneous lymphoma from a theoretical viewpoint; from a clinical viewpoint, however, its contribution is limited, and, if it is not performed, very few cases with isolated involvement of bone marrow would go undiagnosed. We believe that more prospective studies with larger populations are necessary to explore the significance of isolated bone marrow involvement in patients diagnosed with primary cutaneous MZL, including the therapeutic implications and prognosis of this finding. Further study would allow us to decide whether routine bone marrow biopsy is or is not necessary in this type of lymphoma.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Data protectionThe authors declare that they followed their hospital's regulations regarding the publication of patient information and that written informed consent for voluntary participation was obtained for all patients.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Muniesa C, Hernández-Machín B. ¿Está siempre indicada la biopsia de médula ósea en los pacientes con linfoma primario cutáneo de células B de la zona marginal? Actas Dermosifiliogr. 2013;104:667–71.