An 80-year-old man visited our department with asymptomatic skin lesions that had appeared 2 months earlier. The patient stated that he was not receiving any regular treatments and had not been administered new drugs; he reported no fever or other symptoms and did not recall having been bitten or stung.
Physical examination revealed erythematous papules on the upper part of the torso; the papules measured approximately 3mm in diameter and were firm with a depressed center (Figs. 1 and 2). Some of the papules had coalesced to form plaques. The mucosa, palms, and soles were not affected.
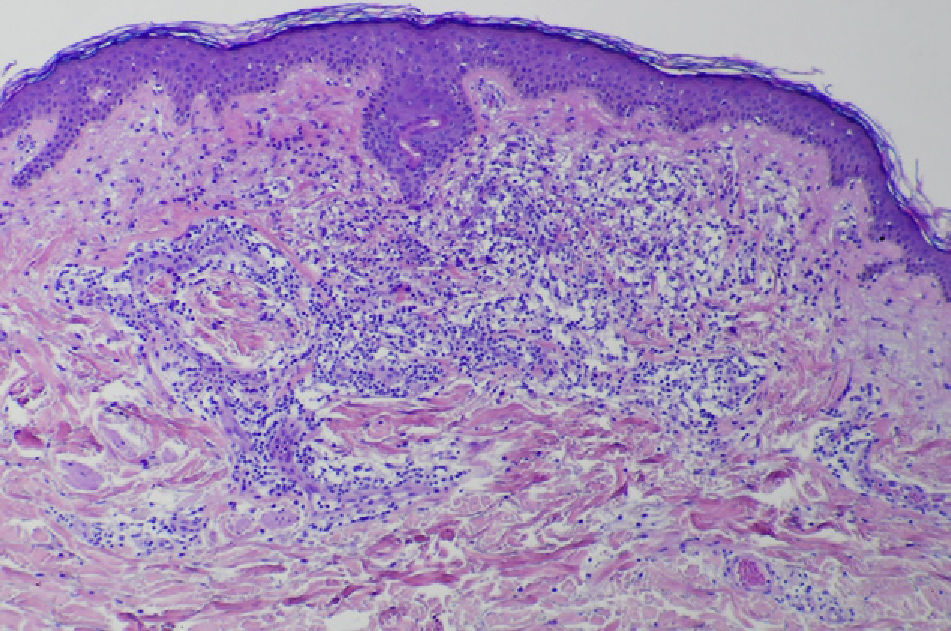
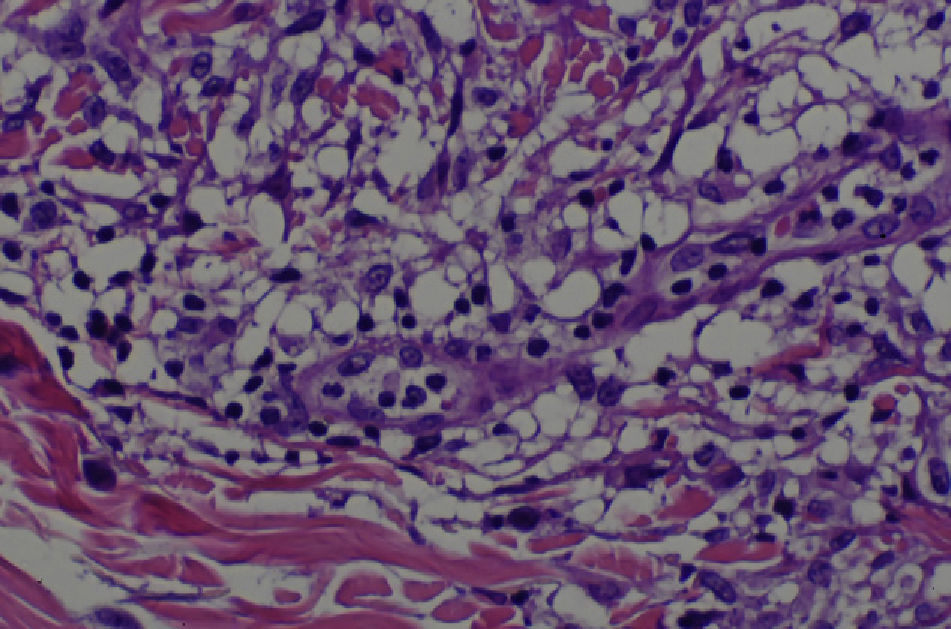
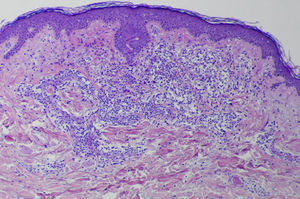
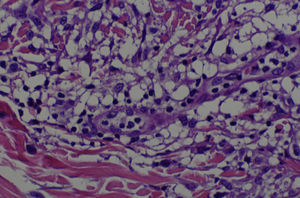
A skin biopsy revealed a dense infiltrate in the papillary and middle dermis, consisting mainly of histiocytes, some of which were vacuolated, lymphocytes, and some multinucleated giant cells (Figs. 3 and 4). Immune staining was positive for CD68 and negative for S100, CD1a, and factor XIIIa.
