Bortezomib is a proteasome inhibitor used in hematologic malignancies such as multiple myeloma (MM).1 We present 2 patients who developed Sweet-like lesions following the administration of bortezomib and suggest that this is a specific cutaneous manifestation associated with this treatment.
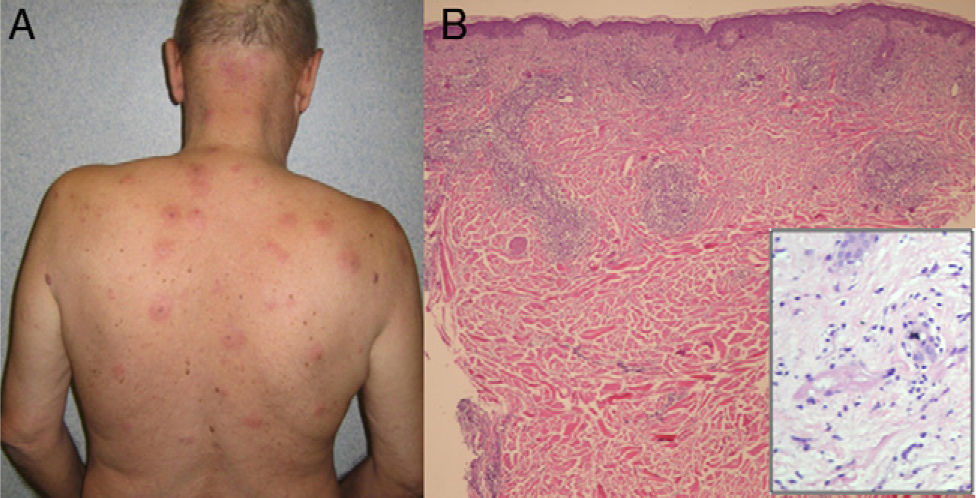
The first patient was a 63-year-old man with a 3-year history of MM who had previously been treated with different chemotherapy regimens and undergone autologous hematopoietic stem cell transplant. On detection of disease recurrence, he was started on treatment with bortezomib. At the time, he was also receiving enalapril. On completion of the first cycle of bortezomib, the patient developed multiple painful erythematous, edematous plaques with a central purple area (Fig. 1A); the plaques became more marked after the second cycle.
The second patient was a 57-year-old man with a 9-year history of MM for which he had been treated with different chemotherapy regimens and undergone 2 autologous hematopoietic stem cell transplants. He was started on bortezomib following relapse of his MM. Omeprazole was the only concomitant medication. Two months later, he developed painful plaques and nodules with an edematous, erythematous-purple appearance on the upper trunk.
Neither of the patients had had fever or any other systemic symptoms. Laboratory results (complete blood count, C-reactive protein [CRP] levels, and erythrocyte sedimentation rate) were normal in both cases.
Skin biopsy showed a diffuse, mixed leukocytic infiltrate involving the full thickness of the dermis, in addition to leukocytoclasia and vasculitis (Fig. 1B). Immunohistochemical staining for CD138, CD79a, and CD68 was negative. Both patients were treated with oral prednisone (40mg/d for 2 weeks) and the lesions disappeared. To prevent recurrence, it was decided to pretreat the patients with oral prednisone (0.5mg/kg/d for 5 days) before the administration of bortezomib in subsequent cycles. No new skin lesions appeared in either patient. The MM progressed in both cases, however, leading to the replacement of bortezomib with lenalidomide and dexamethasone. Unfortunately, both patients died several months later.
To establish the diagnosis of a drug-induced dermatosis in MM, it is first necessary to rule out cutaneous infiltration by the underlying hematologic disease. Different skin reactions have been reported in association with bortezomib, including erythema multiforme, vasculitis, Sweet syndrome, and histiocytoid Sweet syndrome.2–6 These reactions generally have similar clinical and histologic features,7 and symptoms usually appear within days of treatment initiation and increase with each new cycle of treatment. Fever is almost never observed and laboratory findings tend to be normal. Between 8% and 18% of patients develop skin rash.1 Although MM is slightly more common in men than in women (ratio of 1.4:1), Sweet-like lesions have only ever been reported in men.8 The lesions are described as acute, monomorphic eruptions consisting of painful edematous and/or erythematous macules, papules, or plaques that mainly affect the neck and upper third of the trunk. They clinically resemble the plaques seen in Sweet syndrome,1–5,9,10 but can be distinguished by the absence of other systemic features (fever, elevated CRP levels, and neutrophilia) and by certain histologic features (evidence of vasculitis in many cases and absence of a neutrophilic infiltrate) (Table 1).1,2 For this reason, it is preferable to call them Sweet-like lesions. The detection of immune complex deposits by direct immunofluorescence would further support the theory that vasculitis has a role in the etiology and pathology of this entity.11