Laboratory tests and x-ray studies showed only monocytosis, which had already been diagnosed and was being followed up by the hematology department after a diagnosis of chronic myelomonocytic leukemia with limited bone marrow dysplasia and a normal karyotype.
The patient was diagnosed with generalized eruptive histiocytosis and a wait-and-see approach was adopted; the lesions disappeared 6 months after diagnosis. The chronic myelomonocytic leukemia has remained stable to date.
Histiocytosis comprises a rare, heterogeneous group of diseases characterized by the proliferation of histiocytes. Most authors continue to use the traditional classification of the entity into Langerhans cell histiocytosis, type I histiocytosis or histiocytosis X, and non-Langerhans cell, type II, or non-X histiocytosis.
The group of non-Langerhans cell histiocytoses includes multiple diseases, such as generalized eruptive histiocytosis. Some authors maintain that these are not independent diseases but are different stages in the course of the same disease, and that generalized eruptive histiocytosis is the initial stage of the process, with subsequent development of xanthomatous lesions.1
In 1963, Winkelmann and Muller2 described generalized eruptive histiocytosis as a rare condition characterized by multiple noncoalescing, symmetric erythematous papules distributed on the torso and limbs. The disease is not accompanied by extracutaneous involvement and histology shows a monomorphic infiltrate consisting predominantly of histiocytes that are negative for S100 and lipids. The disease has a benign course and mainly affects middle-aged patients. It tends to remit spontaneously and, although the cause has not been established, some authors maintain that it is produced by the apoptosis mechanism.3
In our patient, the differential diagnosis included generalized granuloma anulare, which was ruled out, and immune staining indicated a diagnosis of a type of non-Langerhans cell histiocytosis. The clinical appearance of the lesions, their location, and the patient's age at onset ruled out other types non-Langerhans cell histiocytosis, such as benign cephalic histiocytosis, multicentric reticulohistiocytosis, and progressive nodular histiocytoma. The principal differential diagnosis includes other forms of xanthomatous non-Langerhans cell histiocytosis, particularly adult papular xanthoma. Adult papular xanthoma may be a later stage in the development of the disease, in which the clinical lesions take on a yellowish color and are characterized histologically by a greater number of xanthomatous cells.4
A wait-and-see approach is usually adopted, as the condition tends to resolve spontaneously within a few months. Treatment should be considered when remission does not occur and good results have been reported for systemic treatment with corticosteroids, hydroxychloroquine, and thalidomide,5 with psoralen-UVA6 or even cryotherapy, peeling, or carbon dioxide laser treatment in localized lesions.1
Our patient presented 3 unique aspects: coalescence of the lesions, negative immune staining for factor XIIIa, and association with chronic myelomonocytic leukemia.
Coalescence of the lesions has been reported in the late stage of this disease. Klemke et al.7 linked this clinical sign in this type of histiocytosis with acute monocytic leukemia and with a worse prognosis for the disease. Hence, the coalescence of the lesions in our patient and the myelomonocytic leukemia support this observation.
Another characteristic of our patient is the negative immune staining for factor XIIIa, which is usually positive in generalized eruptive histiocytosis; 2 other cases have been reported in the literature with this characteristic.6,8
In general, non-Langerhans cell histiocytosis presents a benign course in healthy patients and does not usually appear in association with malignant diseases. However, some types of non-Langerhans cell histiocytosis, such as progressive nodular histiocytosis and juvenile xanthogranuloma, have been described in association with hematologic disorders.9 To date, 2 cases have been reported in the literature of generalized eruptive histiocytosis associated with acute monocytic leukemia,7,10 but none have been described in association with chronic myelomonocytic leukemia, as was the case with our patient.
In conclusion, we report what we believe to be the first case of a patient with generalized eruptive histiocytosis associated with chronic myelomonocytic leukemia. In our opinion, given the frequency of hematologic disorders in patients with non-Langerhans cell histiocytosis, further study of this association is needed in patients with these signs and symptoms, and more specifically, in patients with generalized eruptive histiocytosis with coalescing lesions.
Please cite this article as: Montero I, Gutiérrez-González R, Ginarte M, Toribio J. Histiocitosis eruptive generalizada en paciente con leukemia mielomonocítica crónica. Actas Dermosifiliogr. 2012;103:643–644.