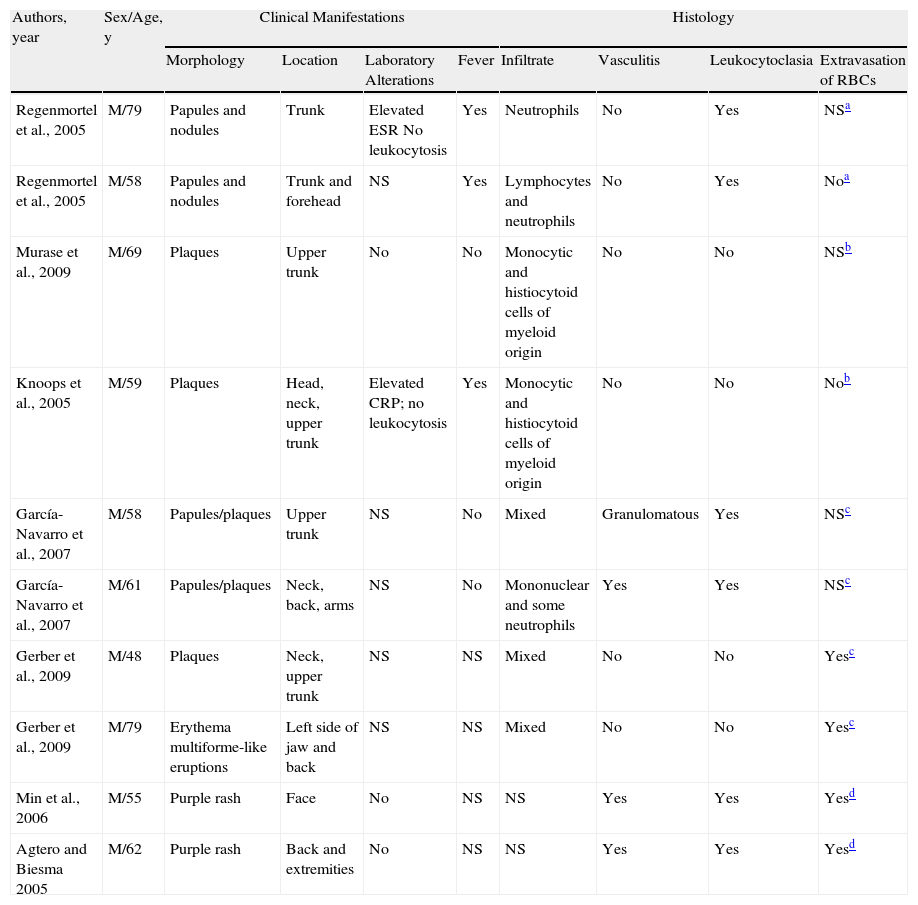
Reactions Attributed to Treatment With Bortezomib in Patients With Multiple Myeloma.
| Authors, year | Sex/Age, y | Clinical Manifestations | Histology | ||||||
| Morphology | Location | Laboratory Alterations | Fever | Infiltrate | Vasculitis | Leukocytoclasia | Extravasation of RBCs | ||
| Regenmortel et al., 2005 | M/79 | Papules and nodules | Trunk | Elevated ESR No leukocytosis | Yes | Neutrophils | No | Yes | NSa |
| Regenmortel et al., 2005 | M/58 | Papules and nodules | Trunk and forehead | NS | Yes | Lymphocytes and neutrophils | No | Yes | Noa |
| Murase et al., 2009 | M/69 | Plaques | Upper trunk | No | No | Monocytic and histiocytoid cells of myeloid origin | No | No | NSb |
| Knoops et al., 2005 | M/59 | Plaques | Head, neck, upper trunk | Elevated CRP; no leukocytosis | Yes | Monocytic and histiocytoid cells of myeloid origin | No | No | Nob |
| García-Navarro et al., 2007 | M/58 | Papules/plaques | Upper trunk | NS | No | Mixed | Granulomatous | Yes | NSc |
| García-Navarro et al., 2007 | M/61 | Papules/plaques | Neck, back, arms | NS | No | Mononuclear and some neutrophils | Yes | Yes | NSc |
| Gerber et al., 2009 | M/48 | Plaques | Neck, upper trunk | NS | NS | Mixed | No | No | Yesc |
| Gerber et al., 2009 | M/79 | Erythema multiforme-like eruptions | Left side of jaw and back | NS | NS | Mixed | No | No | Yesc |
| Min et al., 2006 | M/55 | Purple rash | Face | No | NS | NS | Yes | Yes | Yesd |
| Agtero and Biesma 2005 | M/62 | Purple rash | Back and extremities | No | NS | NS | Yes | Yes | Yesd |
Abbreviations: CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; M, male; NS, not specified; RBCs, red blood cells.
In our patients there was a temporal relationship between the start of treatment and the onset of the lesions, but the cases did not meet the diagnostic criteria proposed by Walker and Cohen for drug-induced Sweet syndrome or those proposed by Su and Lui for classic Sweet syndrome. The immunohistochemical studies ruled out histiocytoid Sweet syndrome. Based on the above, we consider that our patients developed Sweet-like lesions associated with bortezomib.
Histology findings suggest that the process underlying Sweet-like lesions might consist of vasculitis of variable intensity.1,2 Proinflammatory cytokines that induce the chemotactic migration of neutrophils and other inflammatory cells towards the skin might also have an important role and would explain the good response to corticosteroids.1–3 It is unknown why this mixed inflammatory infiltrate tends to affect the dermis. Bortezomib-induced skin lesions similar to those seen in Sweet syndrome might be due to indirect skin damage rather than to direct drug-induced damage. Furthermore, it has been suggested that their presence might be a marker of good treatment response in other hematologic malignancies in which bortezomib is used (e.g., non-Hodgkin lymphoma); their prognostic value in MM, however, is uncertain.1,2 Systemic corticosteroids appear to be useful both for treating existing skin lesions and preventing new lesions in future treatment cycles.
In conclusion, when treating a patient with MM who develops Sweet-like cutaneous plaques following initiation of treatment with bortezomib, it is important to consider both clinical and histologic features in the differential diagnosis. In the absence of fever and abnormal laboratory test results and in the presence of a mixed infiltrate without histiocyte-like cells, the correct diagnosis would be Sweet-like lesions induced by bortezomib.
Please cite this article as: Truchuelo M, et al. Lesiones Sweet-like inducidas por bortezomib: presentación de 2 casos y revisión de la literatura. Actas Dermosifiliogr. 2012;103:829-31